How to Be a Critical Reader of Medical Articles in the Lay Press
We’re officially in the throes of an “infodemic.” Every day, we’re inundated with more information than we can process about a variety of topics, especially medicine.
Why is this happening? One reason is that there exists a bias in medical literature reporting. Every individual and institution in the research process has the potential to overinflate their findings’ value, seeking to gain greater exposure from the press.
Researchers are also pressured to produce noteworthy results. Impressive studies endow prestige and enhance scientists’ and journalists’ careers. Because there’s so much at stake, there’s a tendency to mislead with less-than-accurate information.
Combine that with the press’s tendency to report overly optimistic or frightening statistics. Their goal is to get readers to click, read, and subscribe.
I want to give you the skills to navigate this infodemic of medical literature. Once you finish this post, you’ll be able to read critically and discern between relevant data and sensationalism.
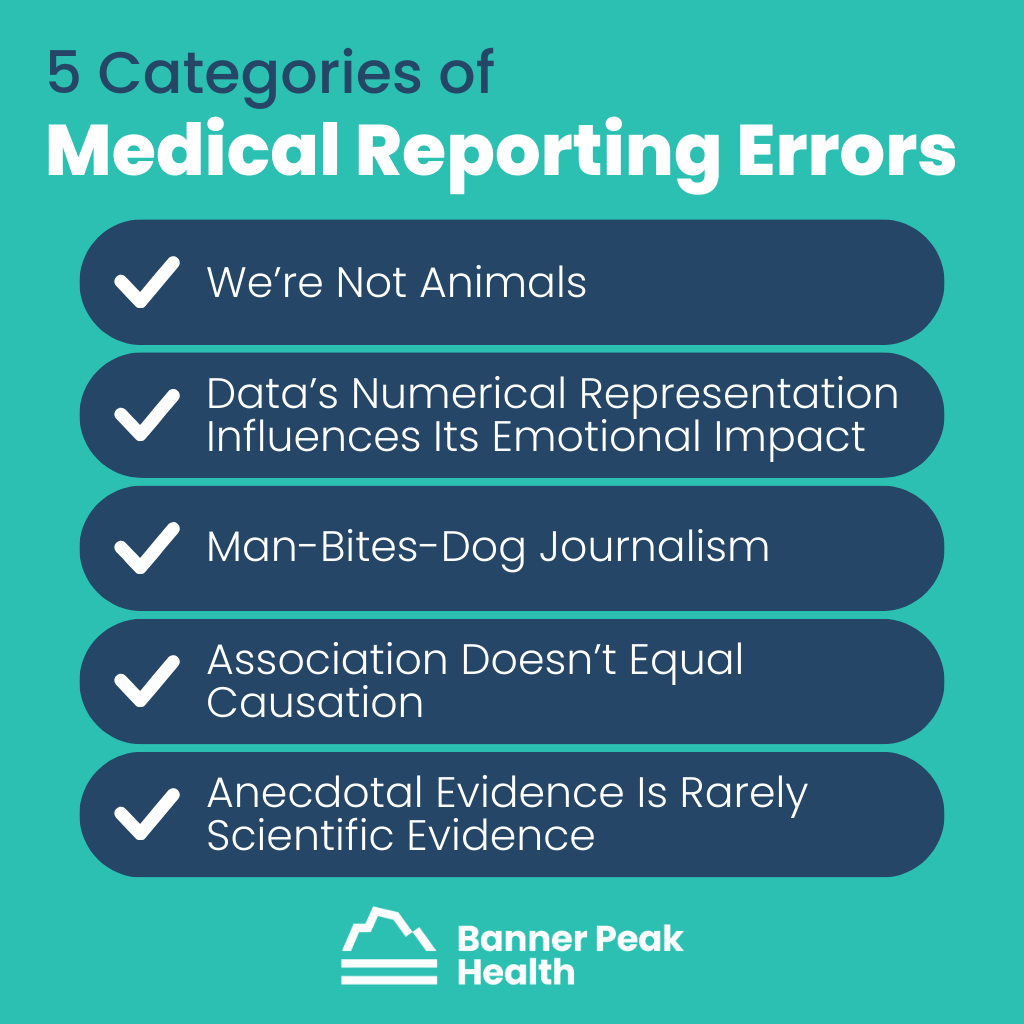
5 Categories of Errors
I’ve identified five categories of common medical reporting errors.
1. We’re Not Animals
We have neither fur nor tails, yet many studies found in medical literature involve animals.
Animal experimentation is part of our research method. Only a minute percentage of discoveries from animal models ever impact human healthcare. Regardless, these studies often excite the press.
Example: Taurine is an amino acid shown to improve health and extend lifespan in mice. However, because of inherent physiological differences, there’s almost no chance this will ever be relevant to humans.
2. Data’s Numerical Representation Influences Its Emotional Impact
Data often tells more than one story, and journalists are storytellers. That can be a dangerous combination.
When the press presents the same data in multiple ways, people can interpret it differently, and the information can have various emotional effects. It can even influence public policy.
Example: The Women’s Health Initiative, which began in 1991, explored hormone replacement therapy (HRT) in postmenopausal women.
One randomized part of the study examined 16,000 women. In a subset study, 678 women — 385 from the HRT group and 293 from the placebo group — received a breast cancer diagnosis.
In 2005, the press reported those results as a 23.5% increased risk of breast cancer from HRT, a frightening finding. This statistic is true, breast cancer did occur at a rate of 0.42% per year in the drug group and 0.34% in the placebo group.
However, the results are more nuanced than that. Each year, for every 1,000 women in the trial, an average of 4.2 women on HRT could expect a breast cancer diagnosis, while an average of 3.4 women on the placebo could expect the same. There was a difference of only one woman per 1,000 each year between the two groups.
The press chose to express the data in a sensational way to entice readers to click on headlines and purchase newspapers. That single statistic changed women’s healthcare for over 20 years. Doctors and patients have been fearful of estrogen replacement therapy. As a result, an entire generation of postmenopausal women have been fearful of using a relatively safe treatment.
3. Man-Bites-Dog Journalism
Science is rarely about the result of any single study but the preponderance of evidence based on the compilation of many studies. However, when a touted study contrasts prevailing wisdom, it’s more likely to appear in the press. Journalists’ prerogative is to grab attention, and contrarian headlines accomplish that.
Example: In 2017, the Independent ran an article quoting one doctor who said, “Sugar benefits your brain health.”
This article expressed the opinions of a single doctor, who states that sugar may not be as harmful as we think it is.
It only became popular because it’s an assertion that goes against prevailing wisdom. In science and medicine, beware the contrarian.
4. Association Doesn’t Equal Causation
Human beings are not lab animals, particularly regarding our diet. It’s impossible to run randomized control trials on humans because we can’t control and measure everything test subjects eat against a control group.
Therefore, we rely on epidemiologic studies, which examine differences in people’s eating habits and try to correlate them with different health outcomes. Unfortunately, this form of study is notoriously susceptible to identifying associations that aren’t necessarily causal.
Example: For many years, red wine was believed to confer a health advantage. The consumption of red wine is associated with many other healthful behaviors, such as eating fresh fruits, vegetables, and healthier oils. Therefore, red wine is a confounder — associated with better health, but not causal.
Nutrition literature is particularly prone to miraculous attributions to certain foods.
5. Anecdotal Evidence Is Rarely Scientific Evidence
Anecdotal evidence may be exciting and compelling, but it’s rarely enough to inform or change the practice of medicine.
