A Patient’s Guide to Statins for Cholesterol Treatment
High cholesterol is common — as is the question, “Do I need to take a statin?”
Despite their efficacy, statins get a bad rap. Cardiovascular disease remains the number one killer of Americans, even though it’s preventable. And still, my patients resist taking statins. I just don’t understand.
When we assess your risk for cardiovascular disease, we explore family history and other confounders, including smoking, high blood pressure, and diabetes. We can also perform a screening test to determine your coronary calcium score. This tells us whether you have calcified plaque in your arteries, indicating that cardiovascular disease is already present.
Beyond that, a MESA score can help us determine whether you’ll have a major heart event in the next 10 years.
Primary and Secondary Prevention
There are seven different statins available:
- Atorvastatin
- Fluvastatin
- Lovastatin
- Pitavastatin
- Pravastatin
- Rosuvastatin
- Simvastatin
Two (pravastatin and rosuvastatin) are more specific to the liver (hydrophilic), whereas the others are lipophilic and may cause more muscle-related side effects.
Statins work by blocking the enzyme that creates cholesterol. As the statins reduce the amount of LDL (low-density lipoproteins) in the blood, cholesterol and the amount of inflammation and plaque in the arteries also decrease.
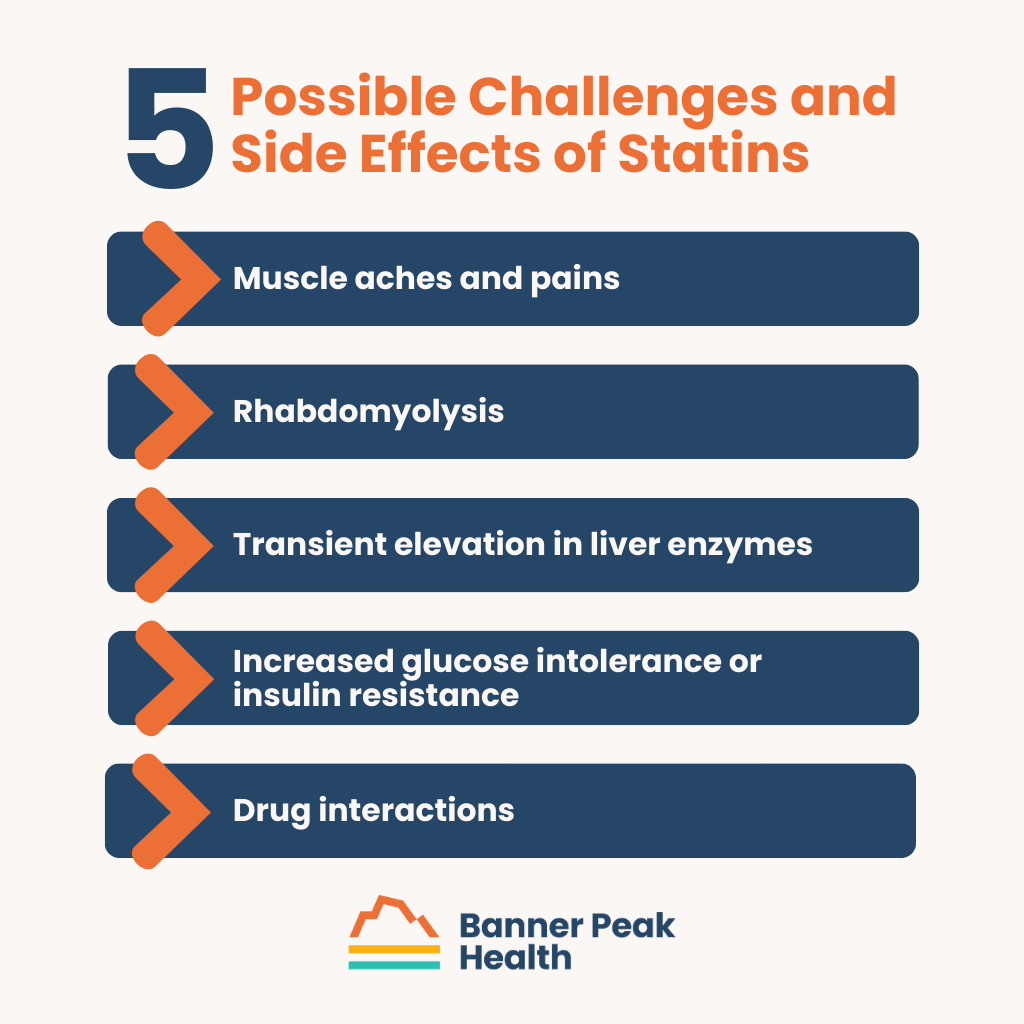
Possible Challenges and Side Effects of Statins
The following are side effects or challenges patients may experience when taking statins:
- Muscle aches and pains: These occur in 5–20% of patients.
- Rhabdomyolysis: This rare muscle breakdown can increase the risk of kidney failure.
- Transient elevation in liver enzymes: Similar to an allergic reaction, this occurs in 10–15% of patients but is completely reversible upon stopping the medication. A doctor monitors the patients’ liver enzymes for signs of elevation during the initial course.
- Increased glucose intolerance or insulin resistance: This can be problematic for diabetics.
- Drug interactions: Patients must avoid certain medications while taking statins, especially atorvastatin and simvastatin.
Not All Symptoms Are Side Effects
Aches and pains are a side effect of statins, but they’re also a normal symptom of aging. Don’t blame the aging process on your medicine.
A patient of mine recently stopped taking a statin due to minor aches and pains, only to experience a major cardiac event a few days later and wind up hospitalized. Don’t make the same mistake.
If You Need a Change, What Can You Do?
If you’re convinced you need to stop taking statins, you have options. First, talk to your doctor.
Alternative Statins
If you react badly to a certain statin, you can probably try a different one. Most side effects are not class effects; you could take another statin and experience none of the same issues.
It’s just a matter of finding the one that’s right for you.
Alternative Medications
Of course, if statins just aren’t right for you, some alternatives to statins don’t have the same side effects. Consider:
- Ezetimibe: Tablets that reduce the amount of cholesterol absorbed from the food you eat
- PCSK9 inhibitors: Two FDA-approved injectables administered every two to four weeks
- Bempedoic acid: Targets the liver, so patients experience fewer muscle aches
Today’s Takeaways
Medications like statins are another reason to have a close, conversational relationship with your doctor. A health advocate who understands your disease risks supports you and keeps you accountable.
If you’re at risk for the poor health outcomes associated with high cholesterol, you should take some kind of medication. Cholesterol is nearly impossible to control with diet alone. Genetics influences about 75% of your cholesterol, while food only influences about 25%.
The good news is that medication is extremely effective, and your doctor is available to help you. The sooner you start, the better.
The ABCs of Dementia and Alzheimer’s Prevention
Many people still believe dementia and Alzheimer’s are genetic diseases beyond our control. That’s not the case anymore. We can do more to prevent these issues than we ever thought possible.
More than six million Americans have Alzheimer’s, and we expect that number to double by the year 2050. Additionally, an estimated 47 million Americans are in the pre-clinical stages of Alzheimer’s disease but have yet to experience any noticeable symptoms.
These pre-clinical stages involve changes in the brain that occur 20–30 years before signs of mild cognitive impairment (like saying “I can’t find my keys” and then finding them in the fridge, etc.).
