The Truth About How to “Reset Your Metabolism” (And What Actually Works)
The other night, our new induction stove displayed an error message. The screen flashed a code I didn’t recognize, so I did what any person living in the 21st century would do: I consulted ChatGPT.
The answer was simple: Reset the stove by flipping the circuit breaker off and back on. No forward-facing power switch existed, so I bundled up, trudged outside in the cold, found the breaker box, and flipped the switch.
After a moment, I flipped it back on. The error vanished. Problem solved.
Walking back inside, I thought, “Wouldn’t it be wonderful if we could do the same thing with our bodies? Especially our metabolic health?”
If something feels off (weight creeping up, energy crashing, blood sugar spiking), we want to flip a switch and return to factory settings. This instinct makes perfect sense. We’re 21st-century humans surrounded by technology, and “reset” is our default problem-solving approach.
But our bodies don’t work that way.
If you’ve ever searched “how to reset your metabolism,” you’re not alone. Grasping why that search leads nowhere is the first step toward real metabolic health.
What “Reset Your Metabolism” Really Means
The phrase “how to reset your metabolism” gets searched thousands of times each month. Patients come to me asking for the metabolic equivalent of that circuit breaker: some pill, supplement, or cleanse that will flip everything back to optimal.
Metabolism, like all our health systems, is dynamic. It doesn’t sit at a fixed point waiting to be “reset.” It’s more like a sailboat than a stove. Wind pushes against the sails. Waves rock the hull. Currents pull in unexpected directions.
The boat stays upright not because it’s frozen in place, but because it constantly adjusts, leaning into the wind, correcting course, and rebalancing against every force trying to knock it over.
That’s your metabolism.

Source: Canva
The Science of Staying Upright: Homeostasis
The medical term for this continuous rebalancing is homeostasis. It’s the most important concept for grasping health and aging.
Think about everything that tries to knock you off course: illness, sleep deprivation, injury, dehydration, stress, etc. We need the resiliency to keep correcting and maintaining equilibrium, no matter what life throws our way.
When you think of the word “reset,” you imagine a single moment: returning to one correct position one time. But health isn’t reaching a destination. It’s your ability to get to that destination again and again.
Why You Can’t Reset Your Metabolism With Pills and Supplements
A pill or supplement doesn’t address the core route to health. It just reduces the danger of your body being out of balance.
Take high blood pressure. If your body isn’t maintaining homeostatic balance, your blood pressure rises. That elevation increases your risk of stroke, heart attack, and kidney damage.
We prescribe medication to bring that number down. But the medication doesn’t rebalance your body. It makes being out of balance less dangerous.
The same applies to blood sugar medications, cholesterol drugs, and supplements marketed to reset your metabolism. They may reduce risk, but they don’t restore the ability to self-regulate.
That pill doesn’t get you off the hook for your own lifestyle choices. A physician can prescribe medication, advise you, and point you in the right direction, but the ultimate responsibility for your health rests with you and the choices you make.
You can’t outsource your health to a doctor or supplement. You own it.
The Real Pillars of Metabolic Health
If we abandon the reset mindset in favor of a support mindset, what does that look like in practice?
The foundational pillars are familiar but bear repeating: nutrition, movement, sleep, and stress management. These aren’t sexy, but they influence your body’s ability to maintain equilibrium.
All of life, we are that sailboat, being pushed by winds and rocked by waves. As we age, we don’t right ourselves as quickly. We spend more time leaning, more time off-balance. That’s the disease state. Eventually, if we can’t right ourselves at all, we capsize.
The goal isn’t to never get knocked off course. We need to build the resilience to recover, again and again.
The Danger of Diets That Promise to Reset Your Metabolism
Popular diets and detoxes make bold promises. From a clinical perspective, these extreme approaches often do the opposite of what they claim.
Consider the logic through the lens of homeostasis. If balance is the goal, what happens when you drastically hurl yourself away from the center?
You don’t strengthen your long-term equilibrium. You destabilize it further. Trendy diets don’t address your body’s ability to self-regulate. They just yank the sailboat in the opposite direction temporarily.
When you stumble upon a new health intervention, ask yourself, “Does this support my body’s ability to maintain balance over time? Or does it just promise dramatic short-term change?”
Today’s Takeaways
You can’t reset your metabolism with a pill, cleanse, or crash diet, because metabolic health is about building your body’s capacity to right itself against whatever forces try to knock it down.
Start with one sustainable change. Maybe it’s consistent sleep timing, a daily walk, or reducing processed food at one meal. The starting point matters less than the mindset behind it: you’re investing in resilience, not looking for a quick fix.
At Banner Peak Health, we help patients move beyond the reset mentality toward true metabolic wellness. If you’re ready to stop searching for the magic button and start building sustainable health, we’re here to guide that process.
What Is Hemoglobin A1C? How to Lower It Naturally
Think back to your school days.
At the end of each semester, you received a grade: a single number that reflected months of effort. That grade wasn’t your score on yesterday’s quiz. It integrated your homework, tests, attendance, midterm, and final exam into one indicator of how you performed over time.
Hemoglobin A1C works the same way for your metabolic health. But what is hemoglobin A1C?
This single blood test captures your average blood sugar control over the past 90 days. Unlike a semester grade that only affects your transcript, hemoglobin A1C is far more consequential. It reflects your risk for diabetes, heart disease, cancer, dementia, autoimmune conditions, and even depression.
Metabolic health influences almost every disease we face. That’s why knowing what hemoglobin A1C measures (and what you can do about it) matters so much.
What Is Hemoglobin A1C?
Hemoglobin is a large, iron-containing protein inside your red blood cells. Its job is to carry oxygen from your lungs throughout your body. Each red blood cell lives for approximately 90 days before being broken down and recycled.
Hemoglobin is made of four protein subunits, and two of these can irreversibly bind glucose. As glucose floats through your bloodstream, some of it attaches permanently to hemoglobin molecules. The higher your blood sugar runs, the more glucose binds.
Hemoglobin A1C measures the percentage of your hemoglobin that has glucose attached. A reading of 5% means 5% of your hemoglobin’s binding sites have glucose bound to them; a reading of 7% means 7% are bound. This percentage gives us a weighted average of your blood sugar over the lifespan of your red blood cells: about three months.
Hemoglobin A1C doesn’t measure a concentration in your blood at one moment. It measures the cumulative effect of your blood sugar over 90 days.
What Does Hemoglobin A1C Mean? Reading the Numbers
The American Diabetes Association defines the categories this way:
- Less than 5.7%: Normal
- 5.7% to 6.4%: Prediabetes
- Greater than 6.4%: Diabetes
“Normal” and “optimal” aren’t the same. The risk for insulin resistance and poor metabolic health climbs above 5.4%. If you’re aiming for the best metabolic health, keep that target in mind.
Why Blood Sugar Fluctuates: The Beach Ball Analogy
Many people imagine blood sugar as a simple pipeline: food goes in, sugar enters the bloodstream. But that’s not how it works.
Instead, picture a beach ball being pushed around by many Nerf guns firing from every direction. Each foam pellet nudges the ball a different way. Where the ball ends up depends on those competing forces.
Your blood sugar works the same way. At any instant, it’s being pushed and pulled by:
- What you ate and when you ate it
- Your stress and anxiety levels
- How much sleep you got
- Whether you exercised
- Your body’s hormone fluctuations
- How relaxed or tense you feel
These forces converge to produce your blood sugar reading at any given moment.
Hemoglobin A1C, by contrast, captures the cumulative result of all those pushes and pulls over 90 days. It measures where the beach ball has traveled on average rather than where it is right now.
How to Lower Your A1C Naturally: Two Steps
If hemoglobin A1C is your semester grade, think of a continuous glucose monitor (CGM) as your daily quiz scores. A CGM attaches to your body and measures glucose levels every five minutes, giving you real-time feedback on how your lifestyle choices affect your blood sugar.
But you don’t need a CGM to start improving your metabolic health.