Example: The media is full of anecdotal evidence from people who successfully combatted their COVID-19 symptoms using ivermectin or azithromycin, both of which have been proven ineffective in randomized control trials.
Today’s Takeaways
Before you become too excited or too frightened by a medical article, remember the following:
- Humans are not animals.
- Be leery of data expressed as percent change rather than an absolute number.
- Beware the contrarian. Don’t take it at face value if something goes against all conventional thinking.
- Association does not equal causation.
- Sample size matters. Don’t extrapolate universal truths from single or small sets of unique events.
There are always exceptions to these rules. Every day, the media reports valid science, and every day, they sensationalize. By being an informed, discriminating reader, you’re better equipped to find the kernels of truth and stay above the fluff.
Our First Year Using an InBody Device (And What It Is)
An InBody machine provides body composition information, including fat weight, water weight, and dry lean mass (muscle, bone, and connective tissue). It allows for a more accurate description of a patient’s body composition than BMI.
This article will answer the question, “What is an InBody scan?” and explain what we’ve learned since acquiring our InBody device.
InBody at Banner Peak Health
We were excited to introduce our InBody device in January 2023.
What is an InBody scan? It’s a bioelectrical impedance analysis for determining what percent of a person is water weight, muscle weight, and fat weight.
A patient stands on the InBody device and holds an electrode in each hand. The device sends an imperceptible current across different axes generated from those four contact points.
The device calculates the resistance across each axis and diagnoses what percentage of the patient is water, fat, and muscle. It’s able to accomplish this due to a fundamental chemical difference between water and fat: water conducts electricity, while fat insulates.
Stepping on a scale doesn’t give us clinically vital information regarding the body’s composition. InBody does.
Our Biggest Insights
Anyone looking in a mirror or stepping on a scale can tell whether they’re overweight. When we started using our InBody scan, we weren’t surprised by the fat content results we saw. However, other results did surprise us.
Sometimes, patients who appeared healthy found out they weren’t as healthy as they thought. Their muscle mass was declining, and they were at risk for sarcopenia. (More on this later.)
Other patients who expected poor results because they were overweight had excellent muscle mass. Hidden in their bodies were real athletes!
We give credit where credit is due. InBody scans help us diagnose and treat every patient appropriately.

Muscle Mass Matters Most
You can’t tell someone’s muscle mass just by looking at them. That’s where InBody comes in handy.
Muscle mass predicts longevity and level of function in later adulthood (age 50+). If we identify and enhance muscle mass in middle age, we can improve the quality and duration of our lives.
It’s also imperative to diagnose and prevent sarcopenia — the decline in muscle mass associated with age. With InBody’s help, we can treat and correct sarcopenia more effectively.
Strength Training
When we discover a patient is at risk for sarcopenia, we recommend strength training and other regimens. For some, this means taking advantage of gym memberships or arranging sessions with a fitness instructor.
Some older patients may use wheelchairs but still need to practice strength training. We send Zoom links for exercises they can do while seated.
Protein Intake
Protein intake is also crucial for building muscle. The current recommended daily allowance (RDA) is 0.8g of protein per kilogram of body weight, according to the FDA. However, experts like Peter Attia recommend 2g per kilogram of body weight (2.5 times the RDA).
The RDA is the minimum amount necessary to stave off a disease state, while Peter Attia’s recommendation advocates maximizing your health state. I target somewhere between the two to enhance patients’ health.
Not all proteins are equal. For example:
- 1g of animal protein is not the same as 1g of vegetable protein.
- The ratio of amino acids in different proteins varies.
- Each type of protein has a different bioavailability.
If you’re not careful, you can exceed your recommended caloric intake. We’re exploring various supplement options as a means to avoid this.
We’re also looking into branched-chain amino acids, a potent form of amino acid supplementation that may preserve muscle mass. Because there is such a wide array of commercial products available, I’m uncomfortable making a pronouncement until I know more.
Tracking What Happens to Muscle Mass During Weight Loss
Successful weight loss involves expending more calories than you ingest. Ideally, we want fat to provide that excess energy, but we don’t always get what we want.
For most weight loss regimens, we expect to lose 75% of weight from fat and 25% from muscle mass. However, we’re finding through InBody scans that when patients use weight-loss medications like Ozempic and Mounjaro (which have GLP-receptor agonist activity), that ratio can be as high as 60% fat loss and 40% muscle loss.
For some patients, this is problematic or even dangerous. By monitoring muscle mass and recommending increased protein intake as well as strength training, we can mitigate the risk of these weight loss medications.
Today’s Takeaways
In addition to the traditional metrics of weight and blood pressure, we now also track muscle mass. InBody provides a more nuanced look into a vital health status.
At Banner Peak Health, we’re always excited to implement new technology that helps us gain insights into each patient’s health status.
So, what is an InBody scan? It’s one of the latest tools that allows us to provide state-of-the-art medical care. It has reinforced that preserving muscle mass is essential to living a long, healthy life.
Does a Meniscus Tear Need Surgery?
It was a warm fall afternoon, and I was running in the hills above Berkeley when I felt a sudden pain in my right knee. No negotiation possible; I had to stop running. Unfortunately, I still had to walk a few miles to my car, and that’s how my persistent pain started.
The pain persisted and I had to acknowledge that my knee wasn’t going to improve on its own. After a visit to an orthopedist and an MRI, I received my diagnosis: a degenerative meniscal tear in my right knee.
I had the same questions any patient would have in this position, including, “Does a meniscus tear need surgery?” Here’s what I’ve learned both from personal experience and medical literature.
What Is a Meniscus Tear?
The meniscus is a figure-eight-shaped fibrocartilaginous “washer” that cushions the knee between the femur (on top) and tibia (on bottom). Meniscus tears or injuries are common and result from either acute or degenerative mechanisms.
Acute injuries occur when a single force overwhelms the structural integrity of the joint, like when a 17-year-old soccer player gets slammed from the side. That acute force overloads the knee’s structural anatomy and damages the meniscus.
Degenerative injuries occur as a result of wear and tear over time. For example, in my case, I’d been running regularly for decades, and that repetitive force caused my meniscus to gradually wear down until it tore in 2005. I had a pothole inside my medial meniscus, which caused pain, low-level swelling, and walking impairment.
Does a Meniscus Tear Need Surgery? My Options
I discussed the options with my orthopedist and decided to try physical therapy. If my knee didn’t improve, we’d consider surgery.
I embarked on six to eight weeks of physical therapy, including exercises to strengthen my quadriceps and increase my hamstring flexibility. I also refrained from putting force on my knee by running.
Within two to three months, I was back to baseline function and could bike, hike, and run.
Don’t Shoot the Messenger… Listen to It
Medicine often falls into the cognitive trap of “shooting the messenger.” It’s an idiom from ancient Greece, when a messenger had to deliver bad news to a king and lost his life for his trouble.
In modern medicine, the injury is the messenger, not the beginning of the story. The meniscal tear communicated a problem. Why did the tear happen in the first place?
My orthopedist saw the injury as the problem and didn’t go upstream to explore what about my body, structurally or ergonomically, had created the injury.
So, I worked with a podiatrist and did a gait analysis. We modified an insole and created a lifelong physical therapy routine to strengthen my core and stabilize my leg.
I was relieved to heal without needing surgery. I heeded the message to try to build back better and avoid future injuries.
Take Two
Seventeen years later, while on vacation in Hawaii, I felt a low-level pain in my left knee. It was less severe this time, so foolishly, I continued to run for several weeks before addressing it.
