How Often Should You Get Bloodwork Done?
How often should you get bloodwork done?
When it comes to bloodwork, many patients believe in a one-size-fits-all approach. Having labs ordered during their annual physical is enough, they think.
Well, not quite.
As much as we’d love a simple solution, health and medicine are seldom so straightforward. How often you should get bloodwork done, and which specific tests your physician orders, depends on your unique circumstances.
Most of us have heard of Elizabeth Holmes and her organization, Theranos. Holmes was a young, charismatic entrepreneur who promised to revolutionize medicine by introducing a personal device that would allow hundreds of tests to be run from a single finger prick.
In reality, the device never existed, and Elizabeth will spend the next 11 years in prison for fraud. The rest of us can watch a version of her story on Hulu.
I was an early skeptic of her theories — not the technology per se, but the fundamental premise that more testing in the hands of more people without medical supervision would make the world a healthier place.
Call me old-fashioned, but I believe the cognitive process of lab testing should intimately involve a healthcare provider. Medicine itself is a scientific endeavor, and at the core of all science is the scientific method: generate a hypothesis (a clinical question) and test it (gather data to try to answer your question).
For example, a diagnostic hypothesis of a fatigued person could generate lab tests to address the source of the fatigue. These might include blood count, hormone balance, etc., but all tests would align with the question we’re trying to answer — why is this person fatigued?
This is one of many strong arguments for why medical testing should always happen under the supervision of a trained professional — and why the question “How often should you get bloodwork done?” is answered, “It depends.”
Blood Test Categories
I like to separate diagnostic lab work into three categories. Defining and exploring these categories demonstrates the importance of medical supervision and how testing regimens can vary among individuals.
Category #1: Symptom-Generated
This category of bloodwork is symptom-directed, and physicians order it to answer a predefined clinical question — i.e. to determine the cause of a specific symptom, such as fatigue or chronic pain.
Someone who experiences right upper quadrant pain, for example, would get tests such as a liver function test.
Category #2: Screening Tests
Screening tests are more open-ended, but should still to an extent be guided by a hypothesis. Tests in this category are chosen based on a patient’s individual risk factors.
If a patient were overweight, we’d test their blood sugar levels to monitor their risk for diabetes. If a patient were on a drug like Protonix, they may be at risk for malabsorption of vitamins such as B12, so we’d want to check their B12 levels. As people age, their organs slowly lose function, so we test kidney function and blood count in older patients. Etc., etc.
Category #3: Disease Management
If a patient has an illness or chronic condition, they need more frequent lab testing to monitor their treatment.
The regularity of testing depends on the specific disease and treatment. For example, some illnesses, like thyroid disease, can be treated with hormone therapies, which need to be monitored frequently.
How Often Should You Get Bloodwork Done?
As I mentioned, it depends on the category and goal of the test.
Symptom-generated testing must happen as soon as symptoms occur. This type of testing isn’t required on a regular basis.
Screening tests are typically done annually because it’s convenient to tack them onto your annual physical. However, if your risk factors justify more frequent testing, consult your doctor to come up with an individualized testing schedule.
In my experience, testing for disease management usually occurs every 90 days (three months). It’s a common interval — A1C testing measures the average blood sugar over 90 days, finding equilibrium after adjusting thyroid medication usually takes 90 days, and adjusting to a new dosage of a cholesterol pill takes about three months.
Preparing for Labs
Many people think they need to fast before going for lab testing. That’s not the case at all. In fact, there are very few labs that necessitate fasting.
Only blood sugar (blood glucose) and cholesterol tests require fasting. However, technology has advanced enough that we can work around fasting for those tests — we understand some people can’t fast or have difficulty fasting.
In place of LDL cholesterol, we can order a more sophisticated test called an apolipoprotein B, which doesn’t require fasting. And for blood glucose, we can order the A1C, a non-fasting lab which looks at a person’s average blood sugar levels over the last 90 days.
Ultimately, labs don’t have to ruin your day — but they should still involve your doctor.
If you have additional questions about bloodwork, or any of our other preventative services here at Banner Peak Health, reach out. We’d love to speak with you.
Executive Physical: Is It Worth It?
Many people are drawn to concierge medicine for its attention to detail and to the individual.
For example, when people are due for their annual physical, they often want more than the traditional healthcare system can provide. This has led to the development of the “executive physical.”
Critiques of the Annual Physical
In 2015, The New England Journal of Medicine published a study claiming annual physicals were a waste of time and money, as they “do not reduce morbidity or mortality, and preventive care can be updated in other ways.”
The study caused an uproar in the medical community. Physicians all across America believed these researchers had insulted the foundations of the traditional healthcare experience.
That’s not exactly true. These researchers were really saying that it’s difficult to put a monetary value on the results of a typical primary care physical. They believed the healthcare establishment could better use its resources elsewhere.
The study holds some truth.
The traditional annual physical is constrained by time and insurance, and often, primary care physicians are unable to help their patients address all of their health care needs.
At Banner Peak Health, we’re free from those time and insurance constraints, meaning we can offer our patients more in the form of the executive physical.
But not all executive physicals are created equal.
The ‘Executive Physical’ Difference
Have you ever seen high-cotton paper? Elegant, high-end paper with cotton content to demonstrate its importance? I see it from time to time.
As the concept of the executive physical has gained popularity, many patients first turn to major academic medical institutions. However, that’s rarely their final stop. After leaving their medical institution of choice, these patients come to me with beautiful binders full of high-cotton paper printed with tons of data — that have never been opened.
To me, this demonstrates the potential weakness of an executive physical; it lacks the means to respond to all the detailed information it discovers.
Banner Peak Health strives to provide something more valuable.
Executive Physicals: The Banner Peak Health Difference
Our executive physical not only investigates possible risk factors, but also provides the structure to implement our findings.
If you’re busy enough to value the time spent on an executive physical, you’ll likely struggle to find enough time to implement the results. That’s how we differentiate ourselves — it comes down to time.
We don’t just generate. We implement.
That’s not to say larger academic institutions aren’t valuable — they have a lot of advanced equipment under one roof. But we take executive physicals a step further by customizing each exam according to the diagnostic studies appropriate for each individual.
We can dedicate the time necessary to provide the care you deserve, and we aren’t beholden to insurance when it comes to what applications, tests, and technologies we can use and order.
From Galleri testing to coronary artery calcium scores, we offer more comprehensive medical insights, and will help you implement solutions every step of the way. Without implementation, test results are just data points printed on expensive paper collecting dust on a shelf.
If you’re ready to implement, we’d love to welcome you as a member at Banner Peak Health. Contact us today.
The Two Types of Body Fat Worth Knowing About
Just as the adage “location, location, location” applies to real estate investing, the same applies to our fat cells.
All fat isn’t created equal. In fact, location highly determines the biology of our fat cells.
In this post, I’ll explain how two classic body types are related to two types of body fat, and why the differences between the two are worth noting.