Step One: Lower Hemoglobin A1C Naturally With Lifestyle Fundamentals
Start with the low-hanging fruit. Ironically, that often means reducing the foods in your diet that aren’t fruit:
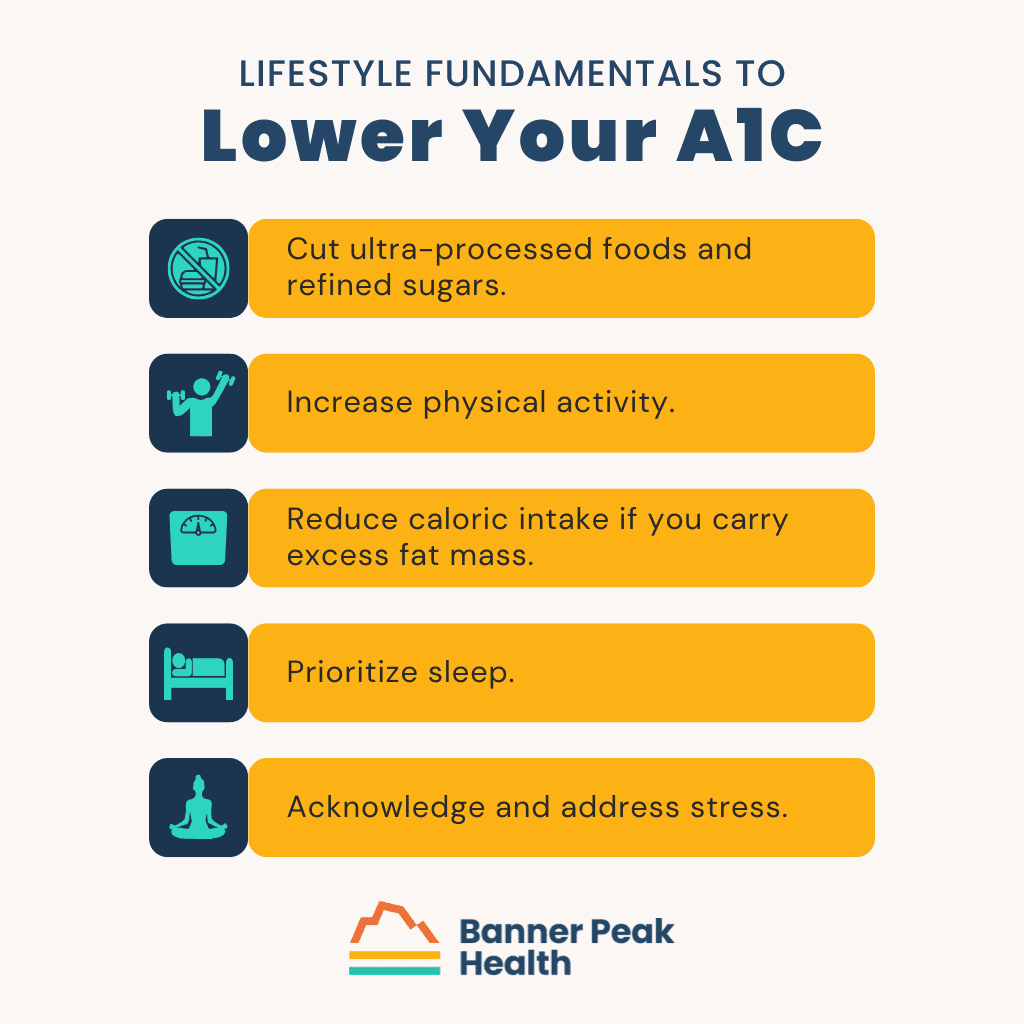
- Cut ultra-processed foods and refined sugars. These spike blood sugar rapidly and offer little nutritional value.
- Increase physical activity. Exercise helps your muscles absorb glucose and improves insulin sensitivity.
- Reduce caloric intake if you carry excess fat mass. Visceral fat directly contributes to insulin resistance.
- Prioritize sleep. Poor sleep disrupts the hormones that regulate blood sugar.
- Acknowledge and address stress. Chronic stress elevates cortisol, which raises blood sugar.
These fundamentals form the foundation of metabolic health. Many people see meaningful improvement in their hemoglobin A1C by applying these principles over several months.
Step Two: Fine-Tune With Real-Time Feedback
If you want to go deeper, a continuous glucose monitor offers a granular view of your individual responses. You’ll learn what foods spike your blood sugar, how timing and food combinations matter, and how exercise and sleep affect your readings.
This is personalized medicine at its most practical. Rather than following generic advice, you learn what works for your body. At Banner Peak Health, we help patients with this kind of data-driven optimization.
Setting Realistic Expectations
Metabolic health unfolds over months and years, not days. You can only meaningfully recheck your hemoglobin A1C every three months, since that’s how long it takes your red blood cells to turn over and reflect your new patterns.
You won’t find a silver bullet for this. If you want to lower your A1C naturally, it requires an integrated approach: better nutrition, more movement, adequate sleep, and managed stress.
Today’s Takeaways
So what is hemoglobin A1C, really? It’s not a verdict. It’s information: a snapshot of where your metabolic health has been over the past three months.
If that number is higher than you’d like, start with the fundamentals in Step One. If you want more precision, consider working with a CGM to understand your body’s unique responses.
At Banner Peak Health, hemoglobin A1C is one of many tools we use to assess and optimize your health. We’re here to help you interpret your numbers and build a personalized plan to improve them.
Best Timing for a PSA Test: A Physician’s Guide for Middle-Aged Men
Back in 1979, a book called Don’t Buy a Car Made on Monday came out, using a humorous title to introduce the idea that what auto workers did over the weekend impacted their work quality on Monday. There was never hard data to support the assertion, but the idea became accepted folklore.
Let’s explore how the same principle may apply to PSA testing.
What the Prostate Does
The prostate secretes prostatic fluid, an integral part of the male reproductive system. This fluid provides the environment for semen to do its job: It serves as an energy source for spermatozoa, helps balance pH during intercourse, and creates the correct viscosity for reproduction.
Prostatic fluid contains a protein called prostate-specific antigen, or PSA. To know what to avoid before a PSA test, you first need to know how PSA gets into your bloodstream.
The Jelly Donut: Prostate Anatomy Explained
Think of the prostate as a prostatic fluid factory, made up of multiple coils of tiny tubes. The inside of each tube produces prostatic fluid, including PSA. These tubes are surrounded by the blood supply, with capillaries running alongside them.
The diagram below shows a cross-section of one of these tubes.

Think of each tiny tube as a miniature jelly donut. The interior jelly is the prostatic fluid (containing PSA), and the donut itself is the layer of cells that produce and contain it.
Anything that disturbs that little miniature donut and allows the jelly to leak out into the bloodstream will raise your PSA.
Why PSA Is Used for Cancer Screening
We use PSA to screen for prostate cancer because abnormal growth within the prostate disturbs the anatomy of those jelly donuts lined up inside it.
Cancer causes the donuts to leak their interior into the bloodstream, elevating PSA.
That’s why elevated PSA can signal a problem worth investigating.
The Problem: PSA Is Not Specific
Any single PSA that comes back abnormally elevated is a false positive 70–80% of the time.
Why so many false positives? Because there are many ways to disturb that jelly donut other than cancer.
What Can Disturb the Prostate (and Raise Your PSA)
Benign Prostatic Hypertrophy (BPH)
As men age, the prostate enlarges. This age-related growth is called benign prostatic hypertrophy. As everything expands and compresses, the jelly donuts become more prone to leaking.
This growth isn’t dangerous, just the normal wear and tear of aging, but your PSA can rise as a result.
Inflammation
If there’s inflammation in the prostate, whether from a bacterial infection or other causes, it creates disturbance in the jelly donut structure. Inflammation makes the junctions between cells more porous, and the jelly (PSA) leaks out.
This is called prostatitis, and it’ll elevate your PSA.
Trauma
Direct trauma to the prostate, whether from medical procedures in that area or from injury, can disturb the anatomy and cause PSA to enter the bloodstream.
