How to Make Safe Choices With Supplements
For this topic, I’d like to share a few stories about patients I’ve had over the years.
A patient of mine, a young woman in her 30s, was suffering from chronic fatigue and joint pain. This was during COVID, but all her workups were negative. I struggled to determine whether she had a chronic illness.
She began seeing a naturopath, who prescribed a series of supplements — at least 10 to be taken in tandem. A month after she began taking these, she called the naturopath’s office to tell them she felt worse. The naturopath reassured her she was detoxing, and she’d feel worse before feeling better.
Skeptical, she called me, and I asked her to come into the office. She was jaundiced, so I did some lab tests. The results showed she was in liver failure.
She ended up hospitalized and on a liver transplant list. She was young and otherwise healthy, so three or four months after stopping the supplements, her liver fully recovered, and she didn’t need a transplant.
Although it’s difficult to determine which supplement played the biggest role in her liver failure, there’s no doubt the supplements caused her condition. She was extremely lucky to make the recovery she did.
Another patient of mine was taking an off-brand fish oil supplement and suffered from hair loss. We investigated and found she had mercury toxicity. Her mercury levels decreased once she stopped taking the fish oil, and her hair grew back.
Finally, I saw a patient who always presented with high liver enzymes at her routine physicals. Although we did many workups, we struggled to determine the reason.
Eventually, I asked if she took any vitamins. She brought me a huge bag of supplements that contained toxic doses of vitamin A. Mystery solved.
I share these stories to demonstrate a point I often make to my patients: vitamin supplements can provide our bodies with necessary elements they would otherwise lack, but taken without caution and care, these same supplements can do more harm than good.
Not All Supplements Are Safe
In 1994, the Food and Drug Administration (FDA) passed the Dietary Supplement Health and Education Act (DSHEA). It established that “dietary manufacturers” don’t need to adhere to the same regulations as pharmaceutical companies.
This means as long as a product is categorized as a “dietary supplement,” manufacturers don’t need to prove positive results before marketing and selling the product. Instead, the FDA must prove the product is unsafe before issuing a recall, a process which can take years, leaving potentially dangerous products on store shelves in the meantime.
Many products go to market containing poor-quality ingredients, hiding ingredients that aren’t listed on labels, or lacking the ingredients they claim to contain. As such, labels frequently list minimal information regarding ingredients and the amount of each.
For example, several years ago, I saw a patient with high blood pressure and diabetes. She was overweight and had tried many different weight loss plans. One day, she told me she’d lost 12 pounds in three months.
I congratulated her and asked how she did it. She showed me the supplement she’d been taking.
The ingredients confused me, because they were all benign things like cranberries and fruit pectin. When I investigated further, I discovered that the supplement contained Fen-Phen, which was especially dangerous for this patient, who already had high blood pressure.
Not only are there virtually zero quality control measures for supplements, but there’s also a real danger in thinking they’re safe for anyone in any dosage just because you can access them over the counter.
That’s simply not true.
More Is Better, Right?
Wrong.
Companies often take advantage of loose federal regulations. Pair that with the ability to buy online, and we’re left with a huge industry harboring immense potential for disaster.
In America, we tend to believe more is better. If one is good, three will work faster or better. However, that isn’t consistent with what we know about your body’s homeostasis.
The truth is, a little of something might help, but too much might throw other things off.
Throughout the past few years, Americans have been desperate for information and looked to supplements to boost their immune systems during lockdown. At the same time, there’s been mistrust of the medical establishment and the propagation of pseudoscience to desperate people.
We all want to be in control of our health, but we take these supplements without realizing the potential hazards. Often, we don’t even disclose what we’re taking to our doctors. But we should.
Risks Associated With Common Supplements
Below is a list of the most common supplements that carry the highest risks (and what those risks are) when taken in excess or when manufactured poorly. Talk to your doctor before starting or altering any medications or supplements.
Poor Quality Risks — Contamination
- Harmful substances
- Mold — consequence of improper storage or expired ingredients.
- Medication
- Male enhancement supplements (Viagra, Cialis, etc.) — some amounts may contaminate generic or natural supplements produced for male enhancement, which is dangerous for men taking nitrates for their heart.
- Heavy metals
- Mercury — sometimes present in low-quality fish oil.