Body Types and Types of Body Fat
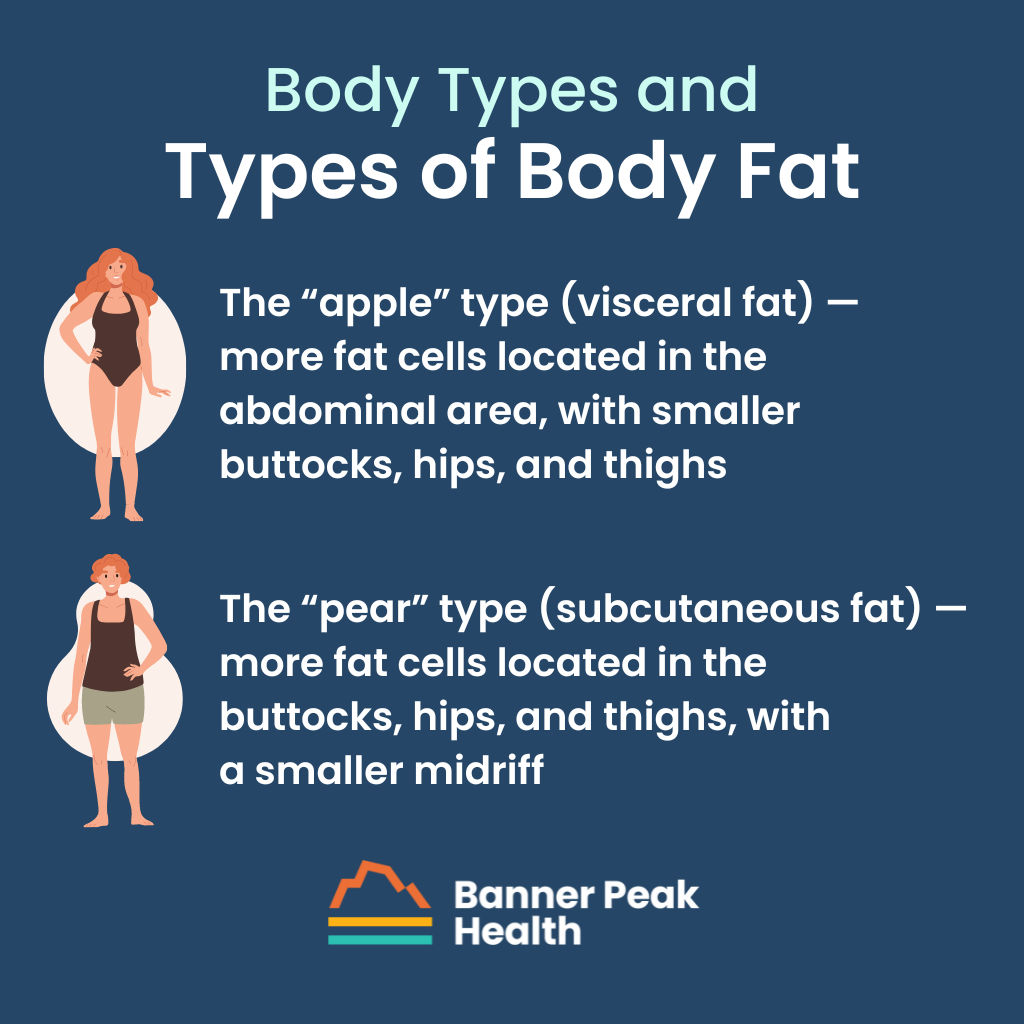
The distribution of fat cells determines two classic human body types:
- The “apple” type — more fat cells located in the abdominal area, with smaller buttocks, hips, and thighs
- The “pear” type — more fat cells located in the buttocks, hips, and thighs, with a smaller midriff
The corresponding types of body fat are visceral fat and subcutaneous fat, respectively.
- Visceral fat = abdominal fat = fat in the gut = the apple body type
- Subcutaneous fat = fat in the thighs, hips, buttocks, and arms = the pear body type
Important Definitions
Let’s take a step back.
We all have a basic understanding that being overweight is “bad for you,” but what does that mean, exactly?
Defining ‘Overweight’
People tend to hyper-fixate on weight. We step on the scale, read the number, and, if it’s too high, we call weight the bad actor. But is it the weight that’s the problem?
There are more accurate ways to measure body composition, such as the body mass index (BMI), but we’ve discussed before why that can also be misleading. (BMI would have a linebacker signing up for Weight Watchers!) Better options, like the InBody scan, can establish an individual’s percentage of body fat and analyze visceral fat levels.
Still, though this information gets us closer, the real answer we’re looking for is the location of the weight and how that affects the metabolism.
Defining ‘Bad for You’
Data collected during the Women’s Health Initiative revealed that postmenopausal women (with normal BMIs) who had high fat cell distribution in the abdominal area (the apple body type) were three times more likely to have unfavorable health outcomes than women with fat cell distribution elsewhere (the pear body type) — even though none of the 2,700 women studied were overweight.
This study illustrates the difference in the biology of fat cells based on location.
Now we can talk precisely about what “being overweight” means and where it’s most dangerous to carry excess weight. There’s also extensive literature exploring the negative outcomes associated with excess visceral fat.
Types of Body Fat and Hormones
Each of us has billions of fat cells distributed all throughout our body, and each fat cell can release up to 20 different hormones. We can think of adipose tissue (fat) as an endocrine organ.
As we reviewed earlier, fat cells aren’t evenly distributed throughout the body. Age, gender, genetics, and hormones determine the location of our fat cells, and we can’t change any of those factors.
In general, the best way to discuss different types of body fat cells is in two main groups — visceral and subcutaneous — based on their location and function.
We’re always learning about our bodies; they’re incredibly complex. For example, in 1994, we discovered a hormone called leptin, which fat cells express to mediate hunger. Since then, we’ve discovered many other hormones secreted by fat cells that impact almost every aspect of our metabolism.
We can now answer the question “why is being overweight bad for you?” at the biological level. Adipocytes (fat cells) secrete hormonal signals called adipokines. The adipokine balance in our bodies determines our health.
Put simply, our fat cells, their location, and the hormones they produce are a huge determining factor in our overall health.
Our Priorities
As a physician, I want to use as many tools as possible to understand each patient’s risk of unfavorable health outcomes.
Understanding not just each person’s height and weight but also their fat distribution helps us to better understand their overall risk for illness, and subsequently, to mitigate that risk.
Today’s Takeaways
- There are essentially two types of body fat:
- Visceral (apple body type)
- Subcutaneous (pear body type)
- Excessive visceral body fat can drastically increase the risk of negative health outcomes, such as coronary artery disease and cancer.
- Fat cells aren’t evenly distributed throughout the body and play a major role in metabolism and overall health.
What Are the Health Benefits of Walking 10,000 Steps a Day?
The other evening, my wife and I were out walking our two dogs.
After a long day, I was ready to head in. My wife pulled out her phone and realized she hadn’t reached her daily goal of 10,000 steps. She asked if I could walk a few more blocks with her.