Currently, researchers are trying to define stage one of Alzheimer’s, which is challenging because it’s subclinical (meaning people who don’t have symptoms are at risk). Stage two is mild cognitive impairment, and stage three is dementia/Alzheimer’s.
Published dementia/Alzheimer’s research focuses on stage three, but we’ve seen very few benefits from the billions of dollars spent. Although Big Pharma would love to make a mint from selling a “silver bullet” for Alzheimer’s, success remains elusive. The drugs on the market offer little relief to patients.
As in most things, we at Banner Peak Health take the road less traveled and prefer an approach focused on how to prevent dementia and Alzheimer’s pre-onset. Fortunately, science is catching up.
How to Prevent (or Delay) Dementia and Alzheimer’s
One-third of Alzheimer’s cases are preventable. We can delay the onset of, or improve, the remaining two-thirds, which we hope to do until we find a “silver bullet.” Unfortunately, a minority group will be diagnosed with Alzheimer’s regardless of their efforts.
Doctors like Richard Isaacson lead the way, but prevention isn’t as attractive as finding a cure. Because prevention relies mainly on lifestyle changes, there’s no product to sell and no money to make (unlike with a miracle pill).
Lifestyle changes are also difficult to track and isolate. However, through precision medicine, we’ve noticed certain impactful markers. Let’s review the ABCs of how to prevent dementia and Alzheimer’s.
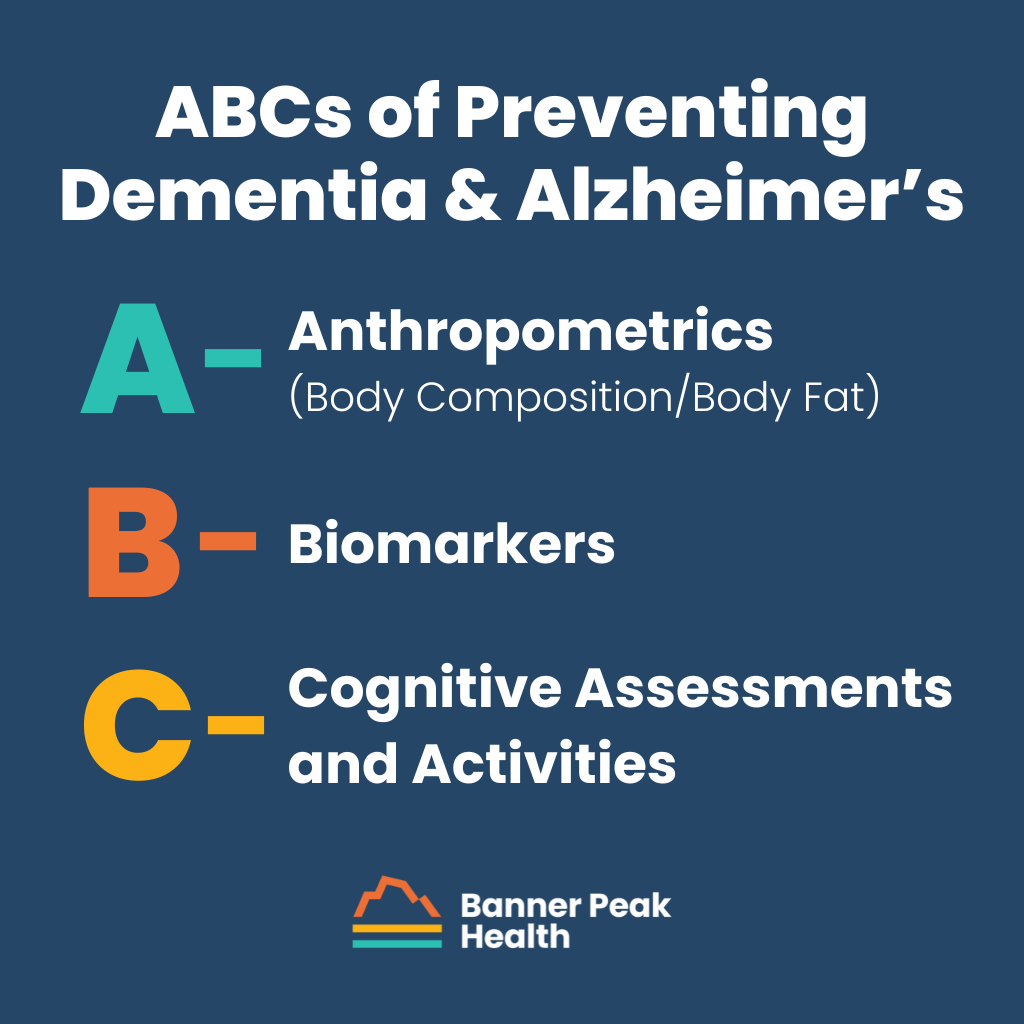
A: Anthropometrics (Body Composition/Body Fat)
We’ve found that the waistline is inversely related to the size of the hippocampus (the part of the brain related to memory). So, as your belly grows, your hippocampus shrinks, damaging your memory.
To optimize your capacity for memory as you age, engage in more cardiovascular and fat-burning exercise. HIIT (high-intensity interval training) burns fat, and studies have demonstrated a relationship between HIIT and memory.
B: Biomarkers
Biological markers, or biomarkers, serve as early warning signs of poor health. These include:
- Cholesterol
- Nutritional markers
- Homocysteine — high levels are injurious to the brain
- B vitamins — cofactors to reactions that help the brain
- Metabolic syndrome
- Blood sugar
- Blood pressure — the SPRINT study demonstrated that patients with lower BP have less cognitive decline
- Lipids/ApoB — should be as low as possible to make sure there are no vascular issues
- Insulin resistance in brain cells — it’s suspected that brain insulin resistance may cause or contribute to Alzheimer’s, unofficially termed “type 3 diabetes”
All these factors are within your control. Discuss each with your doctor and decide which are of most concern for you and how to best optimize your health.
The APOE Gene
You get one copy of the APOE gene from each parent. This gene has different types: APOE e2, APOE e3, and APOE e4.
- APOE e2 may protect against Alzheimer’s disease, and about 5–10% of the population has it.
- APOE e3, the most common variety of this gene, doesn’t affect Alzheimer’s disease.
- APOE e4 increases the risk of Alzheimer’s disease and is associated with early onset. If you have two of these genes, one from each parent, your risk for Alzheimer’s increases 8x–12x (2–5% of the population).
Knowing your risk is essential; you can find out through genetic testing. The more you know, the more intentional you can be about specific strategies on how to prevent dementia and Alzheimer’s.
C: Cognitive Assessments and Activities
Neuro-psych tests take about three hours to complete and cover short-term memory, long-term memory, spatial abilities, language ability, and fluency. Each subset of the test examines different parts of the brain for dysfunction.
After the test, you may be asked to take it again to gauge whether you can improve or reverse some cognitive impairment. You may receive some cognitive exercises to practice beforehand.
Activities like learning a new language, learning a new instrument, or learning how to ride a bike can have tremendous cognitive benefits. Regularly challenge yourself with puzzles or games, and engage in new activities.
How to Prevent Dementia and Alzheimer’s: Your Plan
Each person’s prevention plan is different, but tracking the anthropometrics listed above is essential for everyone. Monitor them and work with your doctor to outline a strategy that works for you. Proactively working to prevent dementia and Alzheimer’s is reliant on precision medicine and open, honest communication.
We All Self-Medicate for Stress — What Are YOU Reaching For?
Fill in the blank: “Today was a hard day. I need ___.”