After an evaluation with a sports medicine doctor and another MRI, I discovered I had another meniscal tear, this time in my left knee. However, this tear was complex. Instead of being a two-dimensional problem, part of the tissue had flipped up and occupied more of the joint space.
If my right knee had a small “pothole” in the meniscus that needed to heal, my left meniscus had the equivalent of a raised bump, like a pebble stuck between a foot and shoe.
This time I asked, “Does a meniscus tear need surgery if it’s complex?”
A Landmark Study
In 2013, the New England Journal of Medicine published a landmark study noting that arthroscopic partial medial meniscectomy (removing the damaged part of the meniscus) occurred in about 700,000 cases annually (at the time of the study), making it one of the most common orthopedic procedures performed.
My case matched perfectly with those in the study. The test population involved 35- to 36-year-olds with no underlying arthritis who had undergone a degenerative tear. Remarkably for a surgical study, the design included placebo controls. Half received the arthroscopic partial resection of part of their meniscus, and the other half underwent surgery with arthroscopy with no tissue removed.
The results showed that 12 months after surgery, there was no difference in functional capacity or pain between those who had received the real or sham surgery. This was a shocking result, demonstrating the body’s ability to heal from these types of injuries without any surgery.
The problem with partial meniscectomy has to do with the meniscus’s anatomy. Since it’s fibrocartilaginous, there’s little to no blood supply, so the part surgeons remove won’t grow back. The knee must continue to function with less of that figure-eight donut cushioning each impact between the femur and tibia. Over time, forces are applied to less of a cushion between the femur and tibia, increasing the forces applied directly to the bone and the risk of osteoarthritis.
Making My Choice
After considering the potential long-term complications of surgery and the randomized control trial’s results, I decided to give physical therapy a shot.
I wish it had gone as smoothly as it did in 2005, but there’s a difference between healing at 40 and healing at 60. The tears’ anatomies were also different, and the second, more complex tear posed a greater challenge.
I aggressively pursued physical therapy, and the fear of surgery and its attendant risk of osteoarthritis compelled me to remain diligent. I slowly regained function and reduced pain.
As of this writing, I still refrain from running. I can hike, bike, and backpack, but I modify my ergonomics.
What Was This Injury’s Message?
While working with a physical therapist, I learned that I had a reduction in right ankle flexion and tightness in my hamstrings. I’m now addressing the root causes of my left knee injury to prevent future issues.
Physical therapy is not just about regaining function after an injury. It’s about addressing why you had the injury and working to prevent future ones.
People undergoing physical therapy, and many doctors prescribing it, often miss that point. Emphasizing it will give people further incentive to do the hard work physical therapy requires.
Today’s Takeaways
- If you’re asking, “Does a meniscus tear need surgery?” after suffering a meniscus tear, the answer is, “Only as a last resort.” If all else fails and multiple surgeons recommend it, it’s a valid option. Until then, focus on physical therapy.
- Physical therapy reduces the risk of future injuries and helps correct the structural problems that led to the initial injury.
Take physical therapy seriously. Your knee’s life depends on it.
12 Colonoscopy Prep Hacks for Better Results
We often think of a dichotomy between “book smarts” and “street smarts” — the different perspectives gained from academic learning versus experiencing the hard knocks of life.
As physicians, we begin our careers with an abundance of book smarts. As we age, experiencing illnesses and medical procedures ourselves, we also acquire street smarts.
A physician with both book and street smarts is more empathetic to his patients. He has a more nuanced view of the small details that can sometimes be game-changing.
In keeping with our mission to promote better health through comprehensive preventative healthcare, I’d like to share some of the colonoscopy prep hacks I’ve learned from the two colonoscopies I’ve undergone.
12 Colonoscopy Prep Hacks
Colorectal cancer is the third-leading cause of cancer deaths in the United States. The American Cancer Society estimates that over 50,000 Americans will die from colorectal cancer in 2023 alone. Regular screening tests for colorectal cancer are essential, and several screening methods are available.
Screening modalities for colorectal cancer range from submitting a small amount of a bowel movement for analysis, to a colonoscopy with a fiber optic scope, which inspects the entire length of your colon. Today, I’ll discuss the latter.
Some of these colonoscopy prep hacks I learned the hard way, some with the help of friends, but I’ve found all of them helpful.
Hack #1: Don’t Procrastinate
Get your screening when your physician advises it. My doctor told me to get my first colonoscopy at age 50, but I dragged my heels until age 51.
Please do as I say, not as I did. At that time, the recommended age for an initial screening was 50. However, we’ve seen a rising prevalence of colon cancer in people under 50, so the recommended age to begin screening is now 45.
I should’ve followed my physician’s directions, and that’s my advice for you. Don’t wait.
Hack #2: Don’t Be Afraid to Negotiate With Your Gastroenterologist
Colonoscopy prep has come a long way from receiving a gallon or two of foul-tasting liquid to drink. Now, there are pills and liquid concentrates. I recently used Plenvu, which is a 16-ounce concentrated liquid you dilute with a quart of water and drink.
Discuss with your doctor which kind of prep would work best for you.
Hack #3: Discuss All Your Medications and Supplements With Your Gastroenterologist Ahead of Time
Some medications, such as aspirin and Motrin, act like blood thinners and need to be withheld before the procedure. If not, you’ll have to delay and reschedule your colonoscopy, and all that prep will have been for nothing.
Hack #4: Consume Adequate Calories Before Your Colonoscopy
During your prep, you’ll be on a clear liquid diet. Most people stick to bouillon broth, but it has very few calories and exacerbates the physical weakness the preparation causes.
I suggest a high-calorie sports supplement called Hammer Gel, which contains 90 calories per ounce. You can sip this throughout your prep day to get as many calories as needed.
Note: Your gastroenterologist won’t want you to consume any food with red, purple, or pink dye during your prep. Those dyes make it difficult to view the colon’s lining because they distort the colors seen there. However, you can ingest yellow-colored food without causing a problem.
Hack #5: Make Your Prep Liquid More Palatable
Most prep liquid is extraordinarily foul-tasting. Add a flavoring agent like Crystal Light (yellow only) to make it less so.
Also, take advantage of the fact that your body’s neurons are temperature-sensitive. Numb your taste buds by making the prep liquid as cold as possible.
Hack #6: Charge Your iPad
Once you start your prep, don’t expect to leave the bathroom. There’s no point in commuting. So, make sure you charge your tablet ahead of time so you’ve got something to do while the prep does its job.
Hack #7: Maintain Fluid Balance
Don’t get so distracted by the fluid leaving your body that you forget to have fluid enter your body. Balancing fluid intake is essential.
Hack #8: Dress Warmly on the Day of the Procedure
Dehydration makes you intolerant to the cold. Expect to feel chilly on the day of your procedure. Wear a sweater or jacket.
Hack #9: Don’t Expect to Remember Anything
When you wake up from anesthesia, your gastroenterologist will tell you the preliminary results of your procedure. However, the anesthetic will not have worn off completely, leaving you amnestic (forgetful). Don’t expect to remember what your gastroenterologist says.
This is also why you can’t drive yourself home on the day of your procedure.
Hack #10: Bananas to the Rescue
This is one of the easiest colonoscopy prep hacks. In addition to dehydration from fluid loss, you’ll also lose significant amounts of potassium during your prep.
Bananas are one of the best natural sources of potassium. Try to eat between two to four bananas throughout the day after your colonoscopy. Bananas also slow down bowel transit time, so if your prep is still doing its job after your procedure, bananas will normalize the situation.