- Lead and arsenic — Ayurvedic medicine may contain these.
- Allergens
- Shellfish — collagen supplements often contain crustaceans.
Excessive or Unnecessary Dosing
- Vitamin E — can be in a standalone vitamin or multivitamin; taken for heart health; more than 400 IU daily may increase all core causes of mortality, and over 800 IU daily may increase the risk of heart failure.
- Vitamin B6 — excessive doses can increase neuropathy.
- Selenium — taken for prostate health; can increase hemoglobin A1C, risk of melanoma, and all core causes of mortality.
- Vitamin A — can cause birth defects when taken during pregnancy; increases risk for osteoporosis and hip fractures.
- Saw Palmetto — taken to remedy hair loss; can cause birth defects when taken by pregnant women.
- St. John’s Wort — interacts with antidepressants and can cause serotonin syndrome; decreases the effectiveness of birth control.
- Kava Kava — can lead to liver failure.
- Gingko — taken for improved cognition; can increase risk of brain hemorrhage, seizure, and stroke.
- Ephedra — banned in 2004 in the U.S. after dozens of people died as a result of taking it; causes heart attack, stroke, and sudden death.
- Biotin — taken for hair, skin, and nails; can interfere with the following tests:
- Blood tests for heart injury and heart failure — can throw off the results
- Thyroid testing — can throw off the results
- Urine pregnancy tests — can affect the control line
Today’s Takeaways
- Supplements aren’t inherently bad, but you must be careful about what and how much you take.
- Let food be thy medicine. Don’t take supplements to make up for a terrible diet.
- Talk to your doctor. They can tell you what supplements you really need, check for drug interactions, and educate you on side effects and warning signs. Keep your doctor in the loop and avoid becoming our next horror story.
Perimenopausal Hormone Replacement Therapy — An Updated View
In the 1940s, the medical community introduced the idea of giving menopausal women estrogen to combat their symptoms. Twenty years later, the FDA approved the first estrogen pill.
For the next few decades, supplemental estrogen was generally seen as positive. Observational studies in the 1980s and 90s even suggested a decreased risk of cardiovascular disease in women receiving hormone replacement therapy (HRT). In 1992, a randomized controlled study called the Women’s Health Initiative (WHI) set out to determine once and for all if and how women benefit from HRT.
The WHI planned to follow 27,347 women between the ages of 50–79 over 13 years. The average participant was 63 — a significant limitation, considering the study didn’t take into account a younger population of perimenopausal women.
The results of the WHI shocked the medical community: for the population studied, HRT didn’t protect from heart disease and resulted in an increased risk of breast cancer. Doctors spent the next few decades making recommendations based on this study’s results.
We’re just now beginning to realize how flawed the WHI was. It omitted a significant portion of the population — perimenopausal women, who, as recent investigations suggest, benefit the most from HRT.
The medical community has spent the 2020s reevaluating the benefits of HRT for perimenopausal women.
‘The Change’ and How Hormones Can Help
During perimenopause and menopause, estrogen and progesterone levels in the body drop and cause vasomotor symptoms (hot flashes, night sweats, and sleep disturbances).
Loss of estrogen can cause loss of bone and muscle mass, mood changes, difficulty concentrating, and loss of sexual function and libido. Sleep disturbances in particular create a cycle that increases other health risks, such as cardiovascular disease and diabetes.
Recent investigations show vasomotor symptoms must be treated by HRT within 10 years of onset for the best results and the best chance of preventing osteoporosis.
Types of HRT
There are several types of HRT, and each requires specificity. For example, if you have an intact uterus (i.e., have not had a hysterectomy), you would need to take progesterone in addition to estrogen to minimize the risk of uterine cancer, endometrial hyperplasia, and endometrial cancer.
Years ago, HRT was usually given orally. Since then, technology has developed many convenient and effective ways to deliver hormones.
Depending on their doctor’s recommendations, women can choose from oral pills, topical preparations, implanted subdermal pellets, or transdermal patches. Transdermal patches in particular are gaining popularity because they tend to cause fewer side effects than other methods. Specifically, they don’t tend to raise cholesterol as much as oral pills.