Although I was tired, I wanted to go with her. I knew it was good for my health, her health, and even the dogs’ health. But I was also curious about my wife’s fixation on the goal of 10,000 steps.
What are the health benefits of walking 10,000 steps a day? I decided to look into it.
Where Does the Idea of ‘10,000 Steps a Day’ Come From?
In 1965, a Japanese company called Yamasa Clock developed a new pedometer. They named it “Manpo-Kei,” which translates to “10,000 steps.”
Why? Because the Japanese character for the number 10,000 resembles a person walking.
That’s it. The name had nothing to do with medical science at all! Instead, it was a marketing decision that, over half a century later, is enshrined in a sort of folklore.
But the story doesn’t end there.
The Health Benefits of Walking 10,000 Steps a Day
We’re aware of the many benefits of aerobic exercise, from weight loss to mood elevation to a reduced risk of dementia.
Robust literature has assessed the dose-response curve for exercise — or, how much exercise yields optimal results.
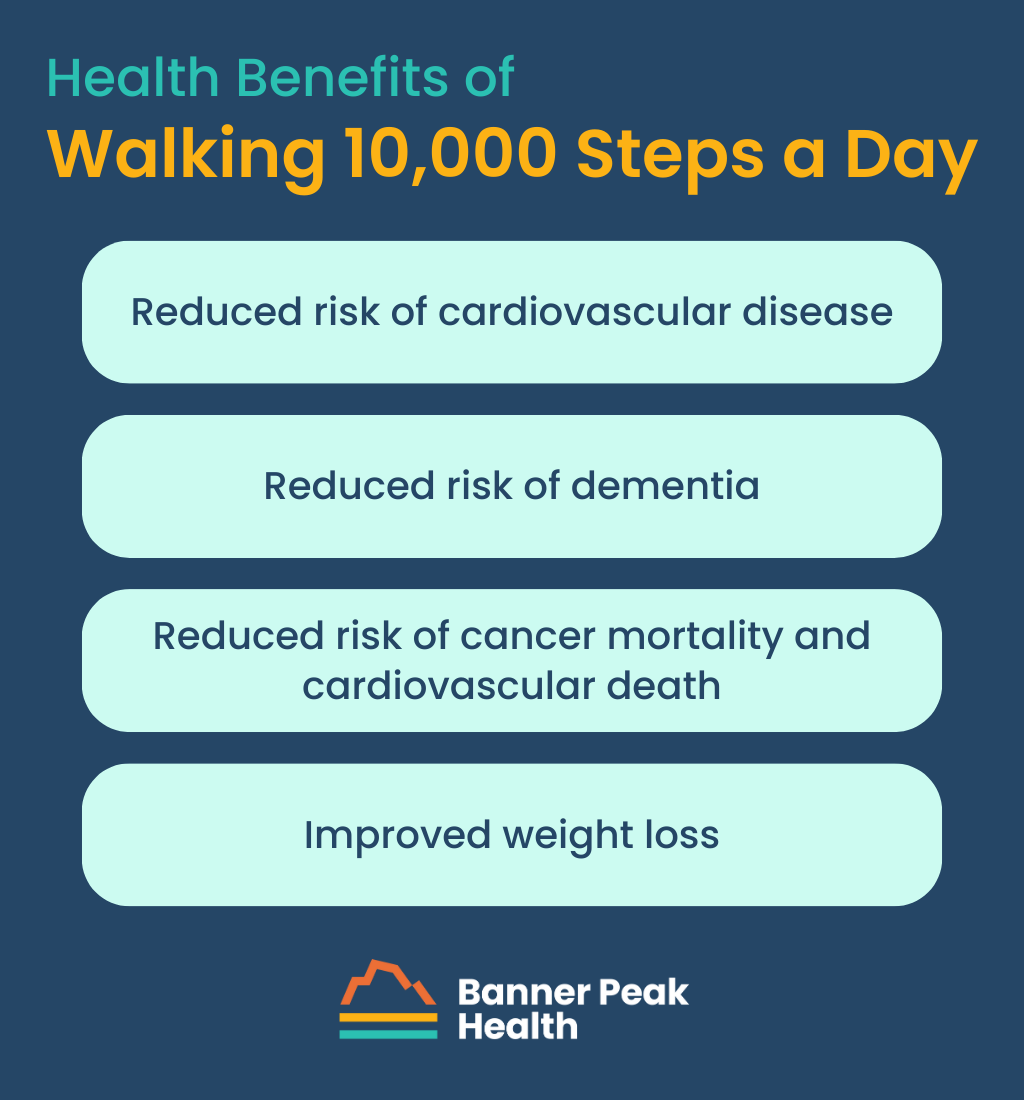
According to a study published in 2019, which monitored 18,000 women over four years, 4,400 steps a day yields better results than 2,700 steps per day. And 7,500 steps per day is better still.
Another study published in 2020 looked at about 5,000 men and women over 10 years. Researchers found that by increasing steps per day from 4,000 to 8,000, subjects could reduce their risk of cardiovascular disease by 50%.
All these studies look for an association between walking and improved health outcomes. However, there’s the obvious confounder here: The more frail or sick you are, the less you walk. So there’s an unavoidable inaccuracy in these studies based on that confounding factor. Nonetheless, they’re being used to encourage people to walk more.
In 2022, results from the largest cohort study to date were released. In Britain, over 78,000 individuals with a mean age of 61 were followed for seven years. The study found that at 3,800 steps per day, dementia risk reduced by 25%, while at 9,800 steps per day, that risk reduced by up to 50%.
Another study looked at the same patient population for overall risk reduction in cancer mortality and cardiovascular death. Researchers found that the maximum benefit occurred at — get this — 10,000 steps per day.
The story has come full circle. After nearly 60 years, what began as a marketing gimmick has proven to be a healthy practice.
Today’s Takeaways
If exercise were a pill, it would be the safest, most powerful drug ever. Literature supports the notion that there are significant health benefits to walking 10,000 steps a day.
Don’t you hate it when your spouse is right?
Everyone knows exercise is good for you on an intellectual level. The challenge we face is helping people develop habits that encourage them to incorporate this behavior into their daily routine.
It’s helpful to find ways to exercise that are fun, or at the very least, less onerous. For example, walking with friends, family members, or furry family members may be enjoyable for you. And if tracking and counting steps helps motivate you to walk farther every day, go for it!
Wegovy, Ozempic, and Mounjaro: Approach Miracles With Caution
When I was a medical student, an elderly physician gave me some sage advice: “Never be the first to prescribe a new drug or the last to prescribe an old drug.”
His admonishment instilled in me a healthy skepticism regarding the risks and benefits of pharmacologic treatment. As it turns out, his caution was well-founded. Over the last 30+ years of practice, I’ve watched dozens of drugs be released and pulled from the market.
The pharmacologic treatment of obesity is particularly rife with examples:
- Fen-Phen (Fenfluramine): Pulled in 1997 for damaging heart valves and leading to pulmonary hypertension.