Hack #11: Don’t Worry if You Have No Bowel Movement for 3 Days
If you don’t have a bowel movement for a few days after your colonoscopy, you’re not constipated. The prep completely clears out the GI system, and food can take up to three days to travel from your mouth to the other end. Restarting the assembly line of your digestion can take time.
Hack #12: Follow Your Gastroenterologist’s Recommendation for a Follow-Up
Based on your results, your gastroenterologist may recommend you have a follow-up colonoscopy in one to 10 years. Follow that advice for the best chance of preventing colorectal cancer.
Final Thoughts
Although it’s certainly not how any of us would choose to spend a day or two, colonoscopies are necessary to maintain our health as we age. Hopefully, these colonoscopy prep hacks will help you face your next (or first) colonoscopy with less dread and discomfort.
Best Supplements and Vitamins for Anti-Aging
I loved the movie The Wizard of Oz as a child. I think the message holds true and applies to our quest for anti-aging solutions.
The characters in The Wizard of Oz discover that the qualities they sought lay within them all along. Similarly, our strongest data regarding longevity rests on individual behavior centered around diet, exercise, sleep, and emotional connection.
Rather than looking toward supplements and vitamins for anti-aging, we should first explore more holistic means of improving our long-term health.
A Flooded Market
There’s a growing list of medications and supplements touted to prolong life. Experts expect the global anti-aging market to increase by 13% annually through 2030, meaning everyone who wants to make a buck on vitamins for anti-aging will have no problem doing so.
The media obsessively pursues “the next big thing” on the market, publishing all the clickbait they can to facilitate its success. All this hype leads to a lack of healthy skepticism regarding the data behind these new products (e.g., metformin, rapamycin, taurine, and resveratrol).
What’s the Problem?
The problem with these new interventions is the weak or nonexistent data supporting them.
Humans aren’t lab rats. Given the inherent duration needed for study (a lifetime) and its complexity, it’s almost impossible to perform a randomized controlled trial for most, if not all, of the anti-aging supplements on the market.
We’re not talking about a 12-week trial to test whether one’s cholesterol decreases. Testing to determine whether humans live longer is much more complicated and time-consuming.
Because we don’t have access to the gold standard of evidence — randomized controlled trials — we must extrapolate from inherently flawed experimental methods.
For example, many dietary supplements go through epidemiologic studies that aren’t randomized. They simply observe who eats or doesn’t eat and look for correlative outcomes.
One problem here is the presence of confounders. Another problem is that we’re forced to rely on animal models. Animals and humans differ in many ways, so results don’t always correlate.
Examples of Popular Products and Insufficient Studies
The following two examples are popular supplements hailed by the media as keys to longevity but which currently lack sufficient study and evidence.
Resveratrol
Resveratrol is a natural polyphenol found in red wine. Its study harbors a classic example of a confounder.
Many claim the resveratrol found in red wine is the answer to the “French paradox” (the generally low rates of heart disease observed in French people).
The flaw in this logic is something called a healthy user bias. This means the people consuming the wine are inherently different from those who don’t (i.e., higher socioeconomic status, greater consumption of fruits and vegetables, etc.). These variables likely have as great an impact on the user’s health as intake of resveratrol.
Furthermore, no current data supports the idea that resveratrol helps people (or animals) live longer.
Taurine
Taurine is an amino acid that our bodies produce. It has many functions, including as a neurotransmitter in the brain. While animal studies have shown links between taurine and longevity in worms and rodents, animal models aren’t always useful for human applications.
For example, the animal models supporting intermittent fasting were originally derived from mouse models. The conclusion: Eat all your meals within an eight-hour window and fast for 16 hours a day.
The caveat here is that a mouse will die after 48 hours without food. So, for a mouse, a 16-hour fast is one-third of the duration until death. That duration doesn’t correlate with the intermittent fasting we recommend. Humans can go an average of three weeks without food, so an equivalent fasting duration would be one week.
So, as Peter Attia puts it, taurine may be the “elixir of life if you’re a mouse,” but humans don’t manufacture, absorb, or excrete taurine the same way mice do. Therefore, the studies examining mice and taurine aren’t as useful as some would like to believe.
Today’s Takeaways
Given our imperfect data, our best anti-aging bet is to go back to the basics — risk versus reward.
Everything we recommend regarding nutrition, exercise, sleep, and social connections is the best we can offer. We know these measures improve longevity, and they’re 100% safe.
While the world tells you to “click here!” to order supplements or vitamins for anti-aging, remember there’s a man behind the curtain. The journey down the yellow brick road is more important than what lies at the end.
The Therapeutic Benefits of Nature
Whether I’m biking, jogging, or walking my dog, exercising in nature has always been my go-to stress reliever.
Some people prefer to exercise in the morning, checking it off the list to get it out of the way. I enjoy exercising at the end of the day to unwind from work.
This wasn’t always the case. In college, I’d go on long runs in the park before stressful tests. I remember one test in organic chemistry. I hadn’t timed my run properly and literally had to run to the lecture hall and take the test in my running gear.
I pitied the students who had to sit next to sweaty me, but I aced the test, did well as a premed, and the rest is history.
My personal experience has convinced me of the tremendous value of both exposure to nature and exercise. Is there any scientific data to validate the benefits of exposure to nature?
What Science Says About the Benefits of Nature
Delving into the literature around the therapeutic benefits of nature exposure reveals a large body of evidence associating nature exposure with a wide range of benefits. These benefits include stress reduction, better sleep, less depression, better cognitive function, lower blood pressure, better immune function, better post-op recovery, and more.
However, as we’ve mentioned in previous blog posts, correlation doesn’t equal causation. For example, access to parks correlates with higher socioeconomic status, and the decision to visit a park correlates with a higher level of physical function.
Very few gold-standard randomized controlled trials have successfully isolated the intervention of exposure to nature. However, I did find one notable study.
The Experiment
In 2018, a group of researchers from the University of Pennsylvania worked with a nonprofit to explore the therapeutic impact of “greening.” Greening is the process of cleaning up an urban property and planting live plants to “green up” the space.
This experiment used 110 clusters containing 541 vacant lots in areas of lower socioeconomic status in the city of Philadelphia. These lots were often blighted with graffiti, abandoned cars, and garbage.
The experimental methodology was this:
- One-third of the lots were cleaned up, planted as green space, and fenced off.
- One-third of the lots were cleaned up and fenced off but had no additional greening.
- One-third of the lots were left untouched (control group).
The researchers identified 442 participants in the neighborhoods adjacent to these areas and performed a mental health questionnaire before the intervention and again 18 months later.
The researchers documented that the participants adjacent to the green space versus the control spaces experienced a 41.5% reduction in depression and a 62.8% reduction in feelings of worthlessness.
This study gives plausibility to the mechanisms of all other association trials. Since strictly randomized controlled trials are so difficult in this case, the fact that this one demonstrated that nature exposure could be beneficial lends credence to other studies.
The full health benefits of nature walks, mountain biking, swimming, jogging, and anything else we enjoy doing outdoors may not be completely documented, but they’re worth investigating.
Is Data Necessary?
As we’ve said in recent posts, when in doubt, it’s often best to calculate risk versus reward.
If a situation involves significant risk, we need ironclad data from reproducible, randomized controlled trials showing a benefit to warrant the risk.
Take chemotherapy, for example. It involves tremendous risk to the patient, so we rely on the decades of study available to show us the benefits of the treatment to weigh whether the risk is worth it. The answer depends on each individual and their unique situation.
However, nature exposure is at the opposite end of this spectrum. There’s almost no risk for most people to spend time in nature, and the potential benefits are great. Because of this, we don’t need stacks of data from decades of gold-standard studies.