What do you reach for? Exercise? Family time? Comfort food? A glass of wine? Pills?
Stress affects us all. I see it hurting my patients, my family members, and myself. We shouldn’t be ashamed to reach for something that helps us cope, but we must know when we’re reaching for the wrong thing — when the coping mechanism makes matters worse.
Healthy Coping
Healthy coping mechanisms keep you in control of yourself and leave you prepared to address your source of stress.
Here are some excellent coping methods you can try:
Box Breathing
This breathing technique activates your parasympathetic nervous system and curbs your vagal response.
Breathe in four-second increments. Inhale, hold your breath, exhale, hold your breath, and repeat.
5-4-3-2-1 (Grounding)
This technique uses your senses to return you to the present.
Name five things you see, four things you feel, three things you hear, two things you smell, and one thing you taste.
This technique’s simplicity makes it a great option for kids.
Exercise
Use moderate exercise to release the excess adrenaline that stress generates.
Journaling
Journaling can help reduce stress, among other benefits. You can even use your journaling session to plan a way to address the source of your stress.
Take a Break From Technology and Lean on Others
Practice being present (i.e., not distracted) by focusing on your immediate surroundings and connecting with other people. It’s easier to be present when you’re with another person.
It can feel challenging to admit you’re struggling, but you’ll almost always feel better when you open up to someone else. If you don’t want to talk about it, it’s still beneficial to simply spend time with others.
Practice Gratitude and Perform Acts of Kindness
Instead of dwelling on your stress, develop a list of five things going well in your life.
Performing acts of kindness also makes you feel good. There is a chemical component here (endorphin release), but this particular chemical makes you feel better and puts you in a healthy frame of mind.
Unhealthy Coping
It’s perfectly normal to reach for unhealthy coping methods because they work... for a while. Unfortunately, the relief is temporary.
Young, healthy, driven professionals are especially prone to unhealthy coping mechanisms. They don’t notice the damage of unhealthy coping like an older, less healthy person would.
Alcohol and Other Substances
Alcohol and other substances often dull the pain of stress. Many people reach for these “solutions” because they work — but only for a short time. Then, they lead to larger problems, like addiction.
Overeating or Undereating
Eating too much or too little harms our bodies and doesn’t resolve stress. In fact, it creates more problems and additional stress.
Avoidance
Avoiding the root of your stress by burying yourself in something else (e.g., work, social media, television, etc.) is escapism. It’s not helpful, and it’s becoming a massive trend.
Social Withdrawal
Interacting with others almost always relieves our stress, and isolation almost always makes it worse.
Aggression or Aggravation Toward Others
Hurting the people closest to you won’t eliminate your stress. It’ll only make you feel worse.
Turning your frustration toward loved ones creates cycles of retaliation and dysfunction. It’s confusing to the people who care about you. For example, your kids may not understand your anger and blame themselves. This can perpetuate dysfunction for generations.
Do You Need Help?
If your unhealthy coping mechanisms lead to depression, addiction, or physical or emotional harm (for yourself or others), rest assured that there are healthier options. Don’t be ashamed to talk to your doctor. This is part of being human.
This is one of the reasons I love practicing medicine in a concierge model. I have the time to explore these topics with my patients without feeling rushed. Together, we can devise a plan for healthy coping.
How to Treat the Winter Blues (SAD)
Around 15 million adults in the U.S. suffer from seasonal affective disorder (SAD), or “the winter blues,” every year. According to the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders — Fifth Edition), SAD isn’t its own entity. It’s a subset of depression or mania with a seasonal pattern.
If you meet five of the criteria for major depression and your symptoms present when days are short and nights are long and then improve when spring arrives, you probably have SAD.
Major depressive episodes are characterized by at least five of the following symptoms (over two weeks):
- Depressed mood; gloom; despair
- Loss of enjoyment of hobbies
- Sluggishness; fatigue
- Reduced appetite or increased food cravings and weight gain
- Insomnia or excessive sleep
- Lack of focus; brain fog
- Psychomotor changes (walking slower)
- Feelings of worthlessness or guilt
- Suicidal thoughts or ideation
Symptoms of seasonal depression subside every spring and recur in the fall. This pattern must repeat for at least two years to result in a diagnosis.

The Biology Behind SAD
Culturally, we’ve evolved to associate light with happiness and darkness with fear. However, biologically, our genetically-influenced circadian clocks determine how we respond to light and darkness.
Physiologically, it works the same way for all of us. The rods in our eyes detect sunlight and activate the retinal ganglion cells (RGCs). That signals the suprachiasmic nucleus, which tells the pineal gland to stop producing melatonin.
When we’re exposed to less light (such as during daylight savings time or the longer nights of winter), our bodies continue to produce melatonin, which encourages sleep. SAD is the biological consequence of hormonal dysregulation precipitated by less daylight.
How Common Is SAD?
Half the population may be vulnerable to SAD, but that doesn’t mean one in every two people suffers from it. One in 20 people, or around 5% of the population, is a more accurate estimate.
The incidence of SAD depends on geography. The closer you are to the equator, the longer the daylight hours, and the less likely you are to suffer from seasonal depression.
How to Identify SAD in Yourself
Mood disorders cause dysfunction in people’s lives, including excess stress, insomnia, increased blood pressure, and other metabolic parameters, though symptoms vary from person to person. Such changes can affect your job, relationships, and sleep.
Many people realize they’re affected by depression or some form of seasonal issue. However, many also explain their feelings away, dismissing them as:
- Holiday-related stress (seeing or not seeing relatives)
- Needing a vacation
- School-related stress (final exams, etc.)
- Cold weather/feeling “cooped up”
Don’t invalidate or minimize your feelings. Your biology causes them, and they deserve attention.

What to Do if You Think You Have SAD
First, talk to your doctor. They’ll ask questions and determine a diagnosis.
If you receive a SAD diagnosis, you may need to consider medication with your doctor. Light box therapy is also extremely effective and recommended to treat seasonal and non-seasonal depression, since it has no side effects.
A light box should have a minimum exposure of 10,000 LUX and should NOT emit UV light, which can cause skin damage.
Use a light box in the morning for 20–30 minutes within the first hour of waking. Keep the light box 16–24 inches from your face. Keep your eyes open, but don’t stare at it.
Typically, you’ll feel a difference within the first few days. Be aware of the other lights you’re exposed to in your home at night. It’s best to mimic a natural light cycle as much as possible — sunset, then starlight and moonlight.
This may sound gimmicky, but it works! Ask your doctor whether a light box is a good choice for you this winter season.
Sleep Apnea: More Than a Nighttime Annoyance
Sleep apnea is extremely common. Around a billion adults suffer from obstructive sleep apnea (OSA), and 80–90% of those cases remain undiagnosed.
OSA is a tip-of-the-iceberg illness, meaning many symptoms don’t seem noteworthy until they lead to more serious, dangerous conditions.
Today, I’m discussing what OSA is, what it looks like, and how to diagnose and treat it.
What Is Obstructive Sleep Apnea?
Everyone knows sleep is important for our health.
In deeper sleep stages, the muscles relax, including those in the back of the throat. Sometimes, the soft tissue there is floppy, either through heredity or because of excess weight. When the muscles relax, that floppy tissue briefly obstructs the airway.
When this happens, oxygen levels drop, and the brain signals the body to wake up. Although you may not wake up entirely, this cycle prevents you from remaining in deeper sleep stages.