- Ephedra: Banned by the FDA in 2004 due to increasing people’s risk of heart attack, stroke, and death.
- Acomplia (Rimonabant): Pulled in 2008 due to a demonstrated risk of psychiatric crises, including suicide.
- Meridia: Pulled in 2010 due to increased risk of heart attack and stroke.
However, obesity and its associated health risks continue to need a pharmacologic tool, and the medical establishment continues to explore new treatments for this highly dangerous medical condition.
The latest drugs developed in the fight against obesity, including Wegovy, Ozempic, and Mounjaro, are categorized as GLP-1 agonists. They may be all the rage at the moment, but they’re not for everyone.
Let’s explore these powerful drugs and discuss GLP-1 agonist side effects.
GLP-1 Agonists: The New ‘Miracle’ Drugs
GLP-1 agonist stands for glucagon-like peptide-1 agonist. This class of medication has a wide array of effects on the body, including appetite suppression, increased insulin production, decreased glucose production, and increased glucose uptake in muscle cells.
GLP-1 agonists were originally developed to help patients with type 2 diabetes lose weight, reduce blood sugar levels, and lower the risk of cardiovascular death. However, we’re now facing the expansion of the use of these medications for weight loss in the general population.
In particular, the drug Mounjaro, which has both GLP-1 agonist and GIP (glucose dependent insulinotropic polypeptide receptor) effects, is the most effective weight loss drug to date. Studies demonstrate a five to 22.5% reduction in body weight, which is unheard of compared to prior weight loss technologies.
The challenge we now face is identifying patients for whom the benefit of Mounjaro exceeds the associated risk.
A Note on Risk/Benefit Ratios
Remember, there is no such thing as a “totally safe” drug. The truth is, all drugs have risks. We must inspect the risk/benefit ratio for all medical therapies according to an individual’s unique circumstances and determine whether prescribing the drug makes sense.
For example, an obese person faces many serious health risks. A drug like Mounjaro can effectively reduce those risks by reducing obesity, meaning the benefits of Mounjaro may outweigh its potential side effects. However, there’s no guarantee, and every case must be carefully considered.
GLP-1 Agonist Side Effects
What we’re seeing now, which is concerning, is people who are not obese using GLP-1 agonists to lose those “last few pounds.” This use of these drugs is particularly popularized on social media.
The danger of weight loss enthusiasm occurs when people take a medication without fully understanding the potential risks. Typical GLP-1 agonist side effects include nausea, vomiting, and diarrhea. However, a more subtle and treacherous threat hides in the weight loss itself.
Dr. Peter Attia — a careful and critical reader of medical literature — describes this risk and highlights the need for additional research in his blog.
“...not all weight loss is healthy. While shedding excess fat mass (and in particular, visceral fat mass) has a multitude of beneficial effects on health, shedding lean mass — which includes muscle and bone — is associated with poorer health trajectories and reduced lifespan.”
What Dr. Attia is referring to is our overall body composition, which we mentioned in a previous post. Fat is one component of our body composition, but so is water. We call whatever isn’t water or fat dry lean mass: muscles, bones, connective tissue, etc.
Dr. Attia brings attention to a small sub-study: 140 patients who lost weight using GLP-1 agonists underwent DEXA scans for body composition analysis, which revealed that up to 39% of total weight lost was lean body mass.
In another trial, a subset of 178 patients showed up to 40% loss of lean body mass. This means for every 10 pounds lost, up to 4 pounds of that loss was muscle and/or bone. These results are alarming, as trials of past weight loss drugs showed only a 25% or lower loss in lean body mass.
We want to preserve lean body mass, especially as we age. Unfortunately, the studies cited by Dr. Attia demonstrate that GLP-1 agonist side effects can have an exceptionally high cost.
These studies were small subsets of larger ones and need more exploration, but the initial findings should be enough for physicians to pause and consider all potential GLP-1 agonist side effects prior to use.
Today’s Takeaways
GLP-1 agonists can be life-changing — and life-saving — for certain individuals. It’s an incredible advancement for people with diabetes or who are obese and need pharmacological help.
However, because of GLP-1 agonist side effects, particularly the loss of muscle mass, these “miracle drugs” are probably not a good choice for people who don’t have diabetes or are not obese. Don’t take these drugs if they’re unnecessary or if your doctor doesn’t recommend them.
I’ve seen many so-called “miracle” drugs come and go, and one thing holds true for them all: they’re miraculous until they’re not.
I want my patients to tell me about their miracles 25 years from now, not just two or three years down the road. Real results stand the test of time.
BMI vs. Body Composition: What’s the Difference and Why Should You Care?
Being overweight correlates with a long list of bad health outcomes, including but not limited to:
- Increased risk of diabetes
- Coronary artery disease
- Stroke
- Cancer
- Wear-and-tear osteoarthritis of the joints
Fat is necessary, but excess amounts can hurt us. Therefore, we need to quantify and monitor our total weight in such a way as to prevent bad outcomes.
We need to understand the difference between BMI vs. body composition, and how we can track and learn about the latter.
What Is Our Body Composition?
The healthy range for body fat varies according to age and gender, but for men, it runs between eight and 28%. For women, it’s 21–35%.
But fat is only one component of our body composition. We’re also made of water. Men are about 60% water; women are about 55%.
Whatever isn’t water or fat is called dry lean mass: muscles, bones, connective tissues, etc. Dry lean mass is calculated by subtracting your water and fat quantities from your total body mass.
We’re all made of water, fat, and dry lean mass, but a standard scale won’t tell you exactly how much of each you carry. We need another method to determine our body composition.
What Is BMI?
Let’s discuss BMI vs. body composition. Can you use the former to determine the latter, and vice versa?
BMI (body mass index) is a mathematical ratio calculated based on a person’s total weight and height. Unfortunately, it’s flawed and inaccurate because it doesn’t consider individual body composition.
Very healthy people with increased muscle mass can be considered overweight by BMI standards. For example, an NFL player may have a high BMI (i.e., a high weight for their height) because of their tremendous muscle mass, but no one would recommend they enroll in Weight Watchers!
BMI vs. Body Composition
Since BMI has significant limitations, I looked into other technologies used to measure body composition. Unfortunately, there’s often a trade-off between ease of use and accuracy.
One can use a simple caliper to squeeze available subcutaneous fat at different parts of the body, then calculate the percent body fat using a table. This method is straightforward and cheap, but unfortunately, it isn’t accurate.
Another method is hydrostatic weighing, in which a patient’s body is completely submerged in water, and the displacement and density are calculated. The results are accurate, but the test is clinically impractical.
Other accurate technologies, such as a DEXA (Dual-Energy X-ray Absorptiometry) scan, are convenient but may not be geographically or financially accessible.
After weighing the pros and cons of many body composition calculators, we at Banner Peak Health decided upon InBody, a bioelectrical impedance device.
BMI vs. Body Composition: What Is Bio-Electrical Impedance?