Pressure From Cycling
Given the anatomy of sitting on a bicycle, particularly a road bicycle, force is applied to the perineal area. Over a number of hours, this external pressure from the bike seat transmits to the prostate, disturbing those jelly donuts.
Literature documents that a bike ride of several hours can cause a measurable elevation in PSA. So, how long do you need to avoid exercise before a PSA test? At a minimum, 48 hours after any extended cycling.
Sexual Activity
Ejaculation creates leakiness within the prostate’s epithelial cells and basement membrane. The process of secreting and ejaculating prostatic fluid disturbs the jelly donut structure, causing PSA to rise and enter the bloodstream.
How long before a PSA test should you not ejaculate? The same rule applies: at least 48 hours.
What to Avoid Before a PSA Test
For the most accurate PSA result, you need to be at least 48 hours removed from:
- Extended bike riding (especially road cycling)
- Sexual activity
If you have an ongoing prostatitis or infection in the genitourinary tract, you don’t get your PSA tested. Wait until the infection has resolved.
General Principles About PSA Testing
Because false positives outnumber true positives by a three-to-one or four-to-one ratio, the first thing to do when you see an abnormal PSA is repeat it.
Before you freak out, pursue further workup, or move to more sophisticated blood testing, anatomical imaging, or urine testing, push the pause button. Think through all the causes for false positives, make sure none of them apply, and then repeat the test.
I learned this adage in medical school: “A single abnormal test does not a disease make.”
When confronted with an elevated PSA, both the doctor and the patient become alarmed and want to move to the next steps immediately. Resist that urge. A careful, repeated test under the right conditions is the appropriate first response.
Today’s Takeaways
Who gets tested for PSA? Middle-aged men. If you’re too young, you don’t get tested. Too old, you don’t get tested.
And what do a lot of middle-aged guys do on the weekends? They go on long bike rides and have sex.
That artificially elevates their PSA on Monday.
Think about what to avoid before your PSA test: no cycling and no sexual activity for at least 48 hours beforehand. And if you do get an elevated result, don’t panic. Repeat the test under optimal conditions before pursuing further workup.
At Banner Peak Health, we take the time to think through the nuances of testing like this. A thoughtful approach to PSA screening can save you from unnecessary anxiety and invasive follow-up procedures.
How Long Should You Cold Plunge? A Physician’s Advice
Everyone wants to know the recipe: How long should you cold plunge? How cold should the water be? How many times per week?
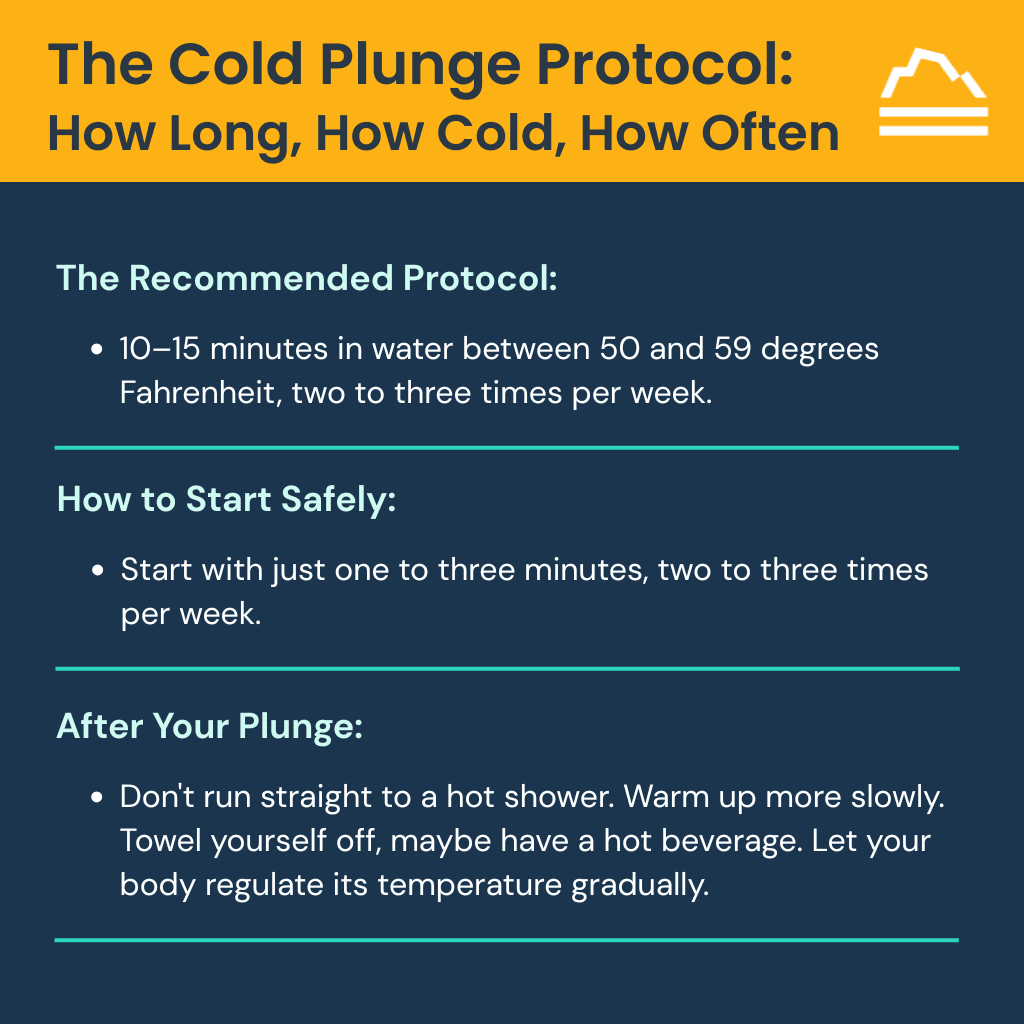
The recommended protocol is 10–15 minutes in water between 50 and 59 degrees Fahrenheit, two to three times per week.
But understanding how cold water immersion works, and how to do it safely, requires a deeper look at what happens in your body during those minutes in icy water.
How Cold Water Immersion Works
Cold water immersion triggers two distinct mechanisms in your autonomic nervous system.
First, we have what’s called the diving reflex. Receptors in the skin of your face and upper body trigger your parasympathetic nervous system to respond when you’re fully immersed in cold water. This ancient reflex helped our ancestors survive underwater.
Second, the initial shock of cold water creates a surge of sympathetic discharge. Your body responds with peripheral vasoconstriction, increased heart rate, and elevated blood pressure. Then, your body tries to compensate by triggering increased parasympathetic tone.
This back-and-forth between sympathetic activation and parasympathetic compensation is where cold plunging becomes what I call “parasympathetic rehab” or “homeostasis training.”
Rethinking the Autonomic Nervous System
For years, I’ve explained the autonomic nervous system using a teeter-totter metaphor: the sympathetic nervous system (fight or flight) on one side, the parasympathetic nervous system (rest and digest) on the other, and balance achieved in the middle.
But that metaphor has a flaw. It suggests equal symmetry on each side, as if both systems play equivalent roles in our health.
They don’t.
A better metaphor is a sailboat in stormy seas.
The sympathetic nervous system is the sail and mast. It propels you forward, but it’s also a toppling force. In a strong wind, the sail wants to knock the boat over. Sympathetic overload is associated with disease.
The parasympathetic nervous system is the weighted keel below the waterline. It anchors the boat and keeps it upright. Parasympathetic strength is associated with resilience to disease and the ability to maintain homeostasis.
This ties into aging and longevity. Aging is about homeostasis: our ability to rebalance after the inevitable buffeting of life.
As we age, we don’t right our sailboat as well. The parasympathetic nervous system degrades. Heart rate variability (HRV), our best real-time measure of the balance between sympathetic and parasympathetic tone, declines with age.
Keeping the sailboat upright allows us to age more successfully.
Cold water immersion strengthens your weighted keel. It trains your parasympathetic nervous system to respond more effectively to stress.
The Well-Supported Benefits
Cold water immersion has advantages across several areas, and the literature supports these benefits well.