Today’s Takeaways
We’ve explored the potential risks and benefits of exposure to nature and green spaces. It’s safe to say the benefits far outweigh the risks for almost everyone. To offset even minimal risk, remember these tips:
- Always wear sunscreen — you can get sunburned even when it’s cloudy.
- Stay hydrated — drink plenty of water when it’s hot.
- Maintain situational awareness — watch your step if there are dogs around.
- Have fun and improve your health — find the best way for you to enjoy nature’s benefits.
Fall Vaccine Update 2023
Autumn, a time for changing seasons, beginning school, and thinking about vaccinations. This year there are three vaccines to discuss: influenza – the perennial classic, COVID – becoming a new tradition and Respiratory Syncytial Virus (RSV) – the new kid on the block.
RSV can cause mild cold symptoms such as coughing, fever, congestion, and sneezing. Symptoms can last for a week or two. Unfortunately, two groups of people are at risk for more serious outcomes. Children under five are more susceptible to bad outcomes with 60,000-80,000 hospitalizations and 100-300 deaths per year. Also, for those over 65 there are 60,000 – 150,000 hospitalizations and 6,000-10,000 deaths per year.
The Fall and Winter of 2022-2023 was one of the worst RSV seasons in recent memory due to many people coming out of COVID isolation and gathering with each other in larger numbers spreading the illness through society. The rate of hospitalizations for those over 65 shot up two-fold. Because there is no specific treatment for RSV in adults, other than supportive care, there is a great need for preventative treatment such as a vaccine.
In the Summer of 2023, CDC’s Advisory Committee on Immunization Practices (ACIP) met to evaluate two new RSV vaccine options: Abrysvo by Pfizer and Arexvy by GSK. Both have been approved for use in those over 60 years old and are currently available. Both pharmaceutical companies are in the midst of marketing campaigns for the vaccines. You may have, or will soon, see their advertisements.
For better or worse, practicing medicine during the COVID pandemic has led to diminished trust in our federal health agencies, creating healthy skepticism and a desire to more critically examine their decisions. At Banner Peak Health, we have reviewed some of the data submitted to the CDC for the two RSV vaccines and have come to our own conclusions.
Both vaccines underwent randomized controlled trials. Ideally, we would have wanted to see evidence of a reduction in hospitalizations and deaths due to RSV. Unfortunately, the two studies didn’t have enough participants to be able to document these critical outcomes. The studies only demonstrated a reduction in illness and symptoms not severe enough to lead to hospitalizations. Furthermore, several hundred people would need to receive the vaccine for every one episode of this level of illness avoided.
Most concerning for these vaccine side effects was their rate of two potentially fatal autoimmune central nervous system diseases, Guillain Barre Syndrome and Acute Disseminated Encephalomyelitis. These were very rare complications occurring in 1 out of 7,500 to 15,000 study participants. However, this rate is much higher than normal in the population and much higher than the rate observed in other vaccines such as influenza and Shingrix (shingles).
How to interpret this data?
These vaccines may be powerful tools for reducing hospitalizations and deaths from RSV, and their rate of dangerous autoimmune complications may have been overstated in these trials to due the randomness associated with the trials. Only a handful of cases occurred. However, the data submitted to the CDC does not support the pharmaceutical companies’ recommendation that everyone over the age of 60 receive the vaccine. The risk/benefit ratio based on the existing data is not strong enough. Basically, more studies and time for follow-up are needed to better understand the strengths and weaknesses of these vaccines.
Nonetheless, RSV is still a potentially lethal disease for those with high-risk health conditions. For these individuals, the protection from the vaccine outweighs the very small risk of a side effect.
In the meantime, our policy at Banner Peak Health:
- If you or a family member are at high-risk for a bad outcome from RSV, please get the vaccine. It is now available at local pharmacies. We define high risk as having a compromised immune system due to illness or medication, current cancer treatment, as well as a severe illness affecting your kidneys, heart, or lungs. If you are uncertain as to your status, please contact us to discuss the issue.
- Everyone else should wait. Hopefully, by next year, we will have more complete information to assess whether to use the vaccines.
Brief COVID Update:
The worst of the pandemic may be over, but COVID is still with us. We are in yet another surge, driven by the emergence of a new variant dubbed Eris- EG.5 (XBB1.9) which currently makes up around 15% of reported cases. Eris can be thought of as the grandchild of Omicron; it’s still highly contagious, but not causing as severe a disease as some of the original variants which have vanished from the human population. So far, Eris symptoms are like previous Omicron variants, possibly with less loss of taste and smell than its grandfather Omicron.
A new vaccine targeting a more recent variant, Omicron XBB.1.1.5, should be available in late September or early October. Raising the question, get the existing bivalent COVID booster now or wait and get the newer version?
We recommend waiting for the newer vaccine which more closely targets the current variant and should be available in a few months. However, if you are planning on traveling or have a high-risk gathering planned, you will need protection sooner and would benefit from getting the current vaccine as soon as possible.
Influenza:
The theme of appropriate timing applies to influenza vaccination as well. We will have our influenza vaccines in early September. The high dose Fluzone vaccine is recommended for everyone over 65, and Flublok is for those under 65 or anyone with an egg allergy. We prefer Flublok over other quadrivalent vaccines because it is less allergenic (not grown in eggs) and more potent since it contains a higher amount of hemagglutinins than the standard quadrivalent flu vaccines offered in the pharmacy.
We recommend that you wait until October to receive your influenza vaccination. A slight delay ensures that the 3-4 months of peak protection will cover a bit later into the flu season which often peaks a bit later here in California. However, if you plan to travel in October, receiving the vaccine in September is okay to ensure adequate time to respond to the vaccine before traveling.
What about receiving more than one vaccine at a time? Not a good idea. Simultaneous vaccinations increase the side effect burden and can create uncertainty as to which vaccine you had a reaction to.
In Summary:
For RSV, unless you or a family member are high risk, please wait to receive the vaccine this season. We define high-risk as having a compromised immune system due to illness or medication, current cancer treatment, as well as a severe illness affecting your kidneys, heart, or lungs. If you are uncertain as to your status, please contact us to discuss the issue.
For COVID, please wait for the release of the new COVID vaccine due in late September or early October.
If you are planning to travel or have high-risk gatherings planned, and it’s been more than four months since your last booster or infection, please get a booster now.
For influenza, please wait until October to ensure that your maximum antibody levels will remain effective throughout the flu season. You can be vaccinated at a pharmacy, or we will have a series of flu vaccine clinics later in the Fall. It is okay to receive the flu vaccine in September if you plan to travel in October.
Please contact us with any questions.
How Does Garmin Measure Stress?
Garmin and other wearables that measure heart function quantify stress. But how does Garmin measure stress, exactly?
These devices use heart rate variability (HRV) to quantify stress levels. But is HRV an accurate way to measure stress? The short answer is yes, absolutely.
But now that we can measure our HRV and determine our stress levels with wearables like Garmin, what do we do about it?
That’s what we’ll cover in this post.
Your HRV Is Like a Tesla
I like cars. In 2019, I was fortunate enough to get a Tesla Model 3.
There aren’t many gauges on an electric vehicle’s dashboard, but there is a charge indicator that tells whether you’re consuming electricity (by accelerating onto the freeway or climbing a steep hill, for example) or recharging your battery. As humans, we have a comparable gauge — heart rate variability (HRV).
Let me explain.