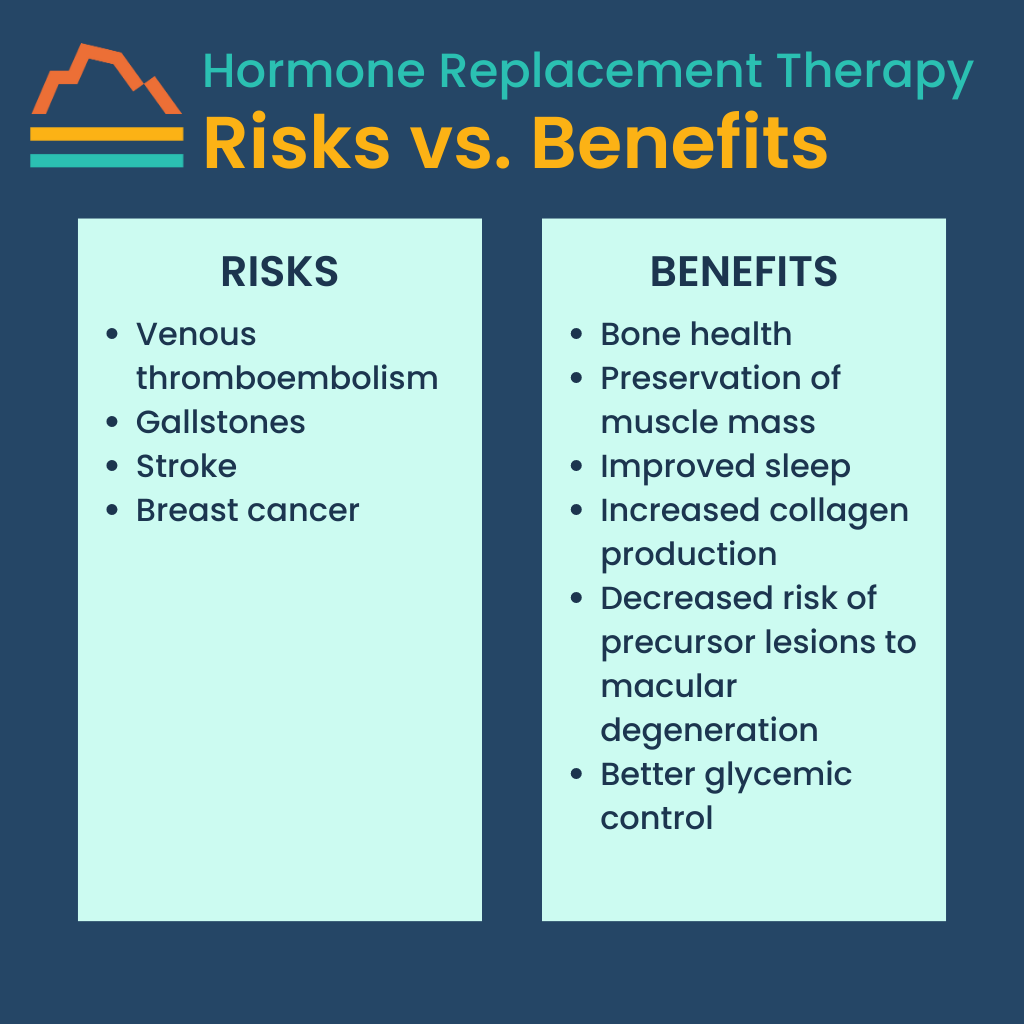
Risks vs. Benefits
Although HRT can effectively reduce the symptoms of perimenopause, it’s not right for everyone. It can cause a risk of venous thromboembolism, gallstones, and stroke, and a very slightly increased risk (0.0009%) of breast cancer. Women who have a family history of blood clots may be encouraged to avoid HRT altogether.
However, for most women, the benefits of HRT far outweigh the potential risks. The most common benefits include bone health, preservation of muscle mass, improved sleep, and increased collagen production. In African American women, HRT may also decrease the risk of precursor lesions to macular degeneration.
For women with diabetes, HRT may lead to better glycemic control — though because of an inherent increased risk of heart disease, women with diabetes must be carefully selected for HRT to avoid unnecessary risk.
The key is treating women early. Once a woman goes through menopause, HRT is no longer effective in treating symptoms or reducing the risks for these conditions. It can even be detrimental.