Sports Recovery
Studies show a reduction in delayed onset muscle soreness (DOMS). Cold water immersion has demonstrated benefits in muscle performance during jumping and sprinting, as well as reduced markers of muscle damage in the blood.
Mental Health and Sleep
Cold water can improve feelings of stress and negative emotions. It can help with relaxation and sleep quality, which makes sense given our discussion about sympathetic and parasympathetic balance.
Metabolic Health
Cold water immersion can increase the energy your body uses, which may help with metabolism.
A small percentage of our total fat is brown fat. Unlike white fat, brown fat burns calories to generate heat. Cold water immersion activates these fat cells, which can increase your basal metabolic rate. Evidence suggests that overall metabolic health improves with cold water immersion: lower blood sugar, better insulin sensitivity.
Cold Plunging: The Dangers You Need to Know
Rapid sympathetic discharge followed by compensatory parasympathetic response can be dangerous. This is why understanding how long and how to cold plunge is necessary for safety.
Cold Shock
Cold shock occurs when your body is immersed in water below 59 degrees Fahrenheit. Anyone who has jumped into a cold lake has probably experienced this. It’s an involuntary set of reactions that can last from a few seconds to about a minute, peaking around 30 seconds.
During that minute, you gasp involuntarily. Your breathing rate increases — hyperventilation. Your heart rate shoots up rapidly. Blood pressure surges. Peripheral vasoconstriction occurs.
If you’re immersed underwater, it’s a real drowning risk. You involuntarily open your mouth. You could aspirate, or even drown.
If you have any risk factors for cardiac arrhythmia, this sudden buffeting by the sympathetic surge and parasympathetic compensation creates risk for dangerous heart rhythms.
As a backpacker, I’m acutely aware that at elevation (6,000–10,000 feet), the hypoxia in the air accelerates all this and compounds the potential risk of cold shock.
One of my daughter’s classmates died while swimming in a mountain lake. He was college-aged and very healthy. It was probably a cold shock reaction.
When I go backpacking with my kids and they want to swim in a mountain lake, I tell them to stay parallel to the shore and not try to swim across the lake. People underestimate the risks of cold water at elevation.
Who Shouldn’t Cold Plunge
So, how long should you cold plunge? For people with the following conditions, zero minutes and zero seconds:
- Heart disease or any cardiac problems
- Uncontrolled blood pressure
- Raynaud’s disease
- Asthma
- Neuropathy
- Pregnancy
- Recent surgery
Nobody should practice cold-water immersion alone in open water, regardless of health. Have others nearby.
How to Start Safely
When beginning cold water immersion, don’t start by instantly putting your head under the water. For the first minute, keep your head above the water.
Start with just one to three minutes, two to three times per week.
You’ll adapt to cold water immersion over time. Like anything, build up gradually. Over weeks and months, you can work toward the 10–15 minutes recommended in the literature. If at any point you experience chest discomfort, lightheadedness, numbness, or dizziness, abort the mission.
Once you finish your cold water immersion, don’t run straight to a hot shower. That’ll give your system too much stimulation in the other direction.
Warm up more slowly. Towel yourself off, maybe have a hot beverage. Let your body regulate its temperature gradually.
Cold Plunging: A Potent Tool, Not a Silver Bullet
Cold water immersion can be a wonderful tool for enhancing parasympathetic tone and recovery after intense workouts, but don’t think of it as a standalone modality or silver bullet.
It’s an arrow in the quiver: one tool among many in a more robust parasympathetic rehab program that includes meditation, careful attention to breathing, Zone 2 cardio, and other lifestyle interventions.
At Banner Peak Health, we look for every possible mechanism to strengthen the parasympathetic nervous system and enhance our patients’ resilience. Cold water immersion, practiced safely and as part of a comprehensive approach, can be a valuable addition to that program.

How a Simple Nasal Spray May Help Prevent COVID and Colds
Getting COVID is never fun.
Last September, I attended a national physician conference and came home with an unwelcome souvenir: COVID. I developed a relatively mild case, but nonetheless, I wasn’t myself for at least a few weeks.
Fast-forward to the same conference in 2025. This time, I went armed with azelastine nasal spray, an over-the-counter antihistamine commonly used for allergies. I applied one spray in each nostril twice a day.
The meeting became what most would call a superspreader event: More than 20 of about 100 attendees caught COVID. But I dodged the bullet.
The Science: Blocking the Virus at the Gate
Azelastine isn’t new. It’s been used safely for decades to treat allergic rhinitis. What’s new is our understanding of how it might protect against respiratory viruses.
COVID and many other upper respiratory infections begin in the nose. The COVID virus binds to ACE-2 receptors on nasal cells — the same area azelastine coats when sprayed.
In laboratory and animal models, azelastine disrupts viral entry, reduces local inflammation, and even interferes with enzymes needed for viral replication. It seems to make the nasal environment less hospitable to infection.
The CONTAIN Trial: From Theory to Proof
In 2025, researchers at Saarland University Hospital published the CONTAIN trial in JAMA Internal Medicine.
Four hundred fifty healthy adults used either azelastine 0.1% or a placebo three times daily for 56 days. Participants self-tested twice weekly for COVID and were screened for other viral infections when symptomatic.
Results:
- COVID infection occurred in 2.2% of the azelastine group vs. 6.7% of the placebo group — a 69% reduction in risk.
- Colds caused by rhinovirus were also reduced (1.8% vs. 6.3%).
- Side effects were mild — mostly a brief bitter taste or a minor nose irritation.
Azelastine’s effect was localized, safe, and surprisingly broad, suggesting protection not only from COVID but also from everyday URIs.
Why This Matters
Vaccines and antivirals remain our strongest defenses against severe disease, but their ability to prevent infection wanes over time and with new variants. Azelastine adds another layer: a topical, low-cost, non-systemic option that can be started immediately and used intermittently — say, during travel, conferences, or cold-and-flu season.
Because azelastine is already FDA-approved for allergies, it’s accessible and familiar. Its mechanism is preventive, not curative. It’s a daily shield, not a rescue medication.
Sometimes, progress doesn’t require a new drug — just a new way of using an old one.
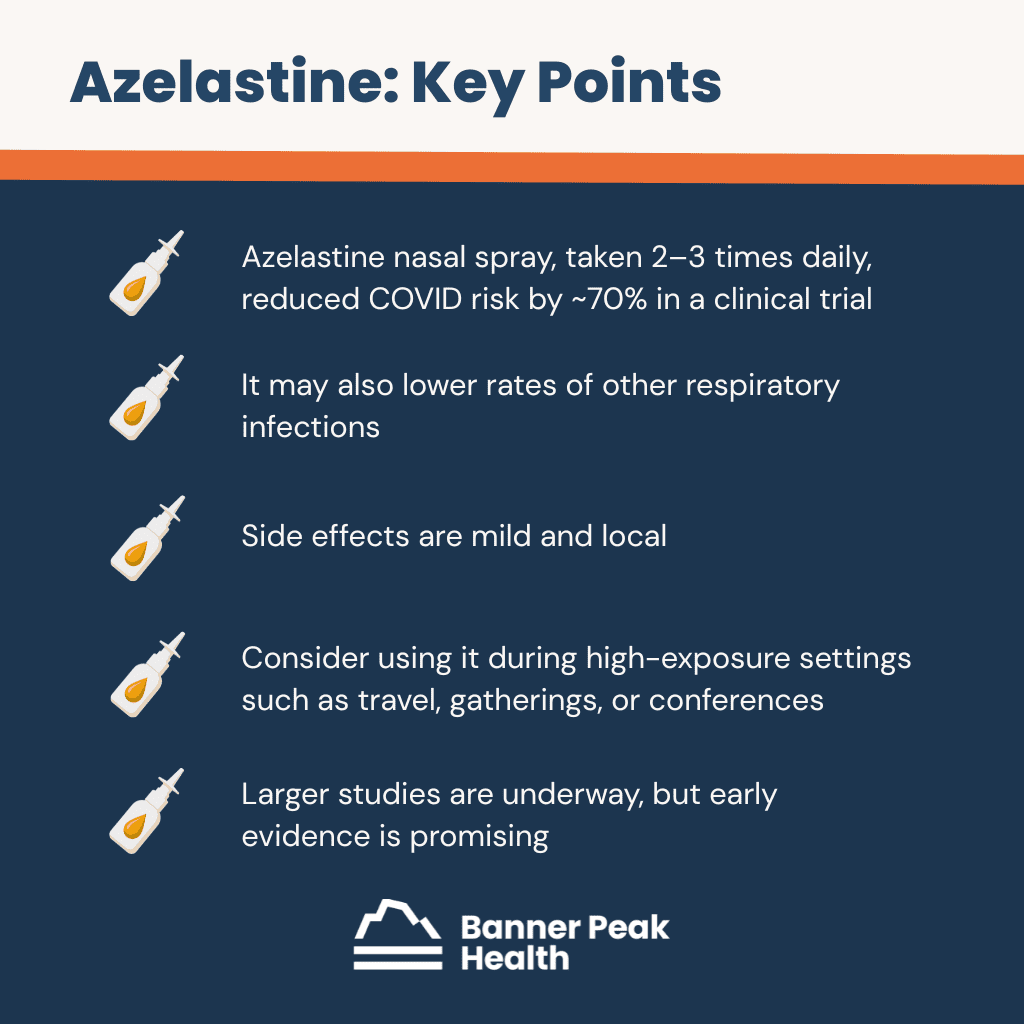
Today’s Takeaways
- Azelastine nasal spray, taken two to three times daily, reduced COVID risk by ~70% in a clinical trial.