Water conducts electricity, and fat doesn’t, a principle of which InBody takes advantage. The device measures electrical resistance across different axes of the body, from which an accurate calculation of a patient’s body composition (body mass, water, and fat) can be made.
By using this convenient, accurate tool, we address patients’ important clinical issues.
For example, patients who want to lose weight often make lifestyle changes, including dietary and exercise modifications, only to be frustrated when the number on the scale doesn’t change. InBody encourages those patients by showing them how their lifestyle changes have impacted their body. Often, their percentage of body fat decreased as their percentage of muscle increased — so while their overall weight didn’t change, the internal makeup of the body did.
Another clinical benefit of InBody relates to weight loss in aging patients. A prevalent problem called sarcopenia (the loss of muscle mass) is associated with many bad outcomes during the aging process. Fortunately, bioelectrical impedance technology allows us to monitor body composition and watch for decreases in muscle mass.
We invested in this technology because InBody allows us to offer a higher standard of preventative care. We’re delighted to provide it in our office for our members.
The Banner Peak Health Difference
When it comes to BMI vs. body composition, it’s important to take the former with a grain of salt and invest in clinically convenient technologies to determine the latter.
At Banner Peak Health, we’re proud to invest in state-of-the-art diagnostic technologies that can give us greater insight into patients’ health to further customize their treatments, better meet their healthcare needs, and maximize their quality of life.
If you’re interested in using InBody to determine your body composition, schedule an appointment today.
Don’t Ignore the Core: How Core Strength Is Essential for Cycling
Core strength is essential to almost all athletic performance.
In nearly all sports, the force generated from a limb (like an arm or leg) must be anchored by a strong trunk — the core. Otherwise, the force is severely diminished.
Imagine throwing a football while you’re floating in an inner tube. Now imagine throwing a football while standing firmly on the ground. The latter football will cover much more distance than the former.
But what are the core muscles? How can we as athletes improve our core strength, especially core strength for cycling? Read on to find out.
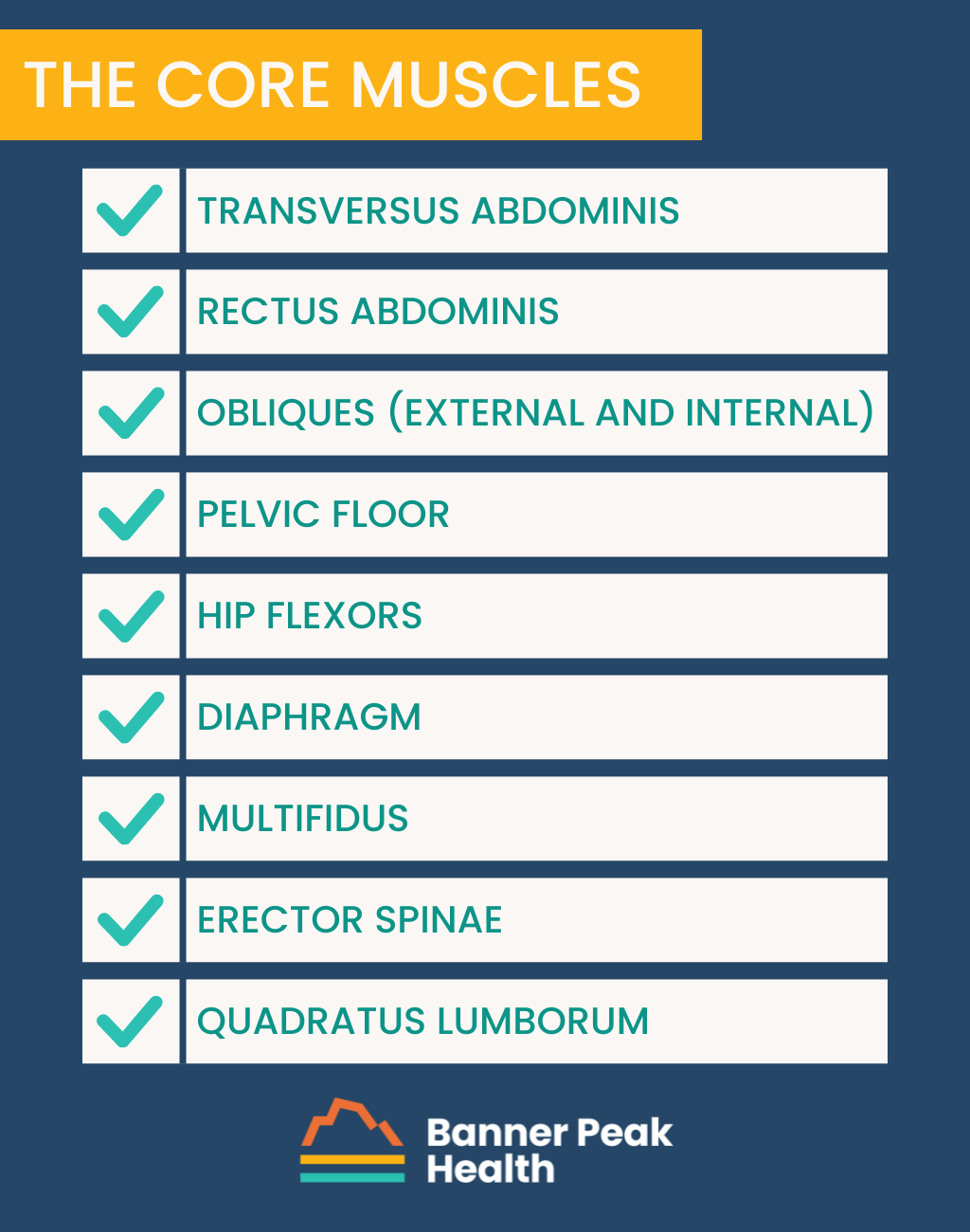
What Are the Core Muscles?
The core muscles are a system of muscles covering the pelvis, lower back, hips, and stomach.
Some have names you’ll recognize, like the gluteus maximus, while others are more obscure, like the external obliques or multifidus. Regardless of popularity, they all work together to get the job done, whether that job be teeing off successfully or throwing a football across a field.
How the Core Muscles Work
Each myocyte (muscle cell) contains countless layers of two overlapping molecules: actin and myosin. Biochemical reactions between these two molecules cause the cell to contract. The combined force of these myocytes creates the strength of a muscle. Thus, the more groups of muscles that create a movement, the stronger the force of the movement will be.
Golf illustrates this principle perfectly.
Many golfers believe the force behind their swing is determined solely by the mass of their arms or pelvis. They have no idea the vital role core strength plays in golf — though having a six-pack may not help your putting stroke.
The same is true in swimming. Your core anchors your arms and legs as you kick, reach, and pull. All those muscles working together generate tremendous power.
Tennis is another great example. When you watch players run across the court, serve, and hit backhand and forehand shots with incredible force, know it’s due to the engagement of their core.
But a favorite and personal example of the core’s influence is cycling.