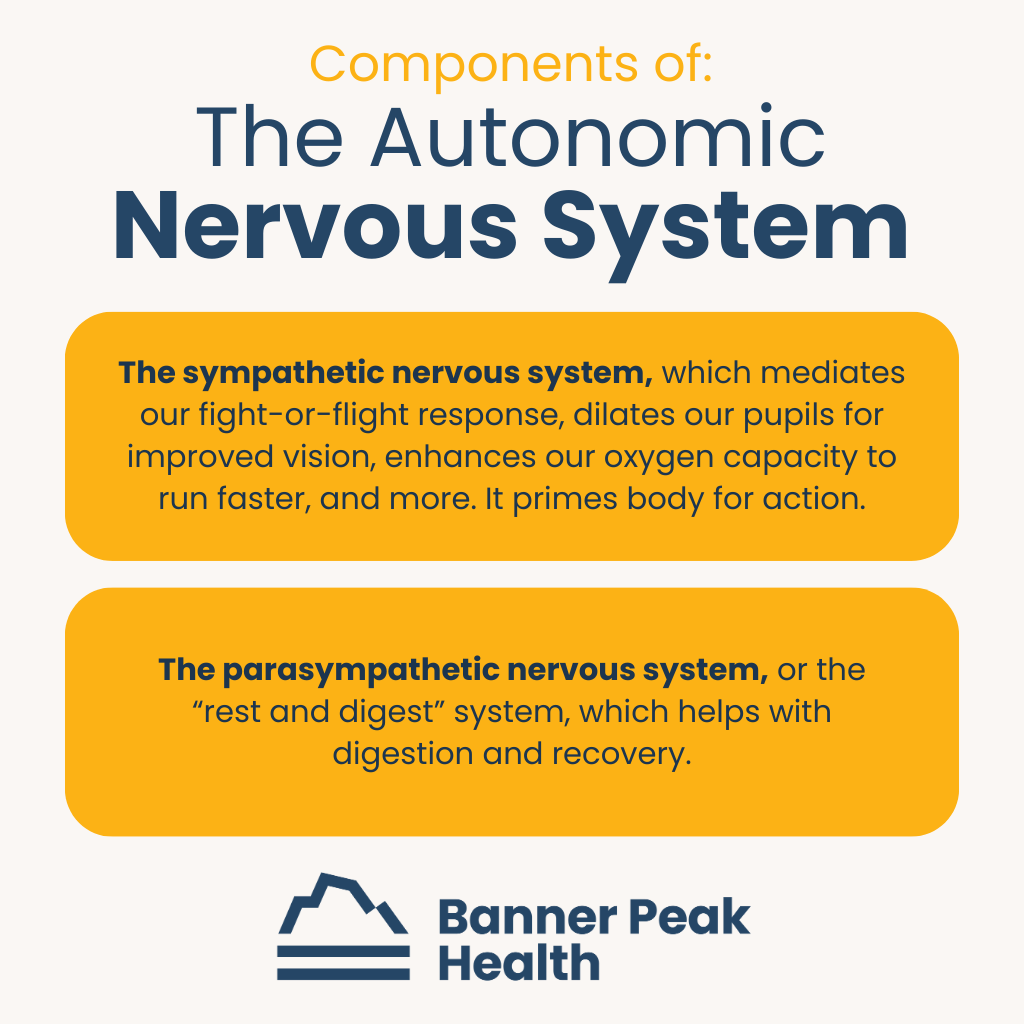
Our autonomic nervous system controls all our essential, automatic biological functions. It comprises two almost opposing systems:
- The sympathetic nervous system, which mediates our fight-or-flight response, dilates our pupils for improved vision, enhances our oxygen capacity to run faster, and more. It primes body for action.
- The parasympathetic nervous system, or the “rest and digest” system, which helps with digestion and recovery.
Knowing where we are on the spectrum between the two competing forces of our autonomic nervous system is vital to our health. The key to understanding that balance is heart rate variability.
What Is Heart Rate Variability?
Normally, our heart beats at a regular rate. If you have a heart rate of 60 beats per minute (bpm), you’ll experience 60 beats in one minute, by definition.
However, the spacing between those heartbeats isn’t precisely one second. The competing forces of the sympathetic and parasympathetic nervous systems mediate the timing of every heartbeat we have.
There are variations in the timing between each heartbeat. By measuring this intra-beat difference, we can analyze a concept called heart rate variability.
When there’s more variation in the spacing between heartbeats, the phenomenon reflects signaling from the parasympathetic nervous system. Conversely, less variation in the spacing between heartbeats reflects a predominance of the sympathetic nervous system.
Analogous to the dashboard of the Tesla, by measuring HRV, we get an insight into our body’s current state.
Are we in a predominantly sympathetic situation (accelerating onto the freeway)? Or, are we in a parasympathetic situation (recharging our batteries and recovering)?
Why Measure HRV?
Heart rate variability first became popularized in the athletic community. As discussed in previous blog posts, physical training is a process of:
- Initiating stress in our body
- Recovering from that stress to come back stronger
- Coming to a new equilibrium of greater strength or aerobic capacity
Athletes trying to maximize their athletic performance want to know how much stress they can put their system under. How much recovery will they need? So, the HRV is uniquely suited to tell athletes whether they can tolerate more strain or need to recover.
For example, a weightlifter who just finished a big workout would need to check their HRV the next day. If the HRV went down, that would reflect a sympathetic predominance, meaning the body hadn’t recovered enough and they may need to modify their workout.
Conversely, if the weightlifter’s HRV were rising, it would indicate a parasympathetic predominance, meaning the body was successfully recovering and could tolerate a more intense workout.
The Role of Stress
In previous posts, we’ve explored the deleterious effects of excess stress. We’ve discussed how stress can cause stress belly and many other bad outcomes, including obesity, high blood pressure, diabetes, cancer, stroke, and heart attack.
The same gauge athletes use to determine whether they’re under stress or in stress recovery can also measure how much stress non-athletes are under.
Stress can be physiological, in terms of a tough workout, or psychological. Increased sympathetic tone and decreased HRV indicates higher stress levels.
We know how damaging stress can be, but it’s been challenging to quantify. Fortunately, we now have tools that accurately measure a body’s total burden of stress.
Enter: Garmin and other wearables that measure heart function.
How Does Garmin Measure Stress?
So, how does Garmin measure stress?
For the last 120 years, we’ve measured heart rate using electrical signals.
The first apparatus weighed over 600 lbs and required five people to operate. Today, a wearable heart rate monitor, like Garmin or an Apple Watch, connects to a smartphone app to detect and record data, including heart rate variability.
The newest development in iPhone watches and other wearables is an optic sensor mechanism that shines an LED light into the superficial skin. The sensor monitors the light reflected back to determine the pulse-by-pulse change in the shape of a tiny artery beneath the skin.
This technology has gotten remarkably accurate. As a result, we’re entering an era of readily-measurable HRV. Anyone who wears a Garmin, an Apple Watch, or another wearable that tracks heart function can potentially use it in this way.
As we explained above, HRV is an accurate way to quantify and measure stress.
Researchers have been studying HRV as it applies to various disease states. Just as stress is a risk factor for bad outcomes, so too is diminished heart rate variability. These outcomes include cardiovascular disease, cancer, diabetes, and inflammatory conditions.
How to Improve Your Heart Rate Variability
Wearables like Garmin and the Apple Watch could provide incredible new data for scientists to study and gain insights. By increasing sample sizes from a few participants in a laboratory to potentially hundreds of thousands of 24/7 users, the potential for vast amounts of data is staggering.