- It may also lower rates of other respiratory infections.
- Side effects are mild and local.
- Consider using it during high-exposure settings such as travel, gatherings, or conferences.
- Larger studies are underway, but early evidence is promising.
- Available without a prescription.
At Banner Peak Health, we continue to explore evidence-based, practical tools for optimizing resilience. Sometimes, the simplest interventions, like a nasal spray, can make the biggest difference.
More Than Medicine: Inside Banner Peak Health’s Community-Driven “Outperform” Concept
Most people think being healthy means not being sick. This limited view constrains how we approach our well-being and what we believe is possible.
At Banner Peak Health, we’ve developed a philosophy that shatters this traditional mindset. We call it “Outperform.”
Redefining Health Beyond Disease
We define medicine 2.0 as medical care that treats existing disease. When you’re sick, you see a doctor, get treatment, and return to “normal.” Health in this system means the absence of disease, nothing more.
Medicine 3.0 takes the next step: preventing disease before it occurs. We screen, test, and identify risk factors. This approach, which forms the foundation of concierge medicine, represents real progress.
But even prevention keeps the focus on disease.
What we’re pursuing at Banner Peak Health goes even further than medicine 3.0. We provide optimization: maximizing your potential, your function, your energy, and yes, your emotional well-being. It’s a different way to think about health.
Follow the Money
To understand this shift, we need to examine healthcare funding.
Traditional fee-for-service medicine relies on procedure codes based on either treating specific diseases or preventing specific diseases. There’s no funding mechanism for optimization.
Insurance companies don’t reimburse for helping someone feel extraordinary. Medicare doesn’t have billing codes for maximizing human potential. The financial structure of traditional healthcare ignores optimization.
Our practice operates on a different model. We’re funded by you, our patients. Not government programs. Not insurance companies.
This direct relationship allows us to build healthcare strategies that meet your needs, including the pursuit of optimal health. Our Outperform program’s financial and philosophical underpinnings rest on this foundation.
From Passive Patient to Active Participant
Outperform changes the question of healthcare. Instead of asking, “What can the medical system do for me?” our patients ask, “What can I do for myself with the medical system’s support?”
Traditional healthcare creates passive relationships. You wait until something goes wrong, then seek treatment. Even preventive care often feels like something done to you rather than with you.
Outperform demands active participation. You own your journey. We teach you how to fish while providing the best equipment and guidance available.
This change happens through what we call MDEC: the Metric-Driven Empowerment Cycle. We leverage current technology to provide real-time, actionable, personalized data that puts you in the driver’s seat.
Take heart rate variability monitoring through the Oura Ring, our preferred wearable device. This technology tracks the balance between your sympathetic and parasympathetic nervous systems, measuring how well your body manages stress and recovery.
You generate the data. We guide you in understanding it. You own where that data takes you on your journey.
Continuous glucose monitoring is another example. Every five minutes, you know your blood sugar level. This integrates everything: stress, activity, sleep, nutrition, and meal timing. The data is personalized, actionable in real time, and yours to leverage.
Traditional medicine focuses on diagnostics and screenings, looking for problems. We focus on monitoring and metrics, tracking progress toward optimal function. One searches for what’s wrong. The other measures what’s possible.
Building Health Through Community
Traditional medicine focuses on individual behavior change. In reality, we all exist in a community. Why not approach healthcare through the lens of how we interact with others?
Society faces an epidemic of loneliness. Copious literature documents the negative biological outcomes of isolation. Social connection improves both emotional well-being and physical health. A human being connected in community is a healthier human being.
Many societal trends have decreased social cohesion. Life has become less social, a phenomenon the pandemic accelerated. Through Outperform, we’re connecting people wherever possible, using education and athletics as tools for bringing our community together.
We’ve launched a pilot program: weekly exercise classes open to the entire Banner Peak Health community and staff. These sessions create connection, shared goals, and mutual support.
The science of behavior change proves that people make better choices in a community. Whether through family relationships, friendships, or organized groups, connection drives healthier decisions. Data on marital status and health outcomes, social support and recovery rates, community involvement and longevity all point to the same conclusion.
Overcoming Traditional Healthcare Limitations
In traditional healthcare settings, implementing data-driven, personalized optimization is challenging.
The technology we use, including Oura Rings, continuous glucose monitors, and advanced metabolic testing, either lacks insurance coverage or requires too much time to implement under fee-for-service constraints.
Consider continuous glucose monitors. They’re available over the counter, but extracting meaningful insights from the data, understanding patterns, and making personalized recommendations requires labor-intensive processes that don’t fit into seven-minute appointment slots or insurance-reimbursable categories.
Traditional fee-for-service practices can’t provide this level of attention. We can.
Our position allows us to identify and adopt emerging technologies early. We evaluate innovations that improve the optimization process, from advanced sleep monitoring to new recovery tools. When something proves valuable, we can implement it without waiting for insurance approval or billing code creation.
Beginning Your Outperform Journey
For someone inspired to move from “not sick” toward optimal health, the most important step is openness.
Whatever approaches you’ve tried before and whatever you’re comfortable with won’t be as effective for moving forward as the new directions we can explore together. You don’t know what you don’t know.
The process we’re describing differs from traditional healthcare. If you’re open to rethinking the entire approach, we can take you somewhere extraordinary.
We’re reimagining what health means and what’s possible when you combine new technology, personalized data, community support, and medical expertise freed from insurance constraints.
Today’s Takeaways
Health means more than the absence of disease. It also means more than prevention.
True health optimization requires a change in how we approach well-being: from passive recipient to active participant, from isolated individual to connected community member, from accepting “normal” to pursuing extraordinary.
At Banner Peak Health, our Outperform philosophy makes this change possible. Through metric-driven empowerment, community connection, and freedom from traditional funding constraints, we’re creating healthcare that helps you maximize your potential.
The question isn’t whether you’re sick. The question is: How extraordinary could you feel?
Fall Vaccine Update 2025
COVID Vaccine
As the bumper sticker states, “If you’re not confused, you’re not paying attention.”
We’re releasing this year’s fall vaccine update amid a political storm that has engulfed health policy. Traditional sources of federal vaccine policy, such as the Centers for Disease Control and Prevention (CDC), the Food and Drug Administration (FDA), and the Advisory Committee on Immunization Practices (ACIP), have been dramatically altered from their prior policy positions.
For example, the ACIP has traditionally met in June and provided guidance for fall vaccine recommendations. However, the entire 17-member ACIP committee was dismissed on June 8, 2025. This panel contained experts in the fields of health policy, immunology, and vaccine research.