Core Strength for Cycling: My Personal Experience
When it comes to cycling, core strength is particularly important. The core anchors the pelvis to generate the power the legs need to pump the pedals. It also keeps the torso angled forward for wind resistance.
I started cycling when I was 12, nearly 50 years ago. By age 30, I’d realized the truth behind the adage, “You have to give to your body to receive from your body.” At that point, I’d developed a workout regimen to help me maintain core strength for cycling.
Over the decades, as I’ve changed and as technology has changed, my regimen has evolved.
In my 20s, I did the sit-ups we all learned in gym class — the ones where you touch your elbow to the opposite knee. However, we now know that those sit-ups cause hyperflexion in the lumbar spine, which increases the risk of lower back injury and pain.
Now, I maintain my core strength for cycling through static planking maneuvers, and I’m proud to say I’ve never had any back problems in my nearly 50 years of riding.
Ironically, I did suffer neck pain associated with cycling several years ago. It turned out that I’d neglected my “north core” — the muscles that stabilize the shoulder girdle, upper back, and neck.
I’ve since expanded my workout regimen to address these muscles and have been able to cycle painlessly.
My advice to all athletes — cyclists in particular — is to be diligent and invest in your core strength, both of the middle core and the north core.
There are several ways to achieve this. You can seek out fitness instructors, physical therapists, Pilates classes, online videos, yoga classes, or books.
The avenues are virtually limitless, so find the one that’s best for you and stick with it. You’ll never find a better investment in athletics — and you’ll never regret it.
The Dangers of Overlooking Your Core
Maintaining your core is both offensive and defensive. Core strength training allows you to stay on the bike longer, hit the golf ball farther, etc., but it also prevents injury, especially in aging athletes.
As I’ve said before, an injured athlete is not a training athlete. Time off to recover takes you out of the game.
Maintaining a strong middle core (and north core) is one of the best preventative measures an athlete can take at any stage of life.
Today’s Takeaways
If Pilates isn’t for you, rest assured there are many ways to build core strength for cycling, golf, tennis, and other sports.
Pick the right avenue for you and stay with it. You’ll be glad you did.
Why Do I Get Headaches After a Nap?
There are two types of adults in the world: the ones who benefit from naps, and the ones who don’t.
If you are a “nap person,” you may be one of the many who experience grogginess after a nap. You may have even asked your doctor, “Why do I get headaches after a nap?”
Fortunately, we can help you with these questions.
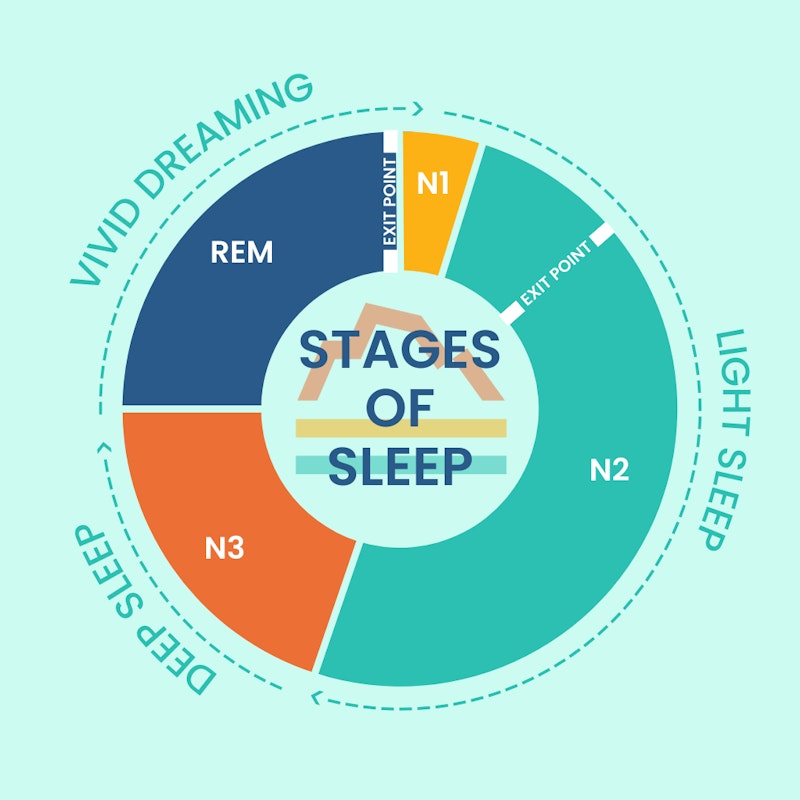
Sleep has an architecture. You sleep in stages, and when you understand those stages, you’ll understand why your naps aren’t always refreshing and what you can do to change that.
The Architecture of Sleep
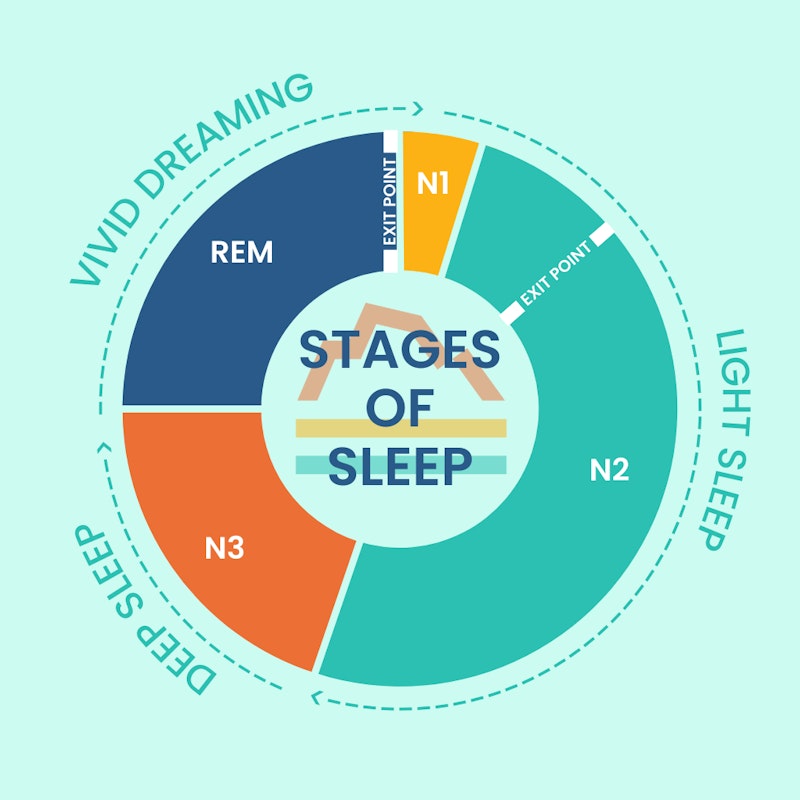
Sleep isn’t a random event. It’s made of four individual stages which, together, comprise a 90-minute cycle:
- Stages one and two are light sleep.
- Stage three is called Delta sleep, or deep sleep.
