How to Get More REM Sleep: Proven Strategies for Quality Rest
Adequate sleep maintains optimal health in both body and mind.
 Sleep helps your body:
Sleep helps your body:
- Maintain peak physical performance
- Maintain immune function
- Repair injuries
- Control weight
Sleep helps your mind:
Let’s explore REM, why it’s important, and how to get more REM sleep.
What Is REM Sleep and Why Is It Important?
Your sleep architecture is divided into 90-minute cycles. Each cycle includes stages of lighter sleep, deeper sleep, brief periods of wakefulness, and REM sleep.
REM stands for “rapid eye movement” because, during this stage of sleep, our eyes move rapidly under our eyelids. Brain waves during this stage are the same as when we’re awake, but we cannot use our muscles, so we can’t move. During this sleep stage, we dream, and the inability to move our muscles prevents us from acting out our dreams.
During this crucial stage, our brains consolidate our memories, and we attach emotional impact to them.
How to Get More REM Sleep With Better Sleep Habits
The sleep cycles that repeat every night are influenced by other bodily functions (some related to hormone release) that occur earlier in the day. How these cycles are timed determines how well we achieve REM sleep that night.
You can improve and increase your REM sleep with some simple changes in your sleep habits.
Many people have heard advice about light exposure, including avoiding blue light before bed, but there’s much more to “light theory” and circadian rhythms. Research demonstrates that the best light exposure to optimize your circadian rhythm is “first morning light” or “dawn light.” It’s one of the most potent signals we have to set (or reset) our circadian rhythms. Sleeping well at night begins with good light exposure first thing in the morning.
I’ve also discussed the TUO Life Bulb, which you can use at home to obtain good morning light exposure.
Another crucial step is to avoid the alarm clock whenever possible. Waking up to an alarm clock isn’t a pleasant way to start your day. Also, the last 90-minute sleep cycle of the night contains the most REM sleep. An alarm clock interrupts your natural sleep cycle at possibly the worst time — at the end, robbing you of valuable REM sleep.
Alarm clocks are REM killers, but they aren’t the only ones. Anything that hurts your sleep hurts your REM sleep. For example, obstructive sleep apnea is one of the biggest sleep impairers we help our members tackle, but we have a not-so-secret weapon.
How Banner Peak Health Can Help You Get More REM Sleep
We’re excited to work with a new sleep image device that allows you to screen for obstructive sleep apnea by wearing a small rubber ring that transmits a signal to your smartphone.
Through advanced technology and other lifestyle changes, we enjoy helping our members figure out how to get more REM sleep and feel refreshed daily.
How to Get More REM Sleep by Changing Lifestyle Factors
Any factor that enhances your sleep quality also enhances your REM sleep.
My best advice regarding how to get more REM sleep is:
- Be cognizant of the chemicals you ingest (e.g., alcohol, caffeine) and their effect on your body. Some patients are more sensitive than others.
- Use stress-reduction techniques like meditation.
- Follow the suggestions in this blog post.
- Get adequate exercise.
If you need more help or have additional questions, reach out. We’re happy to talk.
Sleep is medicine. It affects every aspect of your health. Getting adequate sleep is one of the best things you can do for your body. Don’t underestimate its value.
How to Find a Great Concierge Doctor Near Me
Finding a doctor can be challenging, especially when exploring concierge medicine for the first time.
This blog post will explain the ins and outs of concierge medicine, how to search for a “concierge doctor near me,” and why Banner Peak Health stands out.
What Is Concierge Medicine?
Merriam-Webster defines concierge medicine as a healthcare practice of primary care physicians in which patients pay a membership fee for enhanced access and services.
We at Banner Peak Health define concierge medicine as a relationship-focused healthcare model.
Because the concierge model affords us more time with each patient, we get to know each patient’s personality more deeply than physicians in a traditional practice can. We also leverage that time to explore each patient’s symptoms intellectually, coordinate with other doctors involved in their care, and educate the patient about medical terminology.
Time is the ingredient that takes you from stellar internal medicine to stellar concierge medicine.
The Differences Between Concierge Medicine and Conventional Medicine
I often use the saying “He who pays the piper picks the tune” to explain concierge medicine to anyone unfamiliar.