Robert F. Kennedy Jr. (RFK), Secretary of Health and Human Services, replaced the panel with eight appointees who have a history of vaccine skepticism and limited experience in vaccine science. The new panel met later in June but offered no guidance on the current COVID vaccine policy, a marked departure from prior June ACIP meetings.
The most current federal COVID vaccine policy stems from a directive issued directly by RFK Jr. in May 20251, bypassing the ACIP and the FDA’s August 2025 vaccine approval indications. In the past, COVID vaccination was recommended for everyone over six months old, including children and pregnant women. The current authorizations are drastically curtailed, with recommendations for adults 65 years and older and people of any age with at least one underlying health condition that increases the risk for severe COVID, such as obesity, cancer, diabetes, or an immunocompromised condition.
At Banner Peak Health, we continue to recommend COVID vaccination for anyone over the age of 50 as well as anyone over six months with a risk factor for a severe outcome from COVID, including pregnancy.
The discrepancy between our recommendations and the FDA’s can be reconciled by the extensive list of health conditions that qualify as risk factors. This list includes individuals with elevated BMI, heart disease, and chronic lung disease, as well as physically inactive individuals. We can find a route to meet the FDA indications for almost everyone.
Also, if you have close contact with someone at risk for severe COVID, you need the vaccine even if you aren’t at high risk.
This year, we’re partnering with VaxCare, a vaccine delivery company, which will allow us to expand the vaccines we provide in the clinic to include COVID vaccines. This year, our office has a supply of Pfizer’s COMIRNATY® 2025–2026 Formula.
The 2025 formulation has been updated to target the JN.1 variant, which dominated last winter’s wave. In addition, the FDA has recommended a shift toward the LP.8.1 sublineage, an offshoot of JN.1 that is now becoming more common.
This update is intended to restore protection as the virus evolves. While vaccines may not prevent every mild infection, they remain highly effective at reducing the risk of severe disease, hospitalization, and death.
Key COVID Vaccine Points:
- If you’re over 50 years old, please get a COVID vaccine.
- If you’re under 50 years old with risk factors, please get the vaccine.
- If you’re pregnant, please get the vaccine.
- If you’re not high risk but have close contact with someone who is high risk, please get the vaccine.
- We can provide a COVID vaccine in our clinic.
RSV Vaccine
RSV, short for respiratory syncytial virus, isn’t just a disease kids get. It can also cause serious illness in adults, especially as we get older or if we’re living with health issues like heart disease, COPD, or diabetes.
For folks over 60, RSV is now recognized as a leading reason for hospital stays, sometimes even landing people in the ICU, much like the flu does. The most significant risks are for people over 75, those in nursing or assisted-living homes, or anyone already dealing with chronic health problems. While healthy adults usually get a mild cold-like illness, those at higher risk can face pneumonia, worsening of their ongoing conditions, a long, slow recovery, and even death.
The respiratory syncytial virus (RSV) vaccine is entering its third season of use. Initial estimates of a markedly elevated risk of neurological autoimmune illnesses — such as Guillain-Barré syndrome and acute disseminated encephalomyelitis — have not been borne out with greater usage.
We agree with the current ACIP recommendations that all adults aged 75 and older receive the one-time vaccine. Adults ages 50–74 with one or more risk factors for severe outcomes should be vaccinated. Those who are pregnant should receive the vaccine between 32 and 36 weeks of gestation. We have a supply of Pfizer’s Abrysvo® (RSVpreF) vaccine.
Key RSV Vaccine Points:
- One-and-done vaccine.
- If you are over 75, please get the vaccine.
- If you are 50–74 with one or more risk factors, please get the vaccine.
- Pregnant women should receive the vaccine between weeks 32 and 36 of pregnancy.
- Do not combine the RSV vaccine with other vaccines.
Influenza Vaccine
No controversy here2. We have solid evidence that influenza vaccination reduces the risk of illness, hospitalization, and death in children and adults. Therefore, we recommend it for everyone.
We recommend you wait until October to receive your influenza vaccination. A slight delay ensures the vaccine’s three to four months of peak protection come a bit later in the flu season, which peaks late in California and can last through April/May.
However, if you plan to travel in October, receiving the vaccine in September is okay. This way, your body has adequate time to respond to the vaccine before traveling.
This season, we have a supply of Sanofi’s Flublok® vaccine, which we prefer over other vaccines due to its documented better efficacy: It contains more hemagglutinins than the standard quadrivalent flu vaccines.
For those over 65, we have Sanofi’s Fluzone High-Dose®, which supplies a slightly higher stimulus to the immune system for those old enough to recall black and white television sets and “stick shift” cars.
Emerging data demonstrates that receiving an influenza and COVID vaccine simultaneously doesn’t cause appreciably more side effects and can reduce the total amount of time you spend feeling “off.” That means you can get all your vaccines in one sitting and “just get it over with.”
Key Influenza Vaccine Points:
- Everyone needs an annual booster.
- Late October to early November is the best timing, unless you’re traveling in the fall.
- You can combine the flu and COVID vaccines on the same day.
The Bottom Line
Now is the time to plan your fall vaccine schedule. Please call the office to schedule your vaccinations.
If you have mild cold or flu symptoms, you can still receive a vaccine. However, if you have a fever or more severe symptoms, please delay receiving a vaccine.
Sincerely,
Barry Rotman, MD
Waheeda Hiller, MD
Lindsay Klein, MD
Ari Katz, MD
1. Most of the media focused on the change in populations recommended to receive the COVID vaccine, which overshadowed the potential impact of requiring randomized placebo-controlled trial data to approve future iterations of COVID vaccines. The original COVID vaccine trials were conducted in 2020 and 2021 and followed a traditional randomized placebo-controlled format with large numbers of people receiving the new vaccines. Subsequent years’ vaccines have been approved based on the same FDA biologics framework used for seasonal influenza updates. Manufacturers submitted immunogenicity and safety data (not new placebo-controlled efficacy trials). Running large placebo trials each season would be impractical and unethical once safe, effective vaccines were already available. In fact, there would most likely not be time to conduct such trials each year, given the time imperative to generate a new vaccine each year to target that year’s anticipated new strain. The directive would severely curtail pharmaceutical companies’ ability to annually upgrade COVID vaccines to adapt to emerging strains.
2. Okay, a bit of controversy. At its June 2025 meeting, the newly formed ACIP recommended removing thimerosal (a mercury-based preservative used in multidose vials) from all US influenza vaccines. This recommendation was based on their belief that the mercury in the vaccine preservative created a risk of neurological disease in children. Extensive medical research on the topic has disproven this idea. RFK Jr. made this official policy on July 23, 2025, raising concerns that eliminating the entire supply of multidose influenza vaccines would lead to a flu vaccine shortage for the 2025–2026 season. Fortunately, multidose vials represent only 5% of this season’s supply and will NOT compromise the vaccine’s availability in single-dose vials.
Unlocking Your Vagus Nerve: How Truvaga Can Calm Inflammation, Stress, and Pain
We’re excited about a device that’s changing how we approach stress management and nervous system health: Truvaga, a vagus nerve stimulator that brings medical-grade neuromodulation into your daily routine.
Before discussing this device, we need to understand the nerve it stimulates.
The Vagus Nerve: Your Body’s Master Controller
The vagus nerve controls your immune system activation, heart rate, digestion, blood pressure, and more. This single nerve originates in the brain stem and branches throughout your body, reaching the voice box, lungs, heart, kidneys, spleen, and digestive tract.

Think of it like the wiring in a 777 jet. Complex electrical systems run throughout the plane that send information to and from a central computer. The vagus nerve works the same way: It carries sensory signals from your organs to your brain and control signals from your brain back to control organ function.
As the vagus nerve passes through your neck, it wraps around the carotid artery and lies just millimeters below the skin’s surface. This proximity means we can easily stimulate this master nerve with very low electrical current, right where you’d check for a pulse.