- Stage four is REM (rapid eye movement) sleep. This is the stage in which we dream.
Why Do I Get Headaches After a Nap?
Ever Googled “Why do I get headaches after a nap?” Here’s your answer: The most common cause of that dysphoric, groggy post-nap feeling is waking up mid-sleep cycle.
When you interrupt your sleep cycle, your body doesn’t have the opportunity to complete its natural process. The interruption leaves you feeling out of sync and can result in adverse symptoms, including headaches.
Preventing Headaches After Naps
If you’d like to reduce your potential for grogginess and headaches after napping, there are two techniques I recommend:
- When you lie down to take a nap, set an alarm for 15–20 minutes. This ensures you only spend time in the light sleep stages, making it easier to wake up and less likely you’ll experience uncomfortable side effects.
- If you have time, set your alarm for 90 minutes. This allows your brain to complete a full cycle but wake up before beginning a new one.
Other Advice
If you nap frequently and commonly ask, “Why do I get headaches after a nap?” you may be asking the wrong question.
Perhaps you should ask whether you’re optimizing your sleep at night. For example, are you napping because you don’t sleep well at night? If so, prioritizing your nightly sleep habits should come way ahead of learning how to nap better.
We can help with that, too. Read our most recent blog post on sleep, or contact our office to schedule an appointment. We’re happy to help repair your relationship with sleep.
Today’s Takeaways
- Some people benefit from naps, some don’t.
- Sleep has an architecture of four stages, which take 90 minutes to complete.
- Interrupting your sleep cycle during Stages 3 and 4 can cause uncomfortable side effects such as grogginess and headaches.
- To avoid unwanted side effects from napping, set an alarm for 15-20 minutes so you wake up in a light sleep stage. Or, set an alarm for 90 minutes so you wake up after a complete sleep cycle.
- If find yourself asking “Why do I get headaches after a nap?”, don’t just focus on napping better. Optimize your nightly sleep habits, as well.
What Is a ‘Stress Belly’ and What Does One Look Like?
You may not believe this, but not everything you read on the internet is true — especially when it comes to medical facts.
Shocking, I know.
You may have heard of something called “stress belly” and wondered what it looks like. Stress belly is a real phenomenon, but it’s very different from the images and blog posts you’ll find if you Google “what does a stress belly look like.”
Those images are total BS.
There’s no way to immediately identify the cause of abdominal fat deposition simply by looking at the belly. (Plus, anyone who carries so much fat on their abdomen won’t look like a supermodel everywhere else.)
That being established, what is a stress belly, and what does a stress belly look like?
What Does a Stress Belly Look Like?
Stress belly is the result of a direct physiological link between the emotional stress you experience and increased fat deposition in your abdominal cavity.
Not everyone with abdominal obesity has a stress belly. Likewise, not everyone who experiences excess stress develops a stress belly or abdominal obesity. However, there’s enough overlap to ensure a genuine phenomenon, although it’s not explanatory for all instances.
Causes and Symptoms of Stress Belly
There are many instances of powerful, intricate relationships between our emotional state and our physical state.
A lot of literature links socioeconomic status to health outcomes. For example, if you’re struggling financially, you may not be able to consistently provide food or housing for yourself or your family. The amount of stress engendered by a lower socioeconomic status is considerable.
When we experience chronic stress, we see elevated levels of adrenaline and cortisol, a glucocorticoid which can be measured in saliva, blood, and even hair. These elevated levels correlate with worse health outcomes.
Too much cortisol can set a whole host of other hormonal changes into motion, including putting more adipose (fat) cells within the abdomen. These visceral fat cells are hormonally active, pro-inflammatory, create insulin resistance, and worsen hypertension, which are all risk factors for coronary artery disease.
They’re part of a worsening feed-forward loop that also influences hormones that regulate appetite, like leptin and ghrelin. This causes people under stress to crave comfort foods (foods high in sugar and fat), which compound obesity and continue the feed-forward loop.
Together, all these factors form an unfortunately strong and documented pathway — starting with socioeconomic status and emotional state and leading to increased fat content, heightened cardiovascular risk, and many other downstream health complications.
Risk Factors for Stress Belly
The risk factors for stress belly begin with its namesake — stress. Despite the documented link between socioeconomic status and stress, stress can affect anyone in any circumstance.
Stress isn’t always caused by emotion, either. For example, chronic pain can cause stress. It’s like kicking someone when they’re down.
Another cause of stress — and therefore excessive cortisol, or hypercortisolism — can be a lack of sleep. If you consistently fail to get the proper quantity or quality of sleep, your body generates more adrenaline and cortisol. This especially affects night shift workers, whose circadian rhythms are all out of whack.
The same thing happens when you consume alcohol. Most people equate drinking with relaxation. However, as your body metabolizes alcohol, it releases adrenaline and cortisol, which stresses your body and induces hypercortisolism.
Stress Belly Treatment
So you’ve gotten past “what does a stress belly look like?” and moved on to “how do I get rid of my stress belly?” I hear you.
The best way to combat stress belly is to identify and address its contributing factors. Then, double down as much as you can on removing or managing the factors that cause undue stress and lead to hypercortisolism.
Emotional Stress
When emotional stress weighs heavily, meditation, cognitive behavioral therapy, exercise, and other techniques and tools can relieve some of the burden. Don’t wait until you feel overwhelmed before you ask for help.
Chronic Pain
If you’re experiencing chronic pain, you may not be able to remove the pain or the source of the pain completely, but there may be ways to improve your quality of life. For instance, through meditation, therapy, or other modalities, you may be able to emotionally reframe your pain so it’s less stressful to your body.
Alcohol
Alcohol consumption can be simpler to limit (or omit), but not always. Alcohol is not part of the solution for stress — it’s part of the problem.
If you need help limiting or abstaining from alcohol, contact your doctor or a support group near you.
Sleep
Sleep is crucial to wellness. However, improving sleep can be incredibly complicated.
If you’re having trouble sleeping, please talk to your doctor or contact us here at Banner Peak Health. We’ll be glad to speak with you.
Today’s Takeaways
- All the charts that pop up when you Google “What does a stress belly look like?” are BS.
- Stress belly is real. No, you can’t tell if you (or anyone else) have it just by looking.
- Stress belly increases the risk for a wide array of illnesses, including diabetes, high blood pressure, and coronary artery disease.
- Treatment for stress belly involves managing and omitting the causes of stress. These can include emotional stress, chronic pain, alcohol, and poor sleep.
Text Neck: The Hidden Epidemic We Shouldn’t Ignore
Everyone’s heard the mantra of the “core,” defined as the lower back, hips, pelvis, and stomach. We all know the core is essential for movement and athletic performance.
But what about the north core?
Never heard of it? I’m not surprised.
What I define as the “north core” is the group of muscles surrounding your neck. Unfortunately, the neck is the forgotten part of the spine.
In my opinion, we focus too much on the main core — that anatomy is extremely solid. We really haven’t focused on the ergonomics and protection of the north core, even though those muscles give the neck strength and flexibility.