The financial structure of medicine affects the care patients receive. In a traditional fee-for-service model, the insurance company funds the care and is the de facto boss. However, in a concierge model, the patient funds the care — so they’re the boss.
At Banner Peak Health, we’re beholden to our members’ needs rather than those of insurance companies. That distinction explains our priorities, who we seek to impress, and what care we provide.
You’re entitled to a doctor who’s enthusiastic about medical care and about providing care for you. Concierge medicine circumvents physician burnout by design, so your physician is always engaged.
 At Banner Peak Health, our mantra is “happy staff = happy patients = better health outcomes for all (patients and doctors).” We’re proud to offer extensive benefits to our members, including:
At Banner Peak Health, our mantra is “happy staff = happy patients = better health outcomes for all (patients and doctors).” We’re proud to offer extensive benefits to our members, including:
- Access to your private physician’s personal phone
- Little to no wait times
- Same-day or next-day appointments
- Telemedicine visits and consults
- Extended appointments
- Individual follow-ups by your health team
- Prompt care for urgent needs
- Coordination with specialists and hospitals
- Strong focus on preventative medicine and screenings
And much more.
What Should I Look For in a Concierge Doctor Near Me?
When you search “concierge doctor near me,” a list of practices appears. Which one do you contact? How do you identify the best fit for you? We can help.
First, you want a doctor who will be excited to be your doctor — someone enthusiastic about being a physician, providing care, explaining terminology, researching, and listening to you.
You want someone who accepts you as you are but will also hold you accountable as you pursue your health goals. Your health journey has no escalators. You have to reach the highest peaks yourself.
At Banner Peak Health, we interview prospective patients. We want patients who want to be active participants in their healthcare. We don’t have an “autopilot” option. We want to guide people who want to work to reach their health goals.
You also want a practice with a small physician-patient ratio. This way, your physician can spend ample time developing a relationship with you.
At Banner Peak Health, we see about 250 or fewer patients per physician. Typical concierge practices average between 400 and 600 patients per doctor, and traditional practices average thousands.
Is It Important to Find a Concierge Doctor Near Me?
It’s important to consider your proximity to your concierge doctor, but it’s not a reason to dismiss an otherwise good-fit physician. Remote technology has allowed physicians and patients to meet regularly to discuss non-urgent concerns.
However, there may be times when you need an in-person visit or an urgent appointment. In those cases, having a concierge doctor near you is advantageous.
We’re located in Walnut Creek, and we serve patients in the following communities:
- Walnut Creek
- Berkeley
- Oakland
- Piedmont
- Orinda
- Lafayette
- Moraga
- Pleasant Hill
- Danville
- San Ramon
- Walnut Creek
- Concord
- Clayton
- San Francisco
And beyond.
Partnering With Banner Peak Health
We’re honored that our patients trust us, and we take that trust seriously. We also practice the Golden Rule — we provide the care we would expect ourselves or would want for our family members. When you become a member at Banner Peak Health, that’s what you can expect.
If you’re searching for a “concierge doctor near me” and think we’d be a good fit, contact us. We’re happy to answer your questions.
A Physician’s Thoughts on the Oura Ring: The Latest Health Trend
Gwyneth Paltrow. Jennifer Aniston. Prince Harry. Will Smith. Shaquille O’Neal. Mark Zuckerberg. Barry Rotman.
What do these people have in common? They’ve all publicly acknowledged wearing an Oura Ring — the new medical sensation.
Oura Health was founded in 2013 in Finland. Its product, the Oura Ring, was made commercially available as a sleep-tracking device in 2016. It began with Kickstarter funding in 2015 and expanded to a market capitalization of $2.55 billion by 2022.
The Oura Ring’s original goal — sleep tracking — has expanded to include many goals, including stress management, early disease detection, menstrual cycle tracking, and more.
In the growing field of consumer wearable health devices, the Oura Ring stands out as the most powerful. However, not all its functions are well-validated.
In this blog post, I’ll explore the hype surrounding the Oura Ring. What is it? How does it work? Which features are valuable, and which aren’t?
What Is an Oura Ring?
An Oura Ring is a five-gram, titanium-encased device designed to be worn on a finger. It communicates data to a smartphone app.
