High cholesterol is common — as is the question, “Do I need to take a statin?”
Despite their efficacy, statins get a bad rap. Cardiovascular disease remains the number one killer of Americans, even though it’s preventable. And still, my patients resist taking statins. I just don’t understand.
When we assess your risk for cardiovascular disease, we explore family history and other confounders, including smoking, high blood pressure, and diabetes. We can also perform a screening test to determine your coronary calcium score. This tells us whether you have calcified plaque in your arteries, indicating that cardiovascular disease is already present.
Beyond that, a MESA score can help us determine whether you’ll have a major heart event in the next 10 years.
Primary and Secondary Prevention
There are seven different statins available:
- Atorvastatin
- Fluvastatin
- Lovastatin
- Pitavastatin
- Pravastatin
- Rosuvastatin
- Simvastatin
Two (pravastatin and rosuvastatin) are more specific to the liver (hydrophilic), whereas the others are lipophilic and may cause more muscle-related side effects.
Statins work by blocking the enzyme that creates cholesterol. As the statins reduce the amount of LDL (low-density lipoproteins) in the blood, cholesterol and the amount of inflammation and plaque in the arteries also decrease.
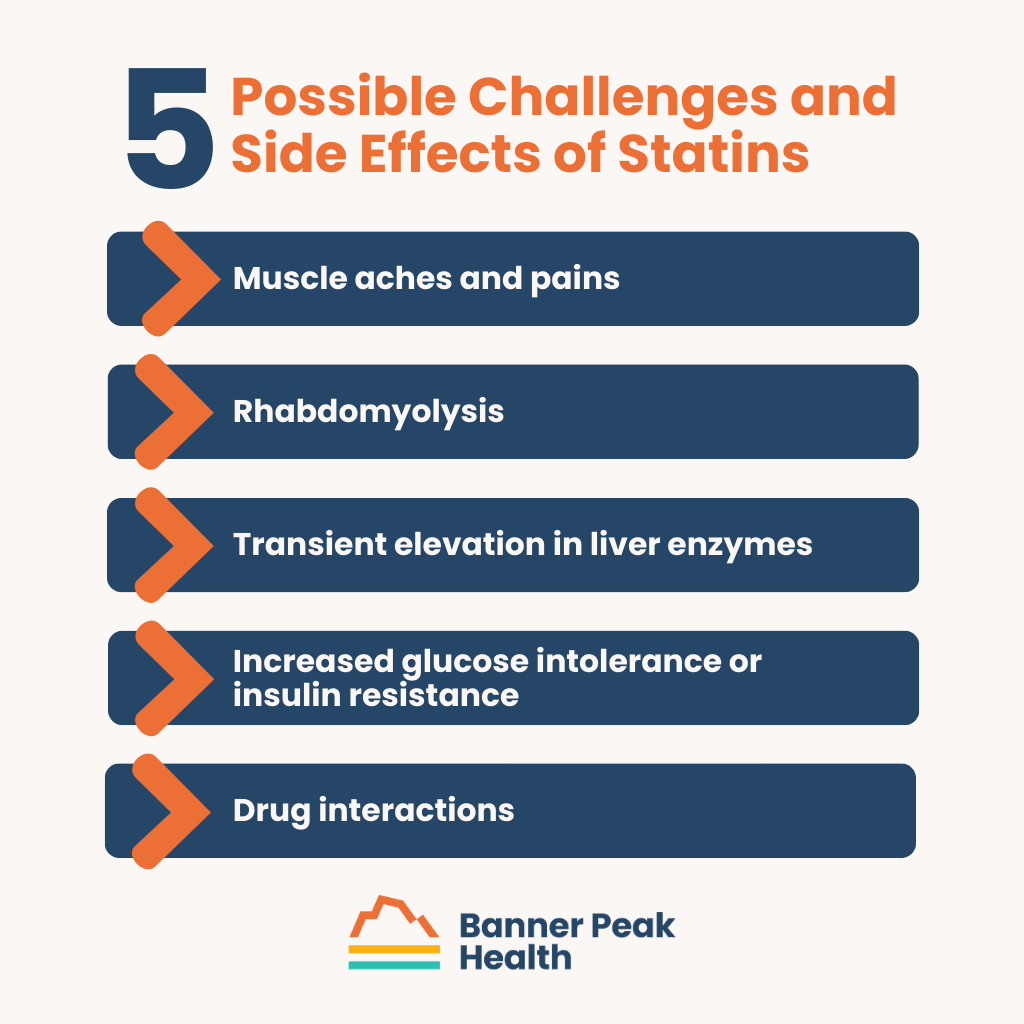
Possible Challenges and Side Effects of Statins
The following are side effects or challenges patients may experience when taking statins:
- Muscle aches and pains: These occur in 5–20% of patients.
- Rhabdomyolysis: This rare muscle breakdown can increase the risk of kidney failure.
- Transient elevation in liver enzymes: Similar to an allergic reaction, this occurs in 10–15% of patients but is completely reversible upon stopping the medication. A doctor monitors the patients’ liver enzymes for signs of elevation during the initial course.
- Increased glucose intolerance or insulin resistance: This can be problematic for diabetics.
- Drug interactions: Patients must avoid certain medications while taking statins, especially atorvastatin and simvastatin.
Not All Symptoms Are Side Effects
Aches and pains are a side effect of statins, but they’re also a normal symptom of aging. Don’t blame the aging process on your medicine.
A patient of mine recently stopped taking a statin due to minor aches and pains, only to experience a major cardiac event a few days later and wind up hospitalized. Don’t make the same mistake.
If You Need a Change, What Can You Do?
If you’re convinced you need to stop taking statins, you have options. First, talk to your doctor.
Alternative Statins
If you react badly to a certain statin, you can probably try a different one. Most side effects are not class effects; you could take another statin and experience none of the same issues.
It’s just a matter of finding the one that’s right for you.
Alternative Medications
Of course, if statins just aren’t right for you, some alternatives to statins don’t have the same side effects. Consider:
- Ezetimibe: Tablets that reduce the amount of cholesterol absorbed from the food you eat
- PCSK9 inhibitors: Two FDA-approved injectables administered every two to four weeks
- Bempedoic acid: Targets the liver, so patients experience fewer muscle aches
Today’s Takeaways
Medications like statins are another reason to have a close, conversational relationship with your doctor. A health advocate who understands your disease risks supports you and keeps you accountable.
If you’re at risk for the poor health outcomes associated with high cholesterol, you should take some kind of medication. Cholesterol is nearly impossible to control with diet alone. Genetics influences about 75% of your cholesterol, while food only influences about 25%.
The good news is that medication is extremely effective, and your doctor is available to help you. The sooner you start, the better.

Waheeda Hiller, MD
For over 20 years in Internal Medicine, Dr. Hiller has dedicated herself to providing unparalleled care to patients. She joined Banner Peak Health in 2023 as a concierge physician to better serve patients with the depth of thought, knowledge, and compassionate care they need to live the healthiest lives possible.