Parasympathetic Rehab: A New Approach to Balance
For years at Banner Peak Health, we’ve explored the human body’s sympathetic versus parasympathetic balance. Modern life jacks up our sympathetic nervous system, the “fight or flight” response. We don’t need to work at increasing sympathetic tone; stress does that for us.
What we need is parasympathetic rehab: strengthening our “rest and digest” system.
We’ve explored many approaches:
- Meditation
- Diaphragmatic breathing
- Cold exposure
- Certain types of music
- Touch and social connection
- Aerobic exercise
- Quality sleep
Truvaga adds to this toolkit. It augments these other parasympathetic-enhancing practices rather than replacing them.
How Truvaga Works
Truvaga is a fist-sized, battery-powered device that delivers low-level electrical current to the vagus nerve through your neck skin. You adjust the intensity until it feels tingly but not painful.
The protocol is simple: two minutes on each side of the neck, twice daily.
The stimulation travels from your neck to the brain stem, where it communicates with different brain regions. This reprograms how your brain directs functions throughout your body, recalibrating your stress response system.
Benefits of Vagus Nerve Stimulation
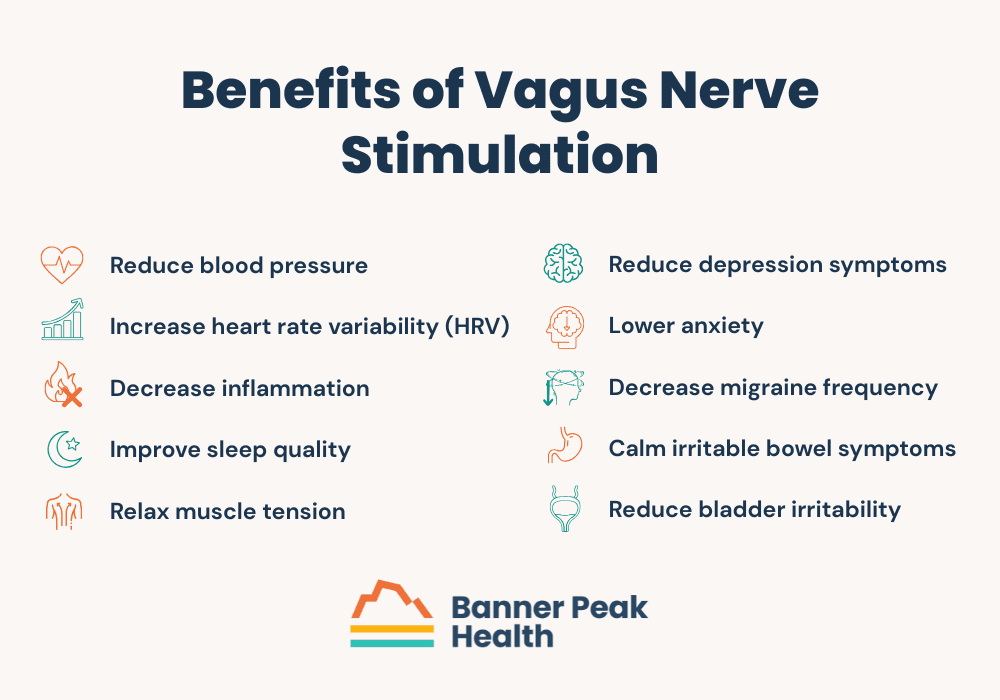
Regular use of a vagus nerve stimulator device can:
- Reduce blood pressure
- Increase heart rate variability (HRV)
- Decrease inflammation
- Improve sleep quality
- Relax muscle tension
- Reduce depression symptoms
- Lower anxiety
- Decrease migraine frequency
- Calm irritable bowel symptoms
- Reduce bladder irritability
Just last month, researchers announced a surgically implantable vagus nerve stimulator for rheumatoid arthritis, demonstrating how this nerve affects immune function.
Truvaga Review: The Science Behind the Device
I’ve spent over a year exploring various devices that claim to enhance parasympathetic tone. Most lacked scientific validation.
Here’s why I’m confident recommending Truvaga: It provides the same electrical stimulus as gammaCore, an FDA-approved prescription device that costs $8,000 plus annual maintenance fees. Years of research on gammaCore show benefits for migraines, cluster headaches, and stress-related conditions.
We conducted our own investigation (including oscilloscope tracings with my daughter, who studies biomedical engineering) and confirmed Truvaga delivers the exact same stimulation protocol as gammaCore. This means Truvaga stands on eight years of validated medical research, not marketing hype.
My Personal Truvaga Experience
As part of my “me-search” approach to testing new technologies, I’ve used Truvaga for eight months. My routine is simple: spray salt water solution for conductivity, apply the device, adjust the intensity, and stimulate for two minutes per side, twice daily.
I didn’t feel immediate effects. But over weeks and months, I noticed improvements.
My migraine frequency decreased. My sleep quality improved. My mood stabilized during stressful periods.
Was this a placebo effect? No. It was my vagus nerve responding as the research predicts.
After 63 years of sympathetic overdrive, rebalancing takes time. You’re asking a small device to undo decades of stress accumulation. With patience and consistency, combined with other parasympathetic practices, you can see strong results.
Who Benefits From Truvaga?
Given our stressed society and the prevalence of conditions linked to autonomic imbalance, most people could benefit from a personalized parasympathetic rehab program that incorporates Truvaga.
The device is safe. Contraindications include:
- Implanted electrical devices (pacemakers, defibrillators)
- Slow heart rate
- Active neck infections or injuries
Always consult your physician if you have cardiac conditions or other health concerns.
Practical Integration
Using Truvaga requires minimal time commitment but consistent practice. Here’s the protocol:
- Clean the neck area.
- Apply conductive spray.
- Position the device against your neck (finding the carotid pulse helps locate the correct spot).
- Adjust intensity to a comfortable tingle.
- Stimulate for two minutes.
- Repeat on the opposite side.
- Perform twice daily.
Combine Truvaga with other parasympathetic practices for optimal results. Think of it as one instrument in an orchestra: effective alone, but best as part of a complete wellness approach.
Today’s Takeaways
- Truvaga delivers the same proven stimulation as prescription gammaCore devices.
- Clinical studies support benefits for migraines, anxiety, and autonomic balance.
- The device is simple, safe, and suitable for home use.
- Best results come from combining Truvaga with other lifestyle approaches.
- Rebalancing your nervous system takes time; expect gradual improvements over weeks to months.
At Banner Peak Health, we’re committed to evidence-based innovation. Truvaga exists at the leading edge of bioelectronic medicine: non-invasive, drug-free interventions that help your body regulate itself.
We’re developing personalized parasympathetic rehab programs and have a Truvaga lending library, allowing patients to try the device before purchasing.
Waking Up With a Sore Throat? A Doctor Explains the Real Reasons Why
Waking up with a sore throat may seem like a minor irritation your morning coffee will wash away. But what if that discomfort is a red flag?
In my practice, I see this symptom frequently. It often signals a more severe issue: how you sleep, how you breathe, and what’s happening in your body overnight.
Mouth Breathing + Dehydration = The Perfect Storm
While you sleep, your body is in recovery mode. Ideally, you breathe through your nose, stay hydrated, and move through sleep cycles uninterrupted.
But for many people, that’s not the case.
If you sleep with your mouth open, you bypass the natural humidification and filtration system your nose provides. Air flowing through the mouth dries the delicate tissues in your throat. Add in the natural dehydration that occurs overnight (especially if you don’t drink water in the hours before bed or if you sleep in a dry room), and you’ve created a perfect storm for irritation.
The result is a dry, scratchy, sore throat.
Why Are You Mouth Breathing?
Mouth breathing is usually a compensation, not the preferred route. What’s forcing you to do it?
- Nasal Congestion — This is the most common cause. Allergies, chronic sinusitis, or even a deviated septum can block nasal airflow, especially when you lie down. Your body adapts by opening the mouth.
- Medications — Certain medications, especially anticholinergics, some antihistamines, and antidepressants, can dry out your mucous membranes. That makes your throat feel sore and irritated, even if you’re not fully congested.