Despite its small size, it continuously measures:
- Motion
- Peripheral skin temperature
- Heart rate
- Heart rate variability
- Blood oxygen saturation
Two decades into the smartphone revolution, we’ve become accustomed to an astounding array of functions built into a small device. However, when I started medical school nearly forty years ago, a device like the Oura Ring was nothing but science fiction.
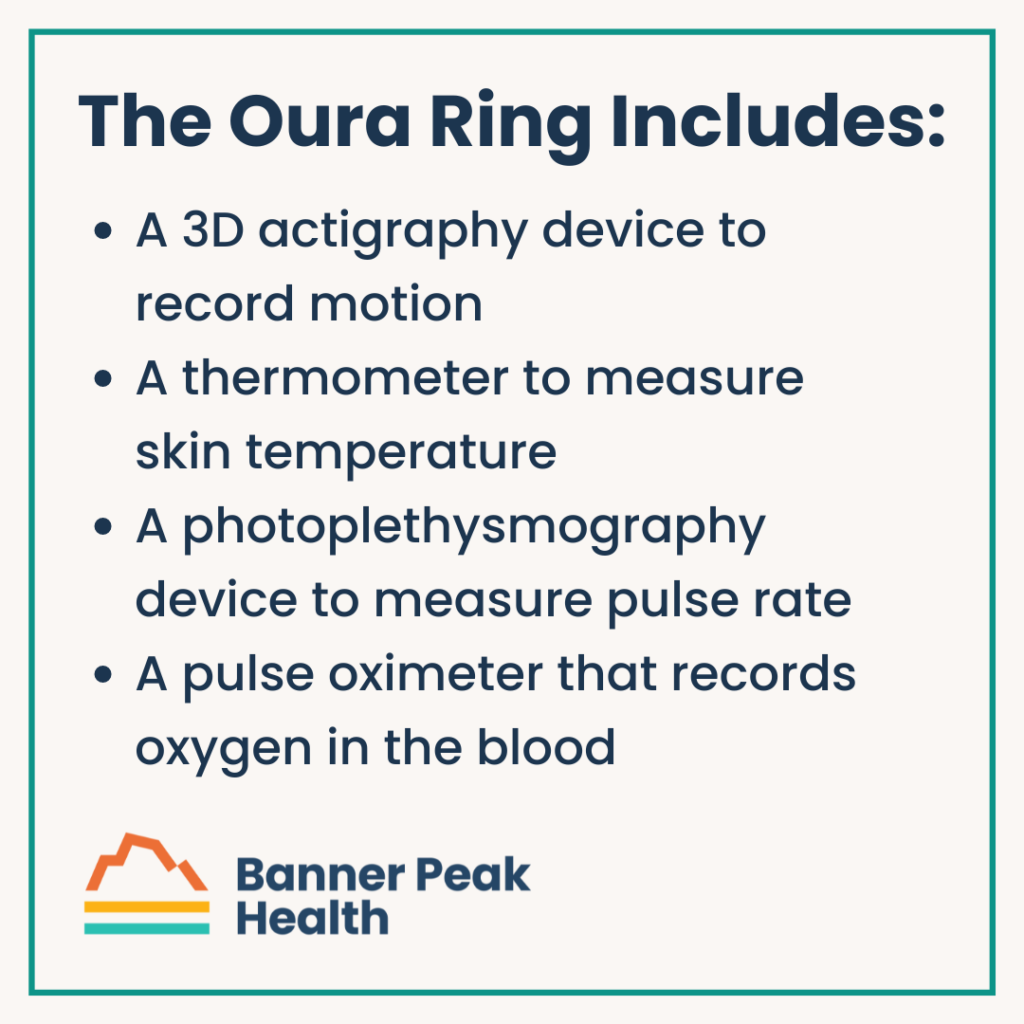
The Oura Ring includes:
- A 3D actigraphy device to record motion
- A thermometer to measure skin temperature
- A photoplethysmography device to measure pulse rate
- A pulse oximeter that records oxygen in the blood
In addition to direct sensor data, the smartphone app calculates various physiological parameters using user data (gender, age, height, and weight).
Some complex algorithms use large, international population-based measurements and AI analysis. For example, the Oura Ring’s sleep metrics are industry-leading. The ability to differentiate sleep stages (awake, light, deep, and REM) is about 80% accurate compared to overnight sleep studies.