Over time, this cycle of lost deep sleep causes hemodynamic changes that put you at greater risk for:
- High blood pressure
- Stroke
- Cardiovascular disease
- Memory loss
How Do You Know You Have Sleep Apnea?
A sleeping partner will become aware of a patient’s sleep apnea if they hear loud snoring and breathing pauses followed by gasping for breath. Other times, the patient experiences excessive fatigue, mental fog, and headaches, or feels unrefreshed upon waking.
In the long term, the lack of oxygen can also cause memory issues.
OSA Is the Tip of the Iceberg
On the surface, obstructive sleep apnea manifests as snoring or fatigue, which is nothing more than an inconvenience.
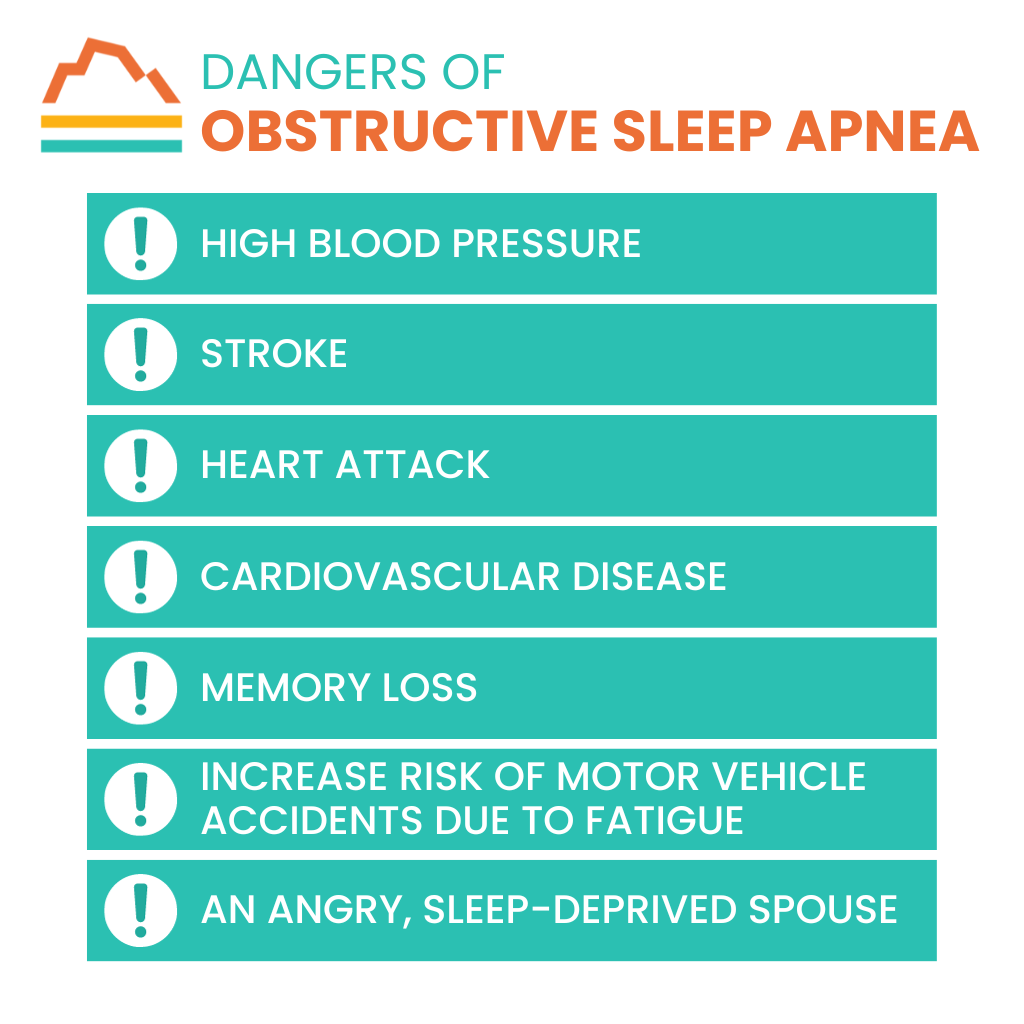
In reality, OSA can lead to more dangerous issues, including:
- High blood pressure
- Stroke
- Heart attack
- Cardiovascular disease
- Memory loss
- Increased risk of motor vehicle accidents due to fatigue
- An angry, sleep-deprived spouse
Never ignore the symptoms of sleep apnea.
Risk Factors of OSA
Risk factors for sleep apnea include:
- Being overweight
- Certain anatomy, like jaw structure, having a thicker neck, or having larger tonsils and adenoids
Although you can’t prevent heredity, losing 10% of your body weight can significantly improve sleep apnea symptoms if you’re overweight.
Some doctors recommend tonsillectomies, but surgery isn’t often the best solution for sleep apnea. It’s painful and tends not to be very successful.
Available Treatments
Don’t wait until you’re exhausted and experiencing severe symptoms to pursue help. If your partner notices apneic episodes, talk to your doctor. They’ll schedule a sleep study to confirm.
Once you’re diagnosed, your doctor will likely recommend you lose some weight.
A continuous positive airway pressure (CPAP) machine is another standard treatment for sleep apnea. Many people can find a mask that works for them and feel much better once they do. For those who can’t tolerate it, there are other options.
Dentists have created oral appliances that adjust your lower jaw forward just enough that when you relax into sleep, your airway isn’t obstructed. These appliances are effective for some patients.
Another option is a hypoglossal nerve stimulation implant. This is an excellent option for patients with sleep apnea who aren’t overweight. Two of my patients have them and are very happy with them.
Sleep apnea-correcting pillows are a solution for people who only suffer from sleep apnea when lying on their backs. The pillows keep the patient from rolling onto their back during sleep, preventing the position that causes OSA.
Finally, playing the didgeridoo (an aboriginal wind instrument that uses circular breathing) can effectively treat OSA, according to a study conducted in 2006. You can pick up a new hobby and treat your sleep apnea simultaneously.
Today’s Takeaways
Don’t be the Titanic. When you see the tip of the iceberg, don’t wait to take action. Talk to your doctor and schedule a sleep study. Sleep (and your health) is too important to risk.
We’re here when you need us. Just give us a call.
Why Is My Hair Falling Out So Much? (Hair Loss in Men and Women)
One in three women asks her doctor about hair loss at some point.
Although hair loss is often considered more acceptable in men, women are almost as susceptible and often more emotionally impacted. They ask, “Why is my hair falling out so much?” “Will I need a wig?” “Am I going bald?”
The physical causes of hair loss range, and while hair loss can indicate a serious condition, it often doesn’t. Still, it’s essential that your doctor address all your questions and concerns.
I’ll try to answer the most common questions about hair loss in this blog post.

Types of Hair Loss
We generally divide hair loss into two categories: patchy and diffuse.
Patchy Hair Loss
Patchy hair loss occurs only in specific areas. It has two causes:
- Scarring: A rash (usually caused by a fungal infection), psoriasis, or discoid lupus leaves scarring, which inhibits hair growth.
- Non-Scarring: Also called alopecia areata, this kind of patchy hair loss is believed to be autoimmune and is fairly simple to diagnose.
Diffuse Hair Loss
Diffuse hair loss occurs over the entire scalp but begins on the crown and front. People refer to this as “thinning hair” or to their scalp getting “wider.” Causes of diffuse hair loss include:
- Androgenic Alopecia: This is classic “male-pattern baldness,” though it can also occur in women and commonly does (especially in women with a family history).