While we don’t have all the answers yet, we do know some basic ways you can improve your HRV (and your health in general).
- Get proper rest — ensure you get enough quality sleep.
- Reduce alcohol intake — studies show alcohol consumption diminishes your HRV.
- Maintain consistent eating and sleeping times — stay within your circadian rhythms.
- Meditate and practice deep breathing exercises — these can help with parasympathetic tone.
- Exercise — helps improve sympathetic tone.
What’s Next?
We began this post with the question, “How does Garmin measure stress?” We’ve answered that — Garmin and other wearables that measure heart function measure stress by detecting your heart rate variability (HRV).
We’ve also explained why measuring and monitoring your stress and HRV is important — both can affect your overall health and wellness.
You can take the first steps toward improving your HRV by following the tips listed above. If you want to further explore your heart rate variability and other important health indicators, that’s our specialty at Banner Peak Health.
We create personalized care plans for each of our members and focus on what’s important to you. Contact us today if you’re interested in our services.
Why ‘Outlive’ by Peter Attia Is One of the Best Books I’ve Ever Read
“Outlive: The Science and Art of Longevity” by Peter Attia is one of the best medical books I’ve ever read. I’m not alone in that assertion — Steven D. Levitt, New York Times bestselling author of “Freakonomics,” called it “One of the most important books you’ll ever read.”
“Outlive” is structured like most books in the self-help genre. Dr. Attia recounts his autobiographical journey, then entices the reader to follow him on the path he’s described.
His eclectic background informs his creative thought process and brings a different perspective to the medical challenges of prolonging life.
As a young man, Attia planned to become a professional boxer. Plans changed, and he earned undergraduate degrees in mathematics and engineering. From there, he studied medicine at Stanford and earned an M.D.
At the beginning of his career as a physician, he studied at Johns Hopkins Hospital in general surgery and at the National Institutes of Health as a surgical oncology fellow.
Today, he focuses on longevity and healthspan (the number of healthy, fully functioning years we have). What I appreciate most are the intellectual constructs he brings to the field.
He’s put a new spin on prevention, explaining that you’ll enhance your longevity by preventing things that cut your life short. A vital part of that is primary care internal medicine.
Why This Topic Strikes a Chord
In today’s post-pandemic society, we have an opportunity to shift the way we approach our health from defensive to offensive. Rather than merely reacting to a health issue, we can work proactively to prevent that health issue from happening in the first place. That appeals to many people, myself included.
The pandemic changed the world in many ways, but one potentially positive outcome is that people are much more cognizant of their health and wellness. That awareness means people realize the value of preventative methods.
Case in point: Dr. Attia’s book is a number one New York Times Best Seller and has nearly 3,000 5-star reviews on Amazon.
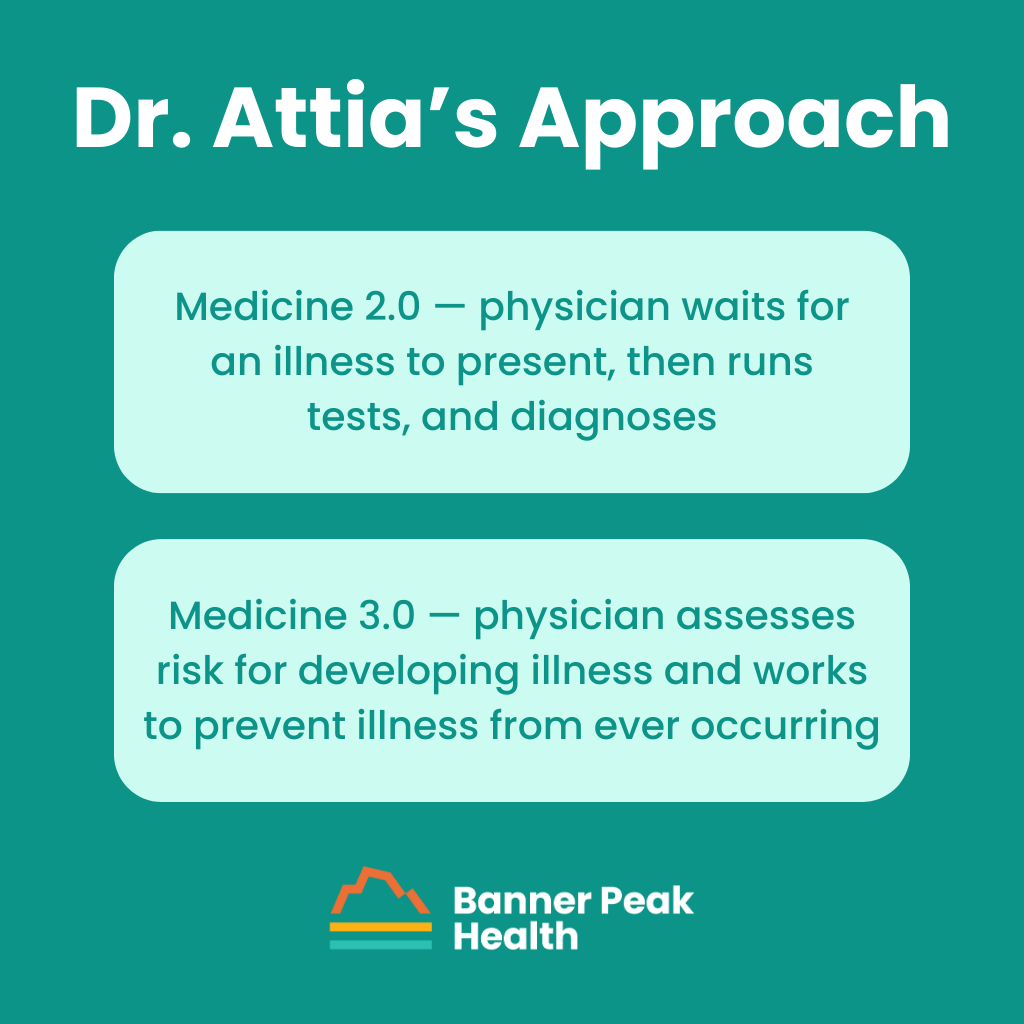
Dr. Attia’s Approach
Dr. Attia calls his approach Medicine 3.0 and refers to traditional medicine as Medicine 2.0. Here are the basic differences:
- Medicine 2.0 — physician waits for an illness to present, then runs tests, and diagnoses
- Medicine 3.0 — physician assesses risk for developing illness and works to prevent illness from ever occurring
The problem with Medicine 2.0 is the inherent limitations within the research. Traditionally, research takes decades of study and carefully controlled experimentation.
However, we can’t test humans the same way we test lab rats, especially when our goal is prevention rather than treatment. Who would commit to experimental lifestyle changes for decades for the sake of science?
Therefore, we can’t rely on the traditional methodology (clinically controlled trials) used by Medicine 2.0 to guide us in pursuing our goals in Medicine 3.0. We need to form a new body of scientific evidence using an alternative to randomized controlled studies.
Focus on Fundamentals
What I find most appealing about Dr. Attia’s approach to longevity is his focus on the fundamentals. The study of aging and longevity has yielded tremendous insights into the physiology of how our cells age.
Many people tout hypothetical pharmacological interventions as solutions to help us prolong our health and lifespan. However, I strongly agree with Dr. Attia that lifestyle modifications are the strongest and safest modalities.
He then introduces what he calls the Four Horsemen — the four leading causes of death and disability in Western society. They are:
The remainder of his book details therapeutic modalities, for which there is the best evidence for avoiding or staving off these Four Horsemen. The fundamentals he describes are what we’ve always referred to as lifestyle medicine.