In one study, women treated with hormone replacement during “mid-life” (avg. 48.7 years) saw their risk for dementia decrease by 26%. However, women given HRT in “later life” (avg. 76 years) increased their risk for dementia by 48%.
In summary, perimenopausal women stand to benefit greatly from HRT and may prevent the worst of symptoms while reducing their risk for more serious issues.
Could HRT Be Right for You?
There’s a lot of pseudoscience out there — saliva and urine home test kits that claim to check hormone levels, for example. Because hormone levels vary from day to day, sometimes hour to hour, according to your monthly cycle, those at-home tests are ridiculously unreliable.
Rather than wasting your time and money on those, schedule a serum test with your doctor and rely on them to interpret the results. We guide our patients through this process often, and we consider every individual’s risk-benefit ratio to make the best decision for them.
Hormone replacement therapy is, in general, a great thing — it keeps you young — and we want to remove the stigma based on a flawed, 20-year-old study. Many women should consider HRT for their health and longevity.
If you have more questions about HRT, contact Banner Peak Health. We’d be happy to chat with you.
How Accurate Is Your Apple Watch’s Heart Rate Monitor?
We live in an age of consumer-driven healthcare. COVID accelerated this, and tech companies have jumped on board to meet the public’s demand.
The Apple Watch is part of this trend, and although it sits at the intersection of entertainment and medical technology, we can’t dismiss its usefulness. The hype regarding the Apple Watch’s accuracy as a heart rate monitor isn’t as exaggerated as you might think.
The Apple Watch detects heart rate through photoplethysmography (PPG), a technique in which LEDs illuminate a capillary and read volumetric changes in the blood. It’s quite accurate when used to measure heart rate and blood pressure, and we can expect additional applications of this technology as it improves.
But just how accurate is the Apple Watch heart rate monitor? When I investigated, I found some impressive data.
Real Examples of the Apple Watch Heart Rate Monitor
So, how accurate is the Apple Watch heart rate monitor? Here are a few examples.
I’ve had two patients in their 40s rush to consult me after alarms on their Apple Watches went off, indicating atrial fibrillation (A-fib). A-fib is a condition in which irregular electrical activity at the top of the heart leads to poor blood flow. It’s notorious for causing stroke and heart failure.
After these patients showed me the data from their Apple Watches, I connected them with a cardiologist who treated them. At the time the alarm sounded, they weren’t feeling anything abnormal, but thanks to the Apple Watch, they received treatment and prevented a serious problem.
Note: While the FDA hasn’t approved the Apple Watch for diagnosing A-fib, the device has been cleared for monitoring A-fib.
Beyond personal experience, I’ve read many stories about people whose Apple Watches alerted them to abnormal heart rhythms, which allowed them to receive life-saving treatments.
For example, in 2018, a high school senior’s Apple Watch alerted her of a heart rate of 190 bpm (beats per minute). When she got it checked out, she discovered she was in renal failure. More recently, in 2021, a nurse was alerted that her heart rate was 40 bpm, which led her doctor to find an atrioventricular block.
The Apple Watch also has a “fall detection” setting, which automatically calls 911 if it detects a fall and the wearer doesn’t move for several seconds. This is a potentially life-saving feature for anyone with low blood pressure or a fainting condition, or for older people who might not be able to get up without help.
What Heart Health Data Points Does the Apple Watch Provide?
The Apple Watch can detect more than just your heart rate, but your heart rate alone can reveal much about your health.
For example, a low heart rate can indicate an atrioventricular (AV) block, as in the case we mentioned above. These patients, who are at a greater risk of fainting, often need a pacemaker.
Conversely, a high heart rate can indicate various issues, including pulmonary embolism and pericardial tamponade. A higher-than-normal resting heart rate also puts you at a higher risk of cardiovascular disease. Staying aware of these conditions can help you strategize with your doctor accordingly.
You can also use your Apple Watch to track your heart rate variability, which is a fitness indicator that varies from person to person. Again, discuss any concerns with your doctor.
Believe it or not, your Apple Watch can even record an EKG (electrocardiogram), sometimes also called an ECG. This test detects irregular heart rhythms and can indicate any number of issues, including atrial fibrillation (A-fib). (If you take an EKG with your Apple Watch and the results concern you, consult your doctor immediately.)