- Telogen Effluvium: This is the most common form of hair loss in women. All hair follicles synchronize, and most or all hair falls out simultaneously. Hormonal changes from pregnancy, thyroid disease, iron deficiency, and other physical or psychological stressors trigger telogen effluvium.
- Anagen Effluvium: Unlike telogen effluvium, anagen effluvium isn’t natural. Chemical damage like chemotherapy or exposure to heavy metals (mercury, arsenic, etc.) causes this condition.
- Topical Chemical, Heat, or Traction-Related Damage: Tying long hair back into braids or ponytails that are too tight, excessive heat from hairdryers and flat irons, and chemical damage from dyes cause this type of hair loss.
Identifying the Cause
The first step in treating hair loss is to determine the cause. When a patient asks, Why is my hair falling out so much?, I first consider their personal history, their family history, and the timeline and pattern of their hair loss.
Beyond that, the following tests can help in certain situations:
- A biopsy can determine the cause of patchy hair loss.
- Blood tests will identify hormonal changes (e.g., thyroid disease) and vitamin or mineral deficiencies (e.g., iron).
- A hair pull test determines the severity and, therefore, the type of hair loss.
- Using a folliscope, a doctor examines a hair’s structure to help determine the cause of the loss.

Traditional Treatments
Once the cause of your hair loss is determined, your doctor can begin treatment. The following treatments have been used for several years to treat hair loss in both men and women:
Iron Supplementation
If the cause of your hair loss is iron deficiency, we treat it with iron supplementation.
Thyroid Hormone Replacement
We treat thyroid disease with thyroid hormone replacement, which enables hair to regrow.
Hair Transplants
Hair transplants have been used to offset hair loss for many years but are costly, painful, and questionable in efficacy.
Treatments Exclusive to Androgenic Alopecia
Many women have polycystic ovarian syndrome (PCOS), which causes excessive testosterone that metabolizes into dihydrotestosterone (DHT). DHT harms hair follicles and leads to hair loss. Androgen blockers for PCOS help reduce DHT-related damage to hair follicles.
Oral spironolactone has effectively treated both men and women, especially when combined with minoxidil.
Women who won’t become pregnant and men may use the following treatments to treat androgenic alopecia:
- A low dose of oral finasteride can effectively prevent hair from falling out but doesn’t regrow hair.
- Minoxidil, the primary ingredient in Rogaine, has been used as a hair loss treatment for decades but is perhaps only 40% effective. It’s also inconvenient; most patients stop using it before seeing results.
New Treatment Options
Oral Minoxidil
Oral minoxidil, not to be confused with topical minoxidil, is an old blood pressure medication. It’s now used orally in low doses to prevent androgenic alopecia in males and females. Its efficacy in regrowing hair is impressive.
PRP (Platelet-Rich Plasma) Injections in the Scalp
PRP injections have shown promise as a treatment for hair loss, but their use is currently off-label. They’re also painful and short-acting.
Today’s Takeaways
- If you’re losing hair, pay attention to it. Know your history.
- Most of the time, we can diagnose hair loss by knowing its timeline and pattern and by doing bloodwork.
- Most of the time, especially for women, it’s telogen effluvium.
- Talk to your doctor. Don’t be afraid to ask, “Why is my hair falling out so much?”
Meditation for Anxiety and Stress: What You Need to Know
These days, life moves too quickly.
Stress and anxiety have become so common that we often accept them as normal. When we do, we face dire consequences at work, in our personal relationships, and in our mental and physical well-being.
You don’t need to endure constant stress. There are solutions out there. Meditation for anxiety and stress is a great place to start.
Meditation Over Medication
One of the most effective solutions to chronic stress isn’t a quick fix, and it isn’t pharmaceutical. It involves a lifestyle change.
Meditation for anxiety and stress has proven effective for millions of people. Beyond lower stress levels, benefits include:
- Lower resting heart rate
- Lower blood pressure
- Better sleep quality
- Better immunity (especially if you have a disease affected by stress)
- Lower anxiety and depression
I can’t discount the emotional benefits of meditation, either. It improves patience and tolerance of others and boosts creativity and imagination.
How to Begin Meditation for Anxiety and Stress
Each type of meditation has a different goal: calming the mind, clarifying thoughts, finding emotional peace, creating connections, etc. Meditation was once a strictly spiritual practice, but today, it’s used more pragmatically.
Whichever type you decide to practice, the benefits are real. Decide on your goal, and match that with the type of meditation that’ll best help you reach your goal. These include:
- Mindfulness
- Transcendental Meditation
- Movement Meditation (Tai Chi or Yoga)
- Buddhist Meditation
For people with anxiety and depression, meditation that calms the mind may be challenging. Start with a meditation style that focuses on the heart rather than the mind.
For example, the following heart-focused meditation is often helpful for people with chronic anxiety who have trouble calming down:
Picture the inside of your heart as an egg. Imagine there’s a light inside that radiates through your body. The egg shatters, and the light of love and goodness extends to all the people you love. Then to all the people you know. Then to all people.
A heart-centered meditation for anxiety and stress can lead to deep inner peace.
First Steps
When you meditate, follow these best practices:
- Get as comfortable as possible. Remember, you’ll be in one position for some time.
- Maintain peaceful quiet. You don’t have to remain still — you can meditate while walking.
- Don’t “start small.” Meditate as often as possible to build a habit.
Two Calming Techniques to Try Today
There are two meditative practices you can start right away: autogenic training and box breathing.
Autogenic Training
I learned this in med school and still use it today. You’ll find it on most guided meditation apps.
It’s a remarkable technique my teacher combined with Pavlovian classical conditioning, and 30 years later, I still respond to the signals. Simply pinch your earlobe or press two fingers together when you listen to the guided meditation.
After enough repetitions, an unconscious association forms between that pinch and the relaxation the meditation accomplishes. Just like Pavlov’s dog and the bell, you’ll relax by simply pinching your earlobe.
Box Breathing
Practice box breathing when you’re feeling anxious. It activates your parasympathetic nervous system and curbs your vagal response. Soldiers even use it in combat.
Simple and effective, you breathe in four-second increments. Inhale, hold your breath, exhale, hold your breath, and repeat.
Final Thoughts on Meditation for Anxiety and Stress
Mental illness’s grip on society tightens each day. Meditation for anxiety and stress has helped people find peace for millennia. Try it yourself.
If you’re struggling, talk to your doctor or contact us at Banner Peak Health so we can tailor a solution for you.
7 Things to Do Before Traveling Internationally
Four of my cousins operate a charity hospital in India. Whenever I visit to help out, I take prophylactic malaria medication on Sunday mornings.
One Saturday night, I started shaking, had a 103-degree fever, felt my liver and spleen, and thought, “Oh, great, I have malaria.” I took the pill I would’ve taken in the morning that night, and by the morning, I was well.

Even though I’m a doctor and prepared for everything, I still got sick, which could’ve been disastrous. That’s why taking certain steps to minimize your risk of illness when traveling abroad is critical.
Specifically, there are seven things to do before traveling internationally to ensure you have a healthy trip.