- Alcohol and Caffeine — Both are dehydrating and can reduce REM sleep quality, indirectly contributing to poor breathing patterns and dryness.
- Sleep-Disordered Breathing — Conditions like sleep apnea or upper airway resistance syndrome often force the mouth open during sleep to maintain airflow. That contributes to dryness and inflammation over time.
When It’s More Than Dry Air
A dry room or low overnight humidity can cause a sore throat, but the persistence, severity, and associated symptoms differentiate between a benign cause and a more serious issue.
Here are red flags that warrant medical evaluation:
- You wake up tired, regardless of how long you slept.
- Your partner notices loud snoring or pauses in breathing.
- You wake with a sore throat and a headache daily.
- You have frequent nighttime awakenings with dry mouth.
- You also experience heartburn, hoarseness, or a bitter taste (suggesting reflux).
These symptoms may point to obstructive sleep apnea, nocturnal GERD, or chronic nasal obstruction. All are treatable and worth discussing with your doctor.
What You Can Do Tonight
If you’re ready to take action and wake up more comfortably, here are my top evidence-based strategies:
- Use a Nasal Saline Spray or Rinse — This clears congestion and supports nasal breathing.
- Try Nasal Strips or Dilators — OTC products like Breathe Right strips mechanically open the nasal passages.
- Use a Humidifier — Aim for 40–50% relative humidity in your bedroom.
- Hydrate Properly Before Bed — Stop caffeine and alcohol in the evening, and drink water throughout the day.
- Elevate Your Head — A slight incline can reduce reflux and improve nasal drainage.
- Consider Mouth Taping — For some patients, this encourages nasal breathing (only after nasal patency is confirmed).
Breathing Better at Night = Energy During the Day
How you breathe during sleep affects how you feel during the day.
Poor nasal airflow, disrupted breathing, and dehydration compound over time, affecting everything from immune health to mental clarity. Fortunately, with the right insight and small, consistent adjustments, it’s often fixable.
At Banner Peak Health, we treat every symptom like a signal. If you wake up with a sore throat regularly, it’s worth digging deeper. We’re here to help you breathe better, sleep better, and feel better.
CPAP Alternatives: Effective Options for Treating Obstructive Sleep Apnea
We lose muscle tone while we sleep, increasing the risk of our tongue falling backward and the collapse of our throat muscles.
When this happens, the result is obstructive sleep apnea (OSA): partial or complete blockage of the upper airway, interfering with air passage to and from your lungs during sleep. This interference reduces the amount of oxygen reaching the body and brain and releases adrenaline, hindering the body’s ability to sleep.
For those seeking CPAP alternatives, understanding how OSA affects your body is the first step toward effective treatment.
How OSA Affects Your Body
Normal sleep physiology occurs in stages, which I’ve written about extensively. OSA disrupts these stages because of hindered breathing, causing many serious problems.
In the short term, OSA can cause poor memory, headaches, and fatigue, which may cause the patient to fall asleep while driving. Long-term complications include:
- Increased risk of obstructive airway disease
- Heart attacks and congestive heart failure
- Non-alcoholic fatty liver disease
- Non-insulin-dependent diabetes
- High blood pressure
- Insulin resistance
- Atrial fibrillation
- Dementia
How CPAP Alternatives Impact OSA’s Effect on Hormones
Obstructive sleep apnea increases the release of stress hormones such as adrenaline and epinephrine.
OSA reduces these beneficial hormones:
- Human growth hormone (HGH): Repairs and builds muscles.
- Testosterone: Maintains sexual function and healthy body composition in terms of muscle mass and fat distribution.
- Estrogen: Maintains healthy body composition and bone health.
OSA increases these potentially harmful hormones:
- Cortisol: Impairs immune function and increases the risk of obesity.
- Leptin: Decreases satiety.
- Ghrelin: Increases appetite.
OSA’s Effect on Athletic Performance
Not only does OSA impair day-to-day functioning and increase the risk of long-term illnesses, but it also interferes with athletic performance in terms of strength, endurance, and cognition.
In 2013, the Journal of Clinical Sleep Medicine examined 12 middle-aged male golfers with severe OSA. The golfers underwent treatment with continuous positive airway pressure (CPAP). Then, after 20 rounds of golf, every golfer’s handicap index (HI) was evaluated.
While the non-OSA control group showed no improvement, the OSA group treated with CPAP improved by 11.3%, and the more skilled players (HI<12) improved by 31.5%.
I’m not a golfer, but I’ve worked with many and have recognized their devotion to the sport. This study proved they’ll do anything to improve their game.
For those who can’t tolerate CPAP, finding effective CPAP alternatives becomes crucial for health and performance.
Why Many Patients Seek CPAP Alternatives
CPAP treatments are effective and beneficial. However, patients often hesitate to discuss their OSA symptoms with a physician because they’re afraid they’ll be prescribed a CPAP machine.
CPAP (continuous positive airway pressure) is the gold standard for treating obstructive sleep apnea. Unfortunately, for most people, it evokes Darth Vader, with a face obscured behind a large mask.
Thankfully, CPAP machines have come a long way since their inception in the 1980s. They’re no longer vacuum cleaner-esque appliances. Even the full-face models are whisper-quiet. If you can’t stand the thought of reenacting the “Luke, I am your father” scene with your spouse every night, there are plenty of CPAP alternatives to choose from.
For severe OSA or mild-to-moderate OSA with risk factors for complications such as heart attack, AFib, or stroke, the first choice and standard of care is a CPAP machine. But if you suffer from mild-to-moderate OSA and/or a CPAP machine is off the table for you, you may benefit from a CPAP alternative.
The Evolution of OSA Diagnosis and CPAP Alternative Treatments
The old-school diagnosis of obstructive sleep apnea required an overnight polysomnogram (at a sleep study facility) with 22 wires attached to you. If you received a diagnosis of OSA, a CPAP machine prescription followed. It wasn’t practical to repeat the sleep study to assess how well the CPAP machine worked.
At-home sleep studies and sleep-tracking tools (such as SleepImage) have since improved OSA treatment. These advancements enable effortless multi-night testing in the comfort of your own home, allowing for a trial-and-error approach to OSA treatment. This is revolutionary not only diagnostically but also therapeutically when exploring CPAP alternatives.
Stacking CPAP Alternatives for Effective Treatment
Stacking modalities means combining multiple therapies. Each individual therapy may offer only a minimal benefit, but together, they provide improvement. Each person can experiment with combining a variety of treatments to achieve a successful outcome, rather than reaching for the biggest gun (i.e., CPAP) first.
At Banner Peak Health, we use SleepImage and collaborate with Empower Sleep. We also consider adding other CPAP alternatives to the stack, including tools that:
- Improve nasal patency: Nasal steroids, nasal strips, and nasal dilators improve airflow through the nostrils.
- Minimize mouth breathing: Tools like external straps and tape close the mouth and encourage nasal breathing. These tools also hold the tongue in a more forward position and prevent it from falling backward as we sleep, where it might obstruct the airway.
- Improve sleep position: Pillows and wedges prevent people from sleeping on their backs. A supine (lying flat on the back) position puts a person at risk of obstruction, and gravity compounds this risk. Side sleeping helps stabilize the throat muscles so they don’t collapse and interfere with air passage in and out of our lungs.
- Improve tone and tongue position: eXcite OSA and REMplenish Straw are like push-ups for your tongue. Mandibular advancement devices like myTAP and Zyppah bring the lower jaw forward. Since the lower jaw anchors the tongue, this repositioning reduces the obstruction risk by keeping your tongue clear of the airway.
- Modify airway pressure (without CPAP): Try Bongo Rx for increased expiratory positive airway pressure.
Today’s Takeaways
Sleep is the foundation of good health. That’s why Banner Peak Health stays at the cutting edge of sleep science. We’re always brainstorming new ways to maximize and optimize your sleep.
Reach out today and tell us about your sleep concerns. We can help you explore both traditional CPAP therapy and effective CPAP alternatives tailored to your needs.