He emphasizes:
Only then does Dr. Attia mention what he calls exogeneous molecules, or pharmacological treatments, which play a refreshingly small role in his extensive book.
The Banner Peak Health Connection
At Banner Peak Health, we always look for new diagnostic and therapeutic techniques to provide our patients with more personalized care. If you share that commitment, I highly recommend reading “Outlive” by Peter Attia, M.D. It’s quite a deep dive, but it’s well worth it.
What Dr. Attia brings to the practice of health at Banner Peak Health is a cognitive framework that validates much of what we’ve already been doing.
He also inspires new ways of thinking about the challenge of maintaining lifespan and healthspan as part of a longevity program. We plan to incorporate those insights into our practice.
Why Stress May Be Your Worst Enemy
Psychology becomes biology. When we think of emotions, we tend to think only of feelings and mental reactions. But as I’ve discussed before, the mind and the body are inextricably linked.
This linkage occurs via hormones, the substances produced by one cell that influence the biology of another. Hormones are how the body’s systems communicate.
For example, the adrenal glands produce adrenaline and cortisol in response to an accelerated heart rate, which can result from both biological stress and emotional stress. The selfsame hormones triggered by injury and lack of oxygen are also triggered by fear, worry, and anger.
Stress Is Here to Stay
Our stress response is adaptive. Our ancestors’ stress response (adrenaline release → increased heart rate → increased oxygen consumption → increased blood flow to muscles) helped them avoid predators in fight-or-flight scenarios. It’s how we as a species have persevered.
In modern society, stress is more chronic. It’s unlikely we’ll need to run from a tiger for a few short minutes (a temporary biological trigger), but we do spend the entire month worrying about paying our mortgage (a long-term emotional trigger).
We live in an epidemic of heart disease, cancer, and obesity. We can connect them all to the constant, dangerous levels of stress we endure daily. Unmanaged, this stress can trigger cascades of biological responses that result in detrimental outcomes.
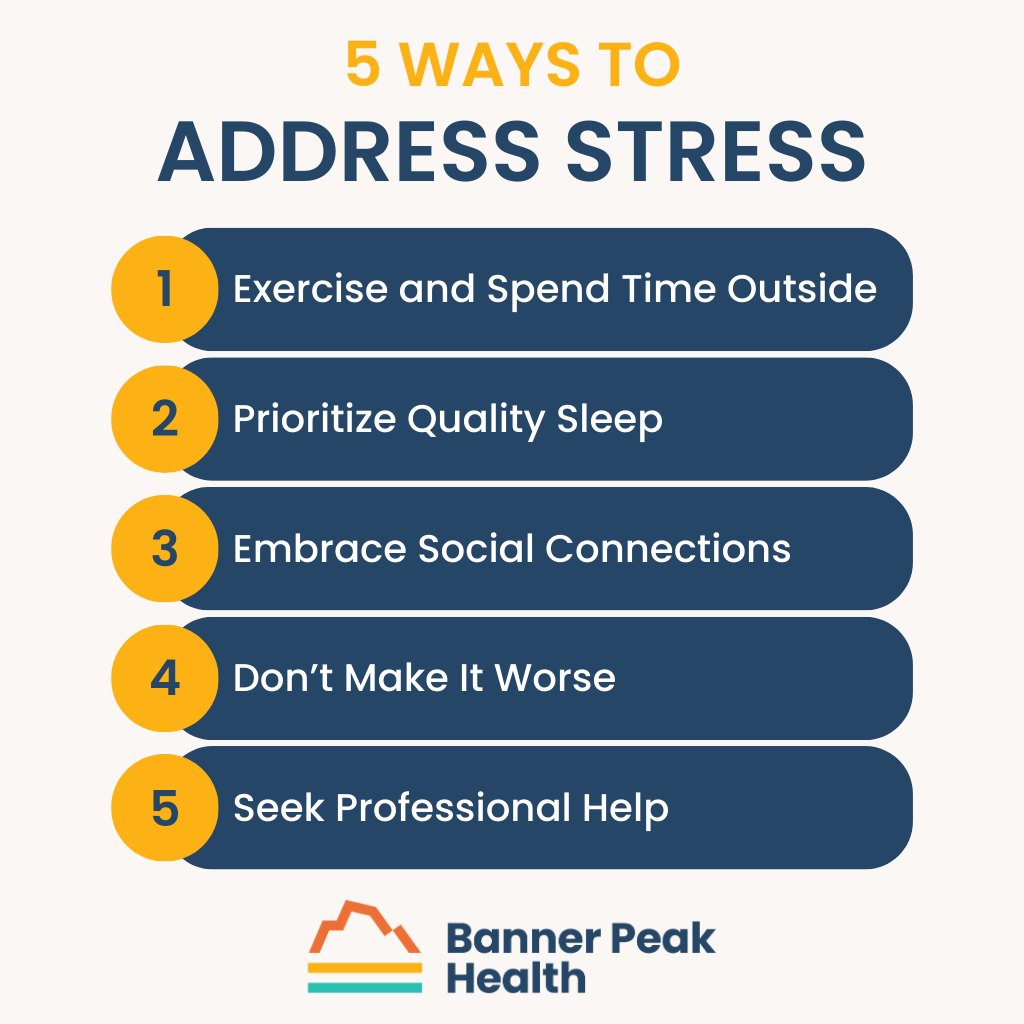
5 Ways to Address Stress
Unfortunately, external sources of stress — illness or the loss of a loved one, for instance — are often beyond our control. In these cases, we need to understand and address our internal response to stress because it’s our only controllable factor.
Most of us are aware of our stress inbox — the external factors that generate our stress — but haven’t considered our stress outbox — our internal stress response. How do we process and mitigate stress?
Everyone is different, but these tools can be helpful for most people.
Exercise and Spend Time Outside
Exercise is a powerful means of stress reduction. Beyond that, you can also spend time in nature. Regardless of what you’re doing, simply being outside and seeing greenery helps relieve stress.
Prioritize Quality Sleep
We’ve previously discussed sleep and its importance for maintaining good health. Here, we’ll just underscore how poor sleep and chronic stress become a vicious cycle. Stress inhibits sleep, which compounds the stress response, which makes you prone to poor sleep, and so on.
It’s crucial to get sleep no matter what, but we realize this is easier said than done. Ask your doctor for help, and make sure your coping mechanisms don’t hinder quality sleep.
Embrace Social Connections
We humans are social creatures. We’ve survived as a species not just because of our own individual adaptations, but because of what we’ve done collectively.
Don’t ignore that evolutionary tendency. Seek religious and/or secular communities of like-minded people who will support and encourage you. “Going it alone” is not an appropriate stress response and will likely lead to increased stress levels.
Don’t Make It Worse
Avoid substances such as nicotine and alcohol. These potent chemicals make us more prone to stress and work against our ability to manage stress in a healthy way.
Seek Professional Help
You’re not alone in this struggle. Stress is a global epidemic affecting millions of people, and there are amazing therapists, counselors, and coaches available to help.
However, these professionals may have long waiting lists, or may not be available in your immediate area. If you lack the wherewithal to seek or secure professional help, consult your primary care physician.
The Banner Peak Health Difference
Here at Banner Peak Health, we’re thankful our patients see us as more than “just” their physical doctors. That’s certainly not how we see ourselves!
We recognize and appreciate the mind-body connection and regularly help our members with mental health concerns. If you need assistance pursuing a less stressful, more fulfilling life, we’re here to help.