The seven cervical vertebrae are tiny, and we aren’t conscious of the surrounding muscles... that is, until the pain of text neck starts.
The Neglect of the North Core
Neglecting the neck can lead to a domino effect of symptoms in our musculoskeletal system.
When we ask our muscles to perform tasks they simply can’t do, they become stretched and inflamed. They spasm. As they spasm and contract, they create tension in adjacent muscle groups.
What starts as overuse of a small group of paraspinal cervical muscles turns into trapezius spasms, shoulder pain, and headaches. And it’s all driven by overuse of these little muscles.
To prevent a pain syndrome cascade, we need to better protect and be conscious of our cervical muscles.
Let’s Talk About Text Neck
There’s an epidemic of neck pain, and the driver is poor ergonomics and how we interact with screens — particularly handheld devices like phones. The condition is called text neck, and recent studies show astounding results.
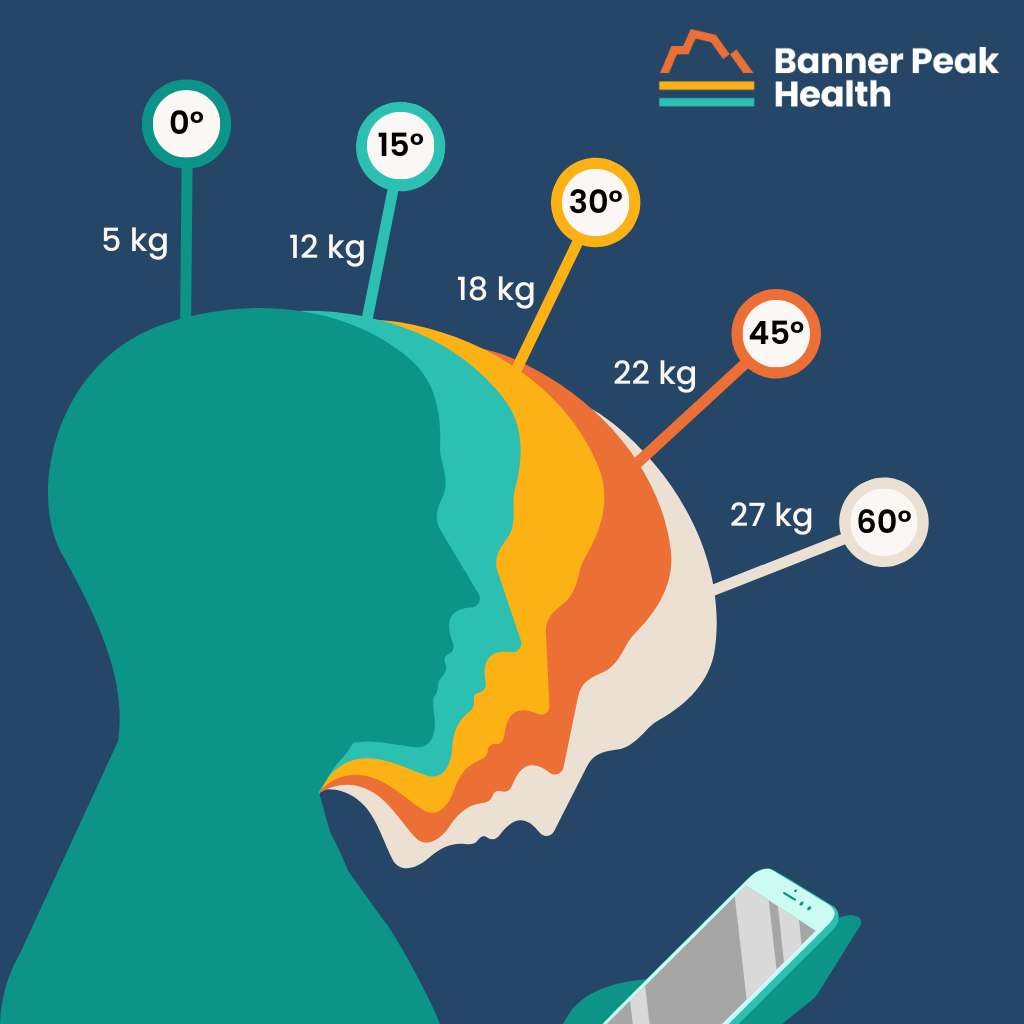
The average human head weighs 10–12 pounds. As you tilt your head forward, you increase the force applied to the base of your neck.
As you can see in the graphic, even slight increases in tilt angle drastically increase the amount of force transmitted to your neck. By the time your head is tilted to a 45-degree angle, the force on your neck has increased fivefold!
Heavy is the head that stares at the phone.
Imagine the effect of this amount of sustained pressure over hours every day. Voilà — text neck!
What if We Ignore Text Neck?
Who doesn’t have neck pain?
My best friend once asked me to refer him to a good acupuncturist because his neck was killing him. I told him I’d refer him to a good acupuncturist if he promised to stop resting his laptop on his chest while he used it in bed.
Don’t put a Band-Aid on a bullet hole. There’s no reason to provide a small, momentarily effective treatment if you don’t do anything to address the root cause of the problem.
As I mentioned earlier, the issue with neglecting your north core is the domino effect it can cause throughout your musculoskeletal system. Overuse leads to stretching and inflammation, which leads to spasms, which leads to pain in the neck, which migrates to the shoulders and back and causes headaches.
Simply put, it’s not just about neck pain.
Stop Blaming Your Pillow for Text Neck
Often, patients ask me what the best pillow is for neck pain. When I ask why, they tell me they wake up every morning with terrible neck pain and insist it must be their pillow.
Let me assure you — it’s not your pillow’s fault.
The mechanism for generating the pain you woke up with is the muscle you overused the day before, the inflammatory process that set up overnight, and the spasm you woke up with. Just because you woke up in pain on your pillow doesn’t make it your pillow’s fault.
What We Can Do About Text Neck
First, we must be aware that text neck syndrome is real and common. The signs are frequent neck pain, headaches, shoulder pain, and pain anywhere from the top of your head to your armpit. The problem is widespread, and we need to address it.
Amazingly, there’s an app for that!
Some brilliant people have found a way to use a smartphone’s motion sensor to determine the angle at which the phone is being held. The app alerts the user with a red light when the angle of view is too severe.
Using tools like this can significantly improve your posture during device use and reduce your risk of developing text neck. Taking advantage of voice-to-text functions and voice assistants like Siri and Alexa more often can also help.
Finally, you can improve your range of motion and alleviate pain by stretching regularly. Since pain is caused by muscle spasms and tightness, stretching those muscles can help reduce pain and prevent further damage.
Today’s Takeaways
- Your “north core” deserves just as much attention as your main core.
- Text neck is real and incredibly common.
- A new pillow won’t solve the problem. Instead, try posture-improvement apps, voice-to-text assistance, and stretching exercises to improve your north core strength and prevent text neck.