In 2019, the New England Journal of medicine published a study that followed 419,297 Apple Watch wearers over eight months. Eighty-four percent of irregular pulse notifications participants received during this time were accurate. That was four years ago.
This technology is constantly progressing. So, what about in 2023? How accurate is the Apple Watch heart rate monitor now?
How Accurate Is My Apple Watch Heart Rate Monitor?
How accurate is the Apple Watch heart rate monitor today? If you’re only checking heart rate, it’s quite accurate.
If you’re looking for other measurements, like certain arrhythmias, take the readings with a grain of salt and rely on your doctor’s advice — especially regarding ventricular arrhythmias, which the Apple Watch doesn’t identify reliably.
False positives can lead to anxiety and unnecessary ER visits. It’s best to contact your primary care physician and discuss your concerns, if possible, rather than run to the hospital — unless you physically feel that something is wrong. If it’s a true emergency, drop everything and go.
Remember, the Apple Watch, like any over-the-counter technology, has limitations and requires appropriate interpretation.
Today’s Takeaways
- Have your doctor verify and interpret all serious alerts and readings from your Apple Watch. However, the pros of wearing one far outweigh the cons.
- Pay attention to your symptoms and trust your body. If something doesn’t feel right, talk to your doctor, even if your Apple Watch doesn’t identify a problem.
- Monitor your readings over time and discuss them with your doctor. He or she will help you interpret the results.
Common Myths About Women’s Sexual Health You Should Stop Believing
Many of my peri- and postmenopausal patients believe diminishing sexual interest, drive, and enjoyment is a normal part of human aging. In fact, they’ve accepted it — which is why they’re so shocked when I tell them this is nothing more than a myth.
Why do so many women believe sex is only for the young? Well, there are many reasons.
Postmenopausal sex is a taboo subject, and it’s not discussed as much as it deserves to be. There also isn’t nearly enough funding for women’s health research. Women’s Health Initiative was a landmark study, but it fell short of collecting exhaustive data. (More on the shortcomings of the WHI in an upcoming post.)
The sore lack of research and a societal aversion to transparent conversations has led to rampant misinformation about women’s sexual health. It’s something I as a physician strive to change, starting with my individual patients.
The truth is, women can and should have fulfilling sexual lives well into their 60s, 70s, and even 80s. There are many ways we can support our sexual health as we age, and we’ll discuss some of them in this post — but first, we’ll explore the significant health benefits of maintaining your sexual health throughout your healthspan.
The Benefits of Supporting You or Your Partner’s Sexual Health
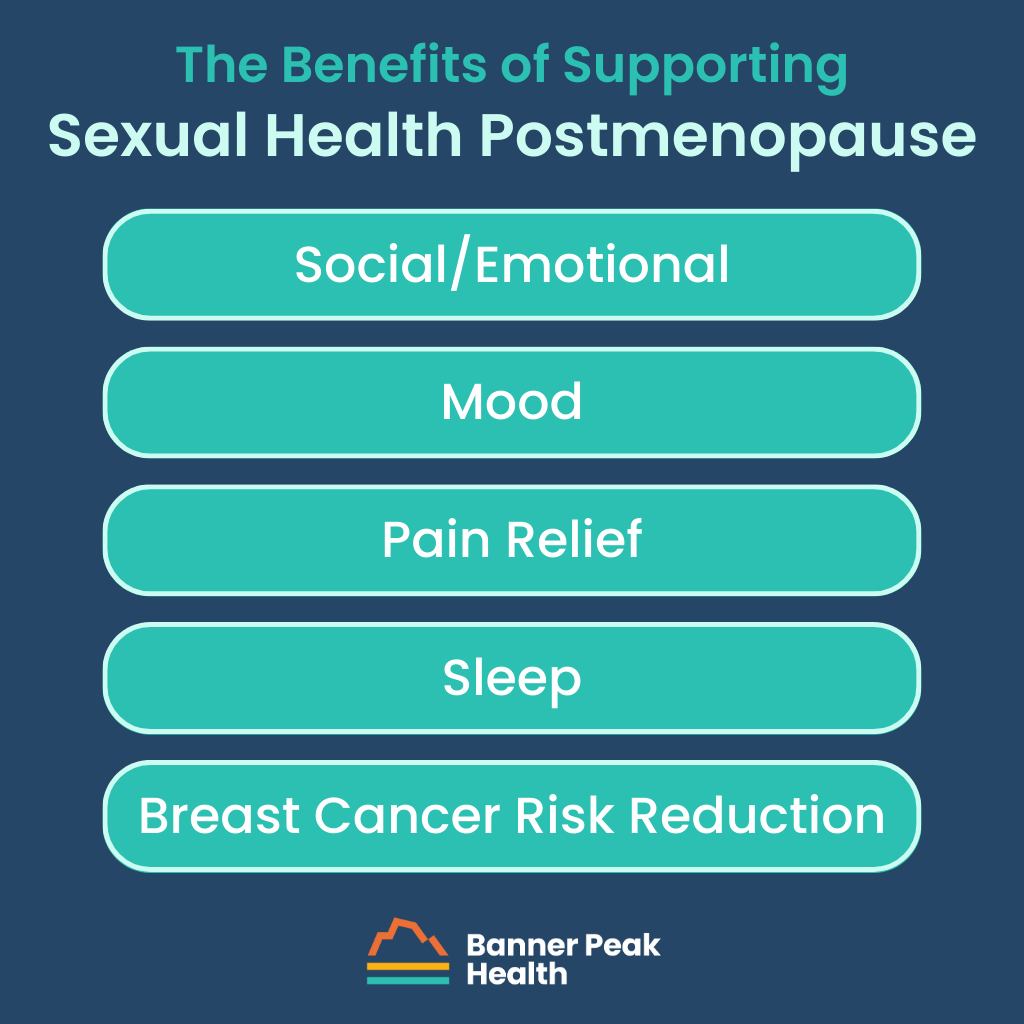
Social/Emotional