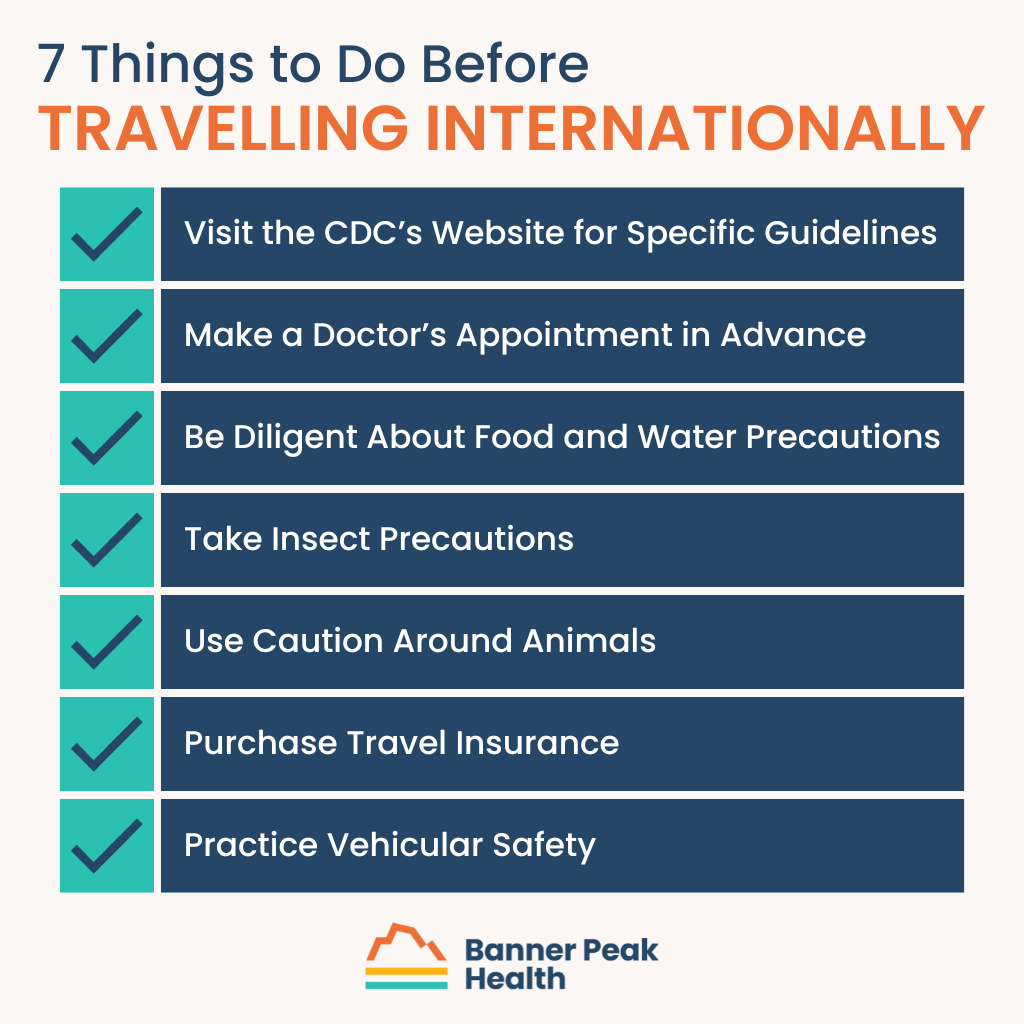
1. Visit the CDC’s Website for Specific Guidelines
The first thing to do before traveling internationally is something you should do as soon as you pick your destination.
The Centers for Disease Control and Prevention (CDC) has a fantastic international travel resource. Choose your destination from their digital list and review the recommended vaccines. You’ll also find information on diseases not preventable by vaccine, such as malaria.
2. Make a Doctor’s Appointment in Advance
The second thing to do before traveling internationally is to see your primary care physician at least four to six weeks before you leave for your trip.
It takes time for vaccines to work and for your body to build immunity. For example, if you’re traveling to Asia, you’ll want full immunity from typhoid and hepatitis A vaccines, which means getting them four to six weeks in advance.
You’ll also need to get any necessary prescriptions and receive instructions on how to take them. Remember my story about the malaria medication I took? If you’re going somewhere where you’ll need a similar medication, you’ll need to get the drug and ask your doctor how to take it.
3. Be Diligent About Food and Water Precautions
If you’re traveling to a third-world country, be diligent about food and water. Avoid raw foods, including raw vegetables, unless you can wash them in boiled or distilled water.
Also, avoid cooked foods served at room temperature. When cooked meat cools, bacteria multiply. Temperatures of 40–140℉ are dangerous.
Always ensure water is boiled or distilled, and only drink water from sealed bottles. In poor countries, people sometimes refill water bottles with local water to sell to tourists. Do not drink water from a container that’s not properly sealed.
Also, avoid ice. It’s easy to overlook — I forgot once myself and ended up with traveler’s diarrhea because I had a drink made with ice frozen from local water.
Local water can cause waterborne illnesses like typhoid, E. coli, parasites, and traveler’s diarrhea. These are serious, sometimes fatal illnesses, and quality medical care isn’t always available overseas.
4. Take Insect Precautions
If you’ll be camping or spending time in the jungle, treat your clothes and gear with permethrin in advance.
Wear insect repellent and cover exposed skin. There are several effective repellent ingredient options to choose from:
- Deet
- The only ingredient proven effective against ticks, which can transmit Lyme disease
- Concentrations over 50% show no additional protective benefit
- Picaridin
- Repels mosquitoes, biting flies, ticks, fleas, and chiggers
- Needs to be reapplied more often than Deet
- Oil of Lemon Eucalyptus (Paramenthane-3,8-diol)
- Natural botanical that repels mosquitoes
- IR3535
- Repels mosquitoes and black-legged ticks
When wearing both sunscreen and insect repellent, apply sunscreen first, then repellent.
You may need to use a bed net to keep mosquitoes and biting flies at bay while sleeping. Bed nets help prevent malaria, yellow fever, dengue fever, chikungunya fever, and more.
5. Use Caution Around Animals
Americans generally take exceptional care of their pets, but pet owners in other countries don’t always practice the same standards.
Aside from obvious risks like African safaris or swimming with sharks, seemingly “harmless” animals, even pets, can cause rabies. Rabies leads to over 59,000 deaths worldwide annually, with 95% occurring in Asia and Africa. If you get bitten or scratched while traveling, immediately clean the wound with soap and seek medical attention.
Smaller creatures also pose a threat. Watch out for arthropods (insects and arachnids, including spiders, ants, and ticks), scorpions, and snakes. These largely depend on where you’re traveling, but always practice caution.
6. Purchase Travel Insurance
One helpful thing to do before traveling internationally is purchase travel insurance. This includes specific types of insurance, such as medical evacuation insurance, in case you contract a dangerous illness or are seriously injured and local medical care doesn’t meet U.S. standards.
7. Practice Vehicular Safety
Motor vehicle accidents are the number one killer of healthy U.S. citizens on foreign soil. Don’t underestimate how different driving is abroad.
For instance, in India, cars, bikes, rickshaws, buses, and trucks share the same road. It can be chaotic and dangerous if you’re unfamiliar with those conditions.
Choose safe vehicles. Avoid motorbikes. Don’t drink and drive or ride with a driver who’s been drinking. Always wear seatbelts and helmets (if applicable). Avoid driving at night, as the lighting can be poor.
Choose larger aircraft (more than 30 seats) whenever possible when flying. Avoid local or unscheduled aircraft, as those pilots may not meet U.S. standards.