For most applications, the Oura Ring combines four possible data sources:
- Daily measured data
- Individual data baseline
- User-specific data
- Population-based comparison metrics
For example, to detect the early onset of an infection, the Oura Ring notes a change in a person’s skin temperature, heart rate, breathing rate, and heart rate variability from his or her baseline. It compares that change to a predictive population-based model.
One study noted the Oura Ring’s ability to diagnose COVID infection an average of 2.75 days before the study subjects displayed enough symptoms to seek a COVID test.
On the other hand, building a function that incorporates many layers of data means that an inaccuracy at any point compromises the entire process’s accuracy.
For example, Oura Ring has a readiness function that combines your sleep, activity, and stress scores to reflect how prepared your body is for the day. The sleep score has good validation. However, both the literature and my experience suggest that the activity score isn’t accurate and that the magnitude of error increases as the intensity of exercise increases.
The more active you are, the more difficult it becomes for the Oura Ring to measure your heart rate and track the total amount of body motion. A similar challenge affects the stress score, which measures your sympathetic nervous system at rest. Physical activity normally increases sympathetic tone.
I’ve found that the Oura Ring doesn’t differentiate when I am truly at rest compared to a brief break in moving around, compromising the stress score’s accuracy. Therefore, I don’t trust the overall readiness score’s accuracy.
The Oura Ring continues to release new functions, such as menstrual cycle tracking, which appears to be at least as accurate as tracking daily oral temperature.
How Accurate Is an Oura Ring?
The Oura Ring provides exciting ways to learn about your body’s health status in real time. I’ve grouped many of the features into three categories depending on their current quality of clinical validation:
- Accurate and valuable tool
- Possibly accurate, use cautiously
- Unproven, for entertainment purposes only

If using one of the functions motivates you to focus on a health aspect and improve your lifestyle choices, the feature is beneficial regardless of its proven accuracy level.
Does an Oura Ring Have Side Effects?
More knowledge isn’t always better.
Consumer wearables’ rising popularity has led to a new diagnosis: “orthosomnia,” an unhealthy obsession with achieving perfect sleep. Paradoxically, becoming overly focused on your quality of sleep leads to anxiety and frustration, which reduces your ability to sleep well. Knowing your sleep score upon arising can hurt your mood for the day.
Can an Oura Ring Help You Make Healthier Decisions?
I found the Oura Ring extremely helpful in my quest to become more “chill.”
I used it for several Metric-Driven Empowerment Cycles (MDECs), tracking sleep, HRV, and meditation. The measured outcome variable allowed me to make a series of adjustments to my life and observe the results. I followed only a few of the growing list of measurements my Oura Ring provided.
Depending on your interests, there are many compelling uses:
- Activity level
- Step count
- Active energy expenditure
- Total energy expenditure
- Body temperature
- Respiration rate
- Heart rate
- Heart rate variability
- Total sleep time
- Sleep stage time (awake, light, deep, and REM)
- Composite readiness score
- Composite stress score
- Composite resilience score
- Early infection detection
- Early pregnancy detection
- Menstrual cycle tracking
The list of functions continues to grow, as does the number of studies validating them.
Final Thoughts on the Oura Ring
There’s a wide array of consumer wearable health devices available. The Oura Ring is the best and will become the recommended device for Banner Peak Health’s patients.
The Oura Ring includes superb directions and educational materials. However, it becomes even more valuable when incorporated into an overall health plan.
Please let us know if you have an Oura Ring or are considering purchasing one. We want to help you derive the maximum health benefit from it.

Heart Rate Variability: A New Tool for Stress Management

Sometimes, you don’t realize you’re stuck in a rut until your life improves.
Life’s impediments can develop slowly, imperceptibly weighing you down. Your daily experience may be suboptimal, but since you’ve felt that way for many years, you feel normal. Only in retrospect do you realize, Wow! That wasn’t my best self. I can feel so much better!
Many sophisticated tests can measure health status. How about a very simple one — the ability to wake up feeling great?
This blog will review my four-month quest to reach that goal and how I used heart rate variability (HRV) to do it.
How Stress and Heart Rate Variability Relate
I write a lot about stress and its health impacts.
For a risk factor as potent as stress, it’s surprising that we’ve lacked practical methods of measuring it until recently. The growing popularity of wearable devices has finally given us convenient access to this vital metric.
