In the 1940s, the medical community introduced the idea of giving menopausal women estrogen to combat their symptoms. Twenty years later, the FDA approved the first estrogen pill.
For the next few decades, supplemental estrogen was generally seen as positive. Observational studies in the 1980s and 90s even suggested a decreased risk of cardiovascular disease in women receiving hormone replacement therapy (HRT). In 1992, a randomized controlled study called the Women’s Health Initiative (WHI) set out to determine once and for all if and how women benefit from HRT.
The WHI planned to follow 27,347 women between the ages of 50–79 over 13 years. The average participant was 63 — a significant limitation, considering the study didn’t take into account a younger population of perimenopausal women.
The results of the WHI shocked the medical community: for the population studied, HRT didn’t protect from heart disease and resulted in an increased risk of breast cancer. Doctors spent the next few decades making recommendations based on this study’s results.
We’re just now beginning to realize how flawed the WHI was. It omitted a significant portion of the population — perimenopausal women, who, as recent investigations suggest, benefit the most from HRT.
The medical community has spent the 2020s reevaluating the benefits of HRT for perimenopausal women.
‘The Change’ and How Hormones Can Help
During perimenopause and menopause, estrogen and progesterone levels in the body drop and cause vasomotor symptoms (hot flashes, night sweats, and sleep disturbances).
Loss of estrogen can cause loss of bone and muscle mass, mood changes, difficulty concentrating, and loss of sexual function and libido. Sleep disturbances in particular create a cycle that increases other health risks, such as cardiovascular disease and diabetes.
Recent investigations show vasomotor symptoms must be treated by HRT within 10 years of onset for the best results and the best chance of preventing osteoporosis.
Types of HRT
There are several types of HRT, and each requires specificity. For example, if you have an intact uterus (i.e., have not had a hysterectomy), you would need to take progesterone in addition to estrogen to minimize the risk of uterine cancer, endometrial hyperplasia, and endometrial cancer.
Years ago, HRT was usually given orally. Since then, technology has developed many convenient and effective ways to deliver hormones.
Depending on their doctor’s recommendations, women can choose from oral pills, topical preparations, implanted subdermal pellets, or transdermal patches. Transdermal patches in particular are gaining popularity because they tend to cause fewer side effects than other methods. Specifically, they don’t tend to raise cholesterol as much as oral pills.