What to Include in a Travel Kit
If you consult us ahead of time, we’re happy to help you prepare a travel kit containing basic items appropriate for your destination, such as:
- Sterile gauze
- Ace wrap
- Alcohol swabs
- Antibacterial ointment
- Tylenol
- Advil
- Benadryl
- Topical steroid
- Imodium
- Dramamine
- Antibiotics (in case of traveler’s diarrhea)
Also include your usual medications (in adequate quantities), an EpiPen if you have a history of anaphylaxis, and an extra pair of contact lenses or eyeglasses.
When you speak with your physician, bring your itinerary. Discuss specific activities and destinations so your doctor can help you fully prepare.
Remember, the best time to consult your physician is four to six weeks before your trip, so you can cover everything you need to do before traveling internationally. Call Banner Peak Health to schedule an appointment as soon as you finalize your travel plans.
What Is the Relationship Between Stress and Memory?
Stress is a loose concept. It refers to anything that disrupts a person’s homeostasis or to a condition people experience when demands exceed their resources.
It can be external (extreme temperatures or physical discomfort) or internal (anxiety). Your coping skills and how much control you have over your circumstances both contribute to your experience of stress.
For example, if you were in freezing temperatures but had a warm coat, you’d be less stressed than if you were only wearing a T-shirt. Or, if you were in an uncomfortable social situation and unable to leave, you’d experience more stress than if you could exit.
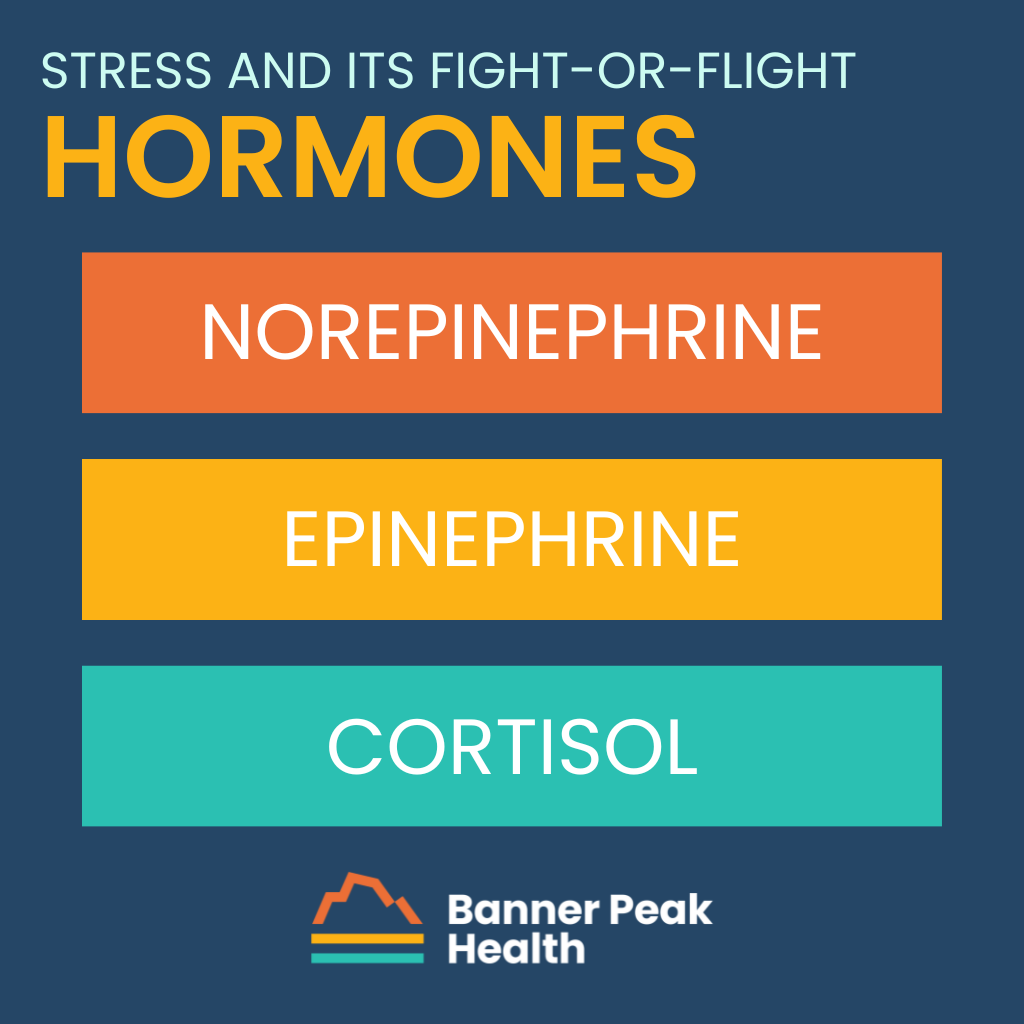
When under stress, your body produces stress chemicals and hormones, including norepinephrine, epinephrine, and cortisol, triggered by the sympathetic nervous system (norepinephrine, epinephrine) and the HPA (hypothalamus-pituitary-adrenal) axis (cortisol). These chemicals and hormones engage your body in “fight or flight” mode, which is why you feel stressed. It’s an evolutionary response to danger.
Stress and Memory
Depending on whether it is acute or chronic, stress affects memory in various ways.
While the human physiologic response to acute stress enhances learning and short-term memory recall, chronic stress is harmful to the acquisition, consolidation, and retrieval of information.
How Does the Brain Respond to Stress?
High cortisol levels particularly affect long-term memory (retrieval) due to cortisol’s harmful effects on the hippocampus, where the brain stores long-term memory.
States of chronic stress often enhance emotional memory recall because the amygdala or primitive brain centers are favored when chronically stressed. This is linked to survival, and explains why facts are often more difficult to recall than feelings when people are in situations where they experience chronic stress.
Our feeling memories and our thinking memories are stored in different parts of the brain depending on how chronically stressed and activated we are.
The Significance
The practical importance of understanding how chronic stress relates to and affects memory is important because it helps us understand the need to return to homeostasis.
Managing stress while learning to maximize memory retention for school, work, and life is crucial. When we begin to see that our memory is suffering as a result of chronic stress, it motivates us to take action to balance our flight-or-flight response with rest, supporting our parasympathetic nervous system. In fact, I would like to introduce a new term: parasympathize.
Some Ways to Parasympathize
- Manage your stress by controlling the controllable.
- Practice recognizing when you’re in “activated” states of stress (i.e., fight or flight).
- Follow stress management best practices:
Following these suggestions will prevent chronically elevated cortisol levels, which is better for your overall health (AKA, homeostasis).
The Connection Between Childhood Trauma and Physical Illness
Would it surprise you to learn that many chronic illnesses — especially ones without a direct physical cause — are linked to childhood trauma?
Childhood trauma causes the nervous system to develop differently. While we’re still learning about this process, it’s clear there are legitimate, debilitating physical effects of childhood trauma in adulthood.
Defining Childhood Trauma
We define childhood trauma using the same criteria the CDC-Kaiser ACE Study put forth. ACE is an acronym for adverse childhood experiences. These equate to traumatic experiences and include three categories: abuse, household dysfunction, and neglect.
- Abuse can be emotional, physical, or sexual.
- Household dysfunction includes substance use disorders, mental illness in the home, parental separation or divorce, and incarceration of a household member.
- Neglect be emotional or physical.
Aside from bearing the effects of childhood trauma in adulthood, adults can experience new trauma, too. For example, the COVID pandemic was a source of trauma for many adults worldwide.