I’ve written about how heart rate variability (HRV) reflects the balance between our sympathetic and parasympathetic nervous systems. More stress increases the sympathetic tone, reducing the variability in timing between each heartbeat. Less stress allows for a greater parasympathetic tone, increasing the timing variability between each heartbeat.
Basically, the higher your heart rate variability, the more “chill” you are.
Recent blogs have illustrated the value of MDECs (Metric-Derived Empowerment Cycles), techniques for generating actionable health data to help people improve their health. Heart rate variability, as measured by wearable devices, is a helpful metric-derived empowerment cycle.
Heart rate variability reflects the sum of physiological and psychological stress sources. Worried about a final exam? Bad night of sleep? Too much (or any) alcohol? Hard workout? Sore back? Laid off from a job? Your heart rate variability will reflect it.
Technically, heart rate variability doesn’t measure the total amount of stress we are exposed to. Rather, it measures how our body reacts to stress — a subtle but important distinction.
Stress is an inevitable part of the human condition. In manageable amounts, it propels us forward, but if its intensity and duration exceed our ability to cope, we suffer adverse consequences. Heart rate variability as a metric-derived empowerment cycle quantifies how our body reacts to our total stress burden. It can also track the results of our stress-management efforts.
Heart Rate Variability’s Role in Fitness
The current abundance of products that measure heart rate variability (Apple Watch, Garmin, Whoop, Oura Ring, etc.) reflects heart rate variability’s popularity in the fitness community. Analyzing daily heart rate variability provides a valuable tool to assist athletes in monitoring their response to training.
A hard workout doesn’t make you stronger, per se; rather, a successful recovery makes you stronger. Knowing your heart rate variability can help you adjust your workouts’ intensity and timing.
For instance, an athlete who wakes up feeling “off” and notices an unusually low heart rate variability score might be better served by scaling back or eliminating a hard workout that day rather than risk overtraining and slowing overall improvement.
While using heart rate variability for sports training may be the primary use case driving its popularity, measuring variation over longer periods of time can guide decisions that affect a wider range of health outcomes.
Short-term stress is adaptive. It helped our ancestors outrun predators. It’s the chronic, elevated stress of modern life that raises our risk for obesity, heart disease, diabetes, cancer, sleep disorders, and mental health conditions. Heart rate variability informs how a person can better cope with stress and reduce the risk of these types of illnesses.
My Stress-Reduction Journey
Over the last year, I’ve experimented with different methods for measuring heart rate variability, including wearables such as Whoop or the Oura Ring and smartphone apps that use a chest strap or the phone camera. How heart rate variability is measured affects its utility.
Heart rate variability varies every second of the day and night in response to variables such as emotional state, exercise, medications, diet, and sleep. For heart rate variability to assess individual variables such as less sugar intake or more exercise, other factors need to be standardized.
A common approach is to measure heart rate variability while asleep, which reduces factors that might interfere with the result. For example, Whoop uses a proprietary algorithm to average the response throughout the night, preferentially calculating heart rate variability during slow-wave sleep, and the Oura Ring records the heart rate variability level every five minutes and presents an average for the night.
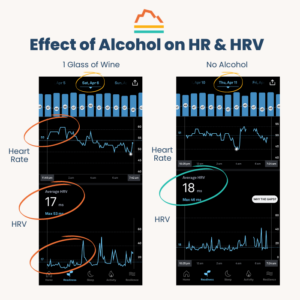
I use the Oura Ring because I appreciate its straightforwardness, and I like tracking my heart rate variability throughout the night. My Oura Ring has taught me that chocolate, sugary desserts, and alcoholic beverages impair my sleep and lower my heart rate variability when I consume them close to bedtime. In fact, I can correlate how many hours the effect lasts with how much I consume.1
In general, measuring heart rate variability at night eliminates many influences that occur while we’re awake. However, issues that arise at night, like a sleep disorder, can affect it. As I described in a prior blog, a SleepImage device taught me that I had a mild case of obstructive sleep apnea, which contributed to my reduced heart rate variability.
I also use the app HRV4Training to monitor my heart rate variability daily. Its protocol relies on a one-minute pulse reading through the smartphone camera, done while sitting immediately after waking up. It eliminates the effects of sleep disorders and other factors that come into play once you begin your day.