Our relationships do wonders for our overall happiness and quality of life, and a healthy sexual relationship is no different. Physical intimacy solidifies the bond you share with your partner.
Intercourse facilitates the synthesis and release of a cascade of hormones, including oxytocin and DHEA, which play an important role in bonding. It’s a deep feeling that’s difficult to quantify, but one we all recognize.
Mood
Studies have demonstrated that sexually mindful women have better self-esteem and tend to be more satisfied with their relationships.
Pain Relief
Sex releases endorphins, which help with pain reduction. Not only is preexisting physical pain subjectively less intense during intercourse, but the endorphins released via orgasm can reduce stress and alleviate pain.
Sleep
The hormones released during sex have also been shown to improve sleep. When you improve your sleep, other aspects of your health are impacted, such as your immune function, cardiovascular health, and mood.
For example, some studies have shown a 30% increase in IGA antibodies in sexually active people versus the abstinent control group.
Breast Cancer Risk Reduction
There’s even a study that demonstrates a risk reduction for breast cancer in women who had sex once a month versus women who didn’t.
Ways to Support Our Sexual Health as We Age
Generally speaking, women experience a decline in interest, drive, and enjoyment of sex during perimenopause and postmenopause due to estrogen loss. Hormone replacement therapy is the primary way we can address this.
In fact, this was the norm in the early 2000s, when one in four women was receiving hormone replacement therapy. But the medical community has since stopped using this therapy regularly, and today, only about 4% of women are receiving hormone replacement.
We should reconsider using this therapy for individuals who are a good fit. Of course, we need to take factors like clotting disorders and stroke risk into account, but that aside, hormones can generally be a good solution for many women.
Other ways to support women’s sexual health include exercise, diet, and carefully chosen supplements. Regular exercise boosts libido. Fruits such as apples, watermelon, and cacao have been linked to enhanced vascular and sexual health. Soy and low-salt diets also help.
The biggest point I want to drive home today is that, as a woman, you are entitled to a vibrant, fulfilling sexual life no matter your age. While it’s common to experience decreased interest, drive, and enjoyment, it’s not a permanent situation, and you don’t need to resign yourself to it.
Talk to your doctor or therapist about the challenges you’re facing. There are solutions available to you, and we’re here to help.
Today’s Takeaways
- The decline in sexual interest, drive, and enjoyment as you age is due to a natural loss of estrogen — but you don’t have to accept it.
- Depending on your individual risk factors, hormone replacement therapy may be a great option for you.
- Every woman, regardless of life stage, deserves a full, healthy, satisfying sexual life.