The Mind-Body Connection and How We Process Pain
The brain’s complex design dedicates parts of itself to rational thought and other parts to primitive survival instincts. We sometimes refer to these parts as our “thinking brain” and “feeling brain,” respectively.
Our feeling brain is where our brain perceives threats in our environment and makes instinctual decisions that keep us alive. This is the fight-or-flight center of the brain.
When we talk about repressed memories, this is the part of the brain we’re referring to. Because those memories connect to experiences too overwhelming for the thinking brain, we store them in the feeling brain.
Triggers are a way to access them.
For example, say you had a terrible experience sometime in the past, and during that experience, a certain type of food was cooking.
Later, you smell that food and suddenly feel terrible but don’t know why. That’s your feeling brain accessing your repressed memory as a result of that trigger — the same smell.
The olfaction is an association your brain formed during the trauma. That association is a trigger that unlocks the memory, but you’re not conscious of it because it exists in your feeling brain rather than your thinking brain.
It’s a form of classical conditioning similar to Pavlov’s dog.
This phenomenon can happen with physical pain, too. Sometimes, if a child suffers an injury as a result of abuse, they may not experience all the associated physical pain because it would just be too overwhelming.
Their brain locks it away to keep the child safe and alive, but that pain gets triggered later in life because the nervous system remembers it from before. This is one of the many effects of childhood trauma in adulthood.
Effects of Childhood Trauma in Adulthood
When the brain and body know it’s safe, they try to process the physical and emotional pain inflicted years before, but the rational mind doesn’t understand where the pain suddenly comes from. This is why adult victims of childhood trauma often tell their doctor, “I have all these things wrong with me, and I don’t know why.”
Physical effects of childhood trauma in adulthood often include GI symptoms like irritable bowel syndrome (IBS). They can also include overactive bladder, fibromyalgia, and inflammation and muscle pain (muscle knots).
When you better understand the effects of childhood trauma in adulthood, you can begin to process them and begin your journey to recovery.
If you have a history of childhood trauma (as defined above by the CDC-Kaiser study) and experience the symptoms we’ve described, now might be the right time to deal with it.
Those things that were once protective no longer serve you. They kept you alive in environments that weren’t nurturing, but now that you’re safe, they’ve come to the surface for a reason. It’s a sign to address them appropriately.
How to Address the Effects of Childhood Trauma in Adulthood
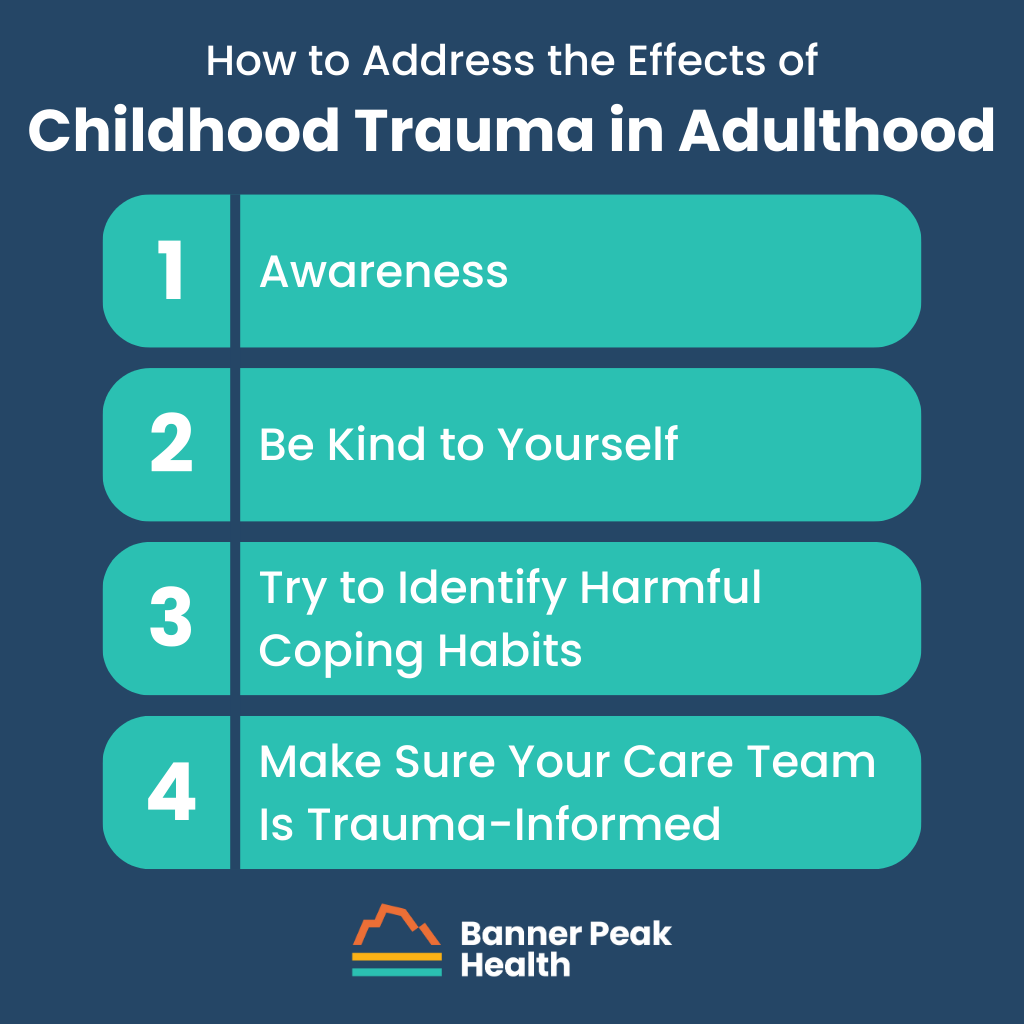
Ready to address the effects of childhood trauma in adulthood? Here are four steps we recommend to get started.
Step 1: Awareness
Many journeys of recovery begin with a step of admission or acceptance. This one is no different.
You must admit the possibility that what you’re experiencing is real. It’s not just “in your head.” It’s programmed into your nervous system.
Unfortunately, many doctors tell adult victims of childhood trauma that their symptoms are all in their heads or just a result of anxiety or depression. But anxiety is a symptom, not a disease, and it’s likely a reaction to pain that has been inflicted but hasn’t been appropriately processed.
Step 2: Be Kind to Yourself
Understand that your body was and is trying to help you survive — and you did. Your body isn’t against you. It protected you in extraordinary ways.
Trauma is not the event; trauma is the response to the event. Overcoming trauma is not about removing the event. You can’t undo the past.
Trauma is part of our survival response. It’s extraordinary the way the human body stores information with the understanding that it will be processed later, when it’s safe to do so. When we see it this way, we empower ourselves to change our perspective from weakness to strength.
Honor your authentic self. You survived.
Step 3: Try to Identify Harmful Coping Habits
Healing from trauma isn’t easy; sometimes, we reach for things that aren’t in our best interests. Identify unhealthy habits and either reduce, quit, or ask for help to quit.
It can be helpful to find an alternative (healthy) coping mechanism to turn to when you feel triggered or stressed.
Step 4: Make Sure Your Care Team Is Trauma-Informed
As doctors, our standard training does not make us trauma-informed. That leaves the onus on you to find medical professionals who are trauma-informed.
When you’ve experienced the effects of childhood trauma in adulthood or are processing those effects, you need a trauma-informed care team.
If you’d like help finding a trauma-informed care team or want to know more about becoming a member here at Banner Peak Health, reach out. We’d be happy to speak with you.