Risks vs. Benefits
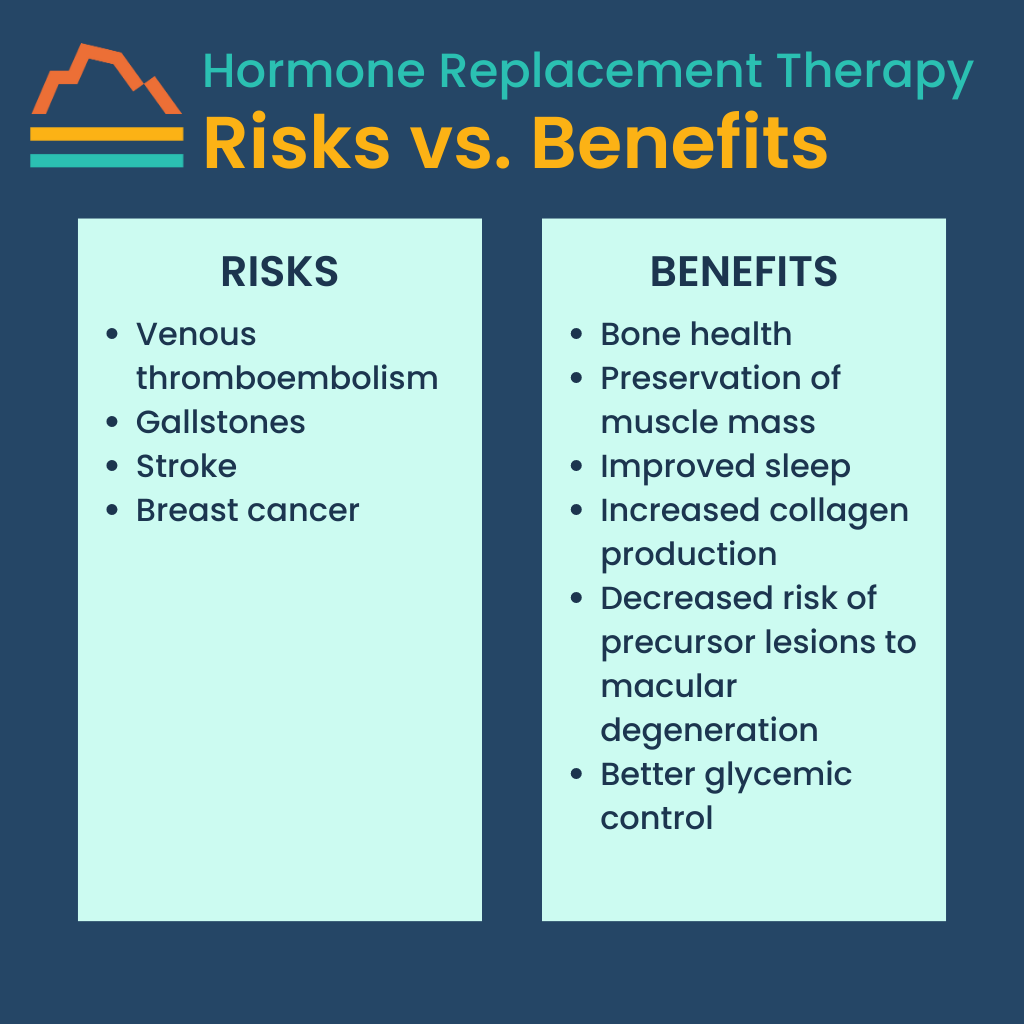
Although HRT can effectively reduce the symptoms of perimenopause, it’s not right for everyone. It can cause a risk of venous thromboembolism, gallstones, and stroke, and a very slightly increased risk (0.0009%) of breast cancer. Women who have a family history of blood clots may be encouraged to avoid HRT altogether.
However, for most women, the benefits of HRT far outweigh the potential risks. The most common benefits include bone health, preservation of muscle mass, improved sleep, and increased collagen production. In African American women, HRT may also decrease the risk of precursor lesions to macular degeneration.
For women with diabetes, HRT may lead to better glycemic control — though because of an inherent increased risk of heart disease, women with diabetes must be carefully selected for HRT to avoid unnecessary risk.
The key is treating women early. Once a woman goes through menopause, HRT is no longer effective in treating symptoms or reducing the risks for these conditions. It can even be detrimental.
In one study, women treated with hormone replacement during “mid-life” (avg. 48.7 years) saw their risk for dementia decrease by 26%. However, women given HRT in “later life” (avg. 76 years) increased their risk for dementia by 48%.
In summary, perimenopausal women stand to benefit greatly from HRT and may prevent the worst of symptoms while reducing their risk for more serious issues.
Could HRT Be Right for You?
There’s a lot of pseudoscience out there — saliva and urine home test kits that claim to check hormone levels, for example. Because hormone levels vary from day to day, sometimes hour to hour, according to your monthly cycle, those at-home tests are ridiculously unreliable.
Rather than wasting your time and money on those, schedule a serum test with your doctor and rely on them to interpret the results. We guide our patients through this process often, and we consider every individual’s risk-benefit ratio to make the best decision for them.
Hormone replacement therapy is, in general, a great thing — it keeps you young — and we want to remove the stigma based on a flawed, 20-year-old study. Many women should consider HRT for their health and longevity.
If you have more questions about HRT, contact Banner Peak Health. We’d be happy to chat with you.

Waheeda Hiller, MD
For over 20 years in Internal Medicine, Dr. Hiller has dedicated herself to providing unparalleled care to patients. She joined Banner Peak Health in 2023 as a concierge physician to better serve patients with the depth of thought, knowledge, and compassionate care they need to live the healthiest lives possible.