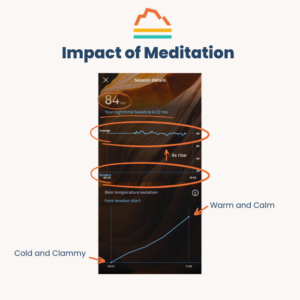
The Oura Ring has a great feature labeled “unguided session” that monitors your heart rate variability for a predetermined amount of time, allowing you to run experiments and determine their effect on your heart rate variability. I use it to track my physiological response to my 20-minute meditation sessions. My heart rate variability rises two or four times higher than my nighttime values (even after treating my obstructive sleep apnea), confirming my meditation’s efficacy.2
In addition to providing daily feedback, heart rate variability monitoring tracks changes over weeks and months.
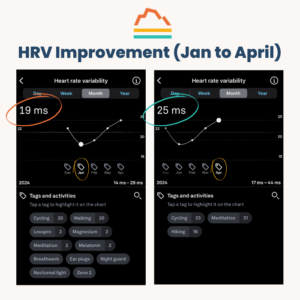
In January 2024, I began addressing many years of deferred maintenance in my life. I embarked on an extensive process of physician appointments, lab studies, sleep monitoring, diet modification, therapy, and dietary supplements.
Many of these interventions would be expected to raise my heart rate variability:
- I began taking a fish oil supplement to reduce my cardiovascular risk. Fish oil has been found to have anti-depressant benefits. I hadn’t been suffering from depression, but any mood improvement may raise heart rate variability.
- I included more Zone 2 training in my exercise regime.
- I improved my sleep/wake cycle synchronization using a TUO lightbulb. I now get more sleep and don’t need an alarm.
- I began treating my mild obstructive sleep apnea.
- I reduced my alcohol and sugar consumption.
- I began B12 replacement for borderline low levels.
- I reshaped my work responsibilities as a physician.
- I began adhering more consistently to 20-minute meditation sessions each morning.
- I adopted a “no news after nine” rule to reduce my news consumption.
My monthly average heart rate variability rose a remarkable 25%, from 19 ms in January 2024 to 25 ms in April 2024. This very significant improvement correlates with how much better I feel.
Heart Rate Variability: Final Thoughts
This blog is not a precise prescription for how to feel better. Rather, it’s an example of how HRV monitoring can guide decisions to improve one’s life. For the first time in years, I wake up feeling great.
I want to bring heart rate variability monitoring’s benefits to patients at Banner Peak Health. Reach out to learn how it can help you achieve your health goals.
Footnotes:
- Before my April 6 nocturnal Oura Ring recording, I consumed one glass of wine with dinner. Both my heart rate and heart rate variability were elevated until around 3 a.m., reflecting the increased sympathetic tone associated with processing even a small amount of alcohol. Most nights, I drink no alcohol. For example, the April 11 tracing illustrates a comparably low HRV score from other factors distributed more evenly throughout the night.
 My Oura Ring functions as a biofeedback mechanism, demonstrating my meditation’s physiological impact. This is a tracing of an abbreviated 10-minute meditation session. The average heart rate variability of 84 ms reflects a value fourfold higher than my average nocturnal value for the year. Compared to being asleep, I reach a state four times more chill during meditation, quantitative evidence of its powerful impact!Peripheral skin temperature correlates with heart rate variability. This tracing demonstrates meditation’s impact on peripheral skin temperature, which progressively warms during the session. When we’re nervous (increased sympathetic tone), our hands become cold and clammy. As we calm down, they warm up, reflecting an increased parasympathetic tone. My finger became warmer during the meditation session.
My Oura Ring functions as a biofeedback mechanism, demonstrating my meditation’s physiological impact. This is a tracing of an abbreviated 10-minute meditation session. The average heart rate variability of 84 ms reflects a value fourfold higher than my average nocturnal value for the year. Compared to being asleep, I reach a state four times more chill during meditation, quantitative evidence of its powerful impact!Peripheral skin temperature correlates with heart rate variability. This tracing demonstrates meditation’s impact on peripheral skin temperature, which progressively warms during the session. When we’re nervous (increased sympathetic tone), our hands become cold and clammy. As we calm down, they warm up, reflecting an increased parasympathetic tone. My finger became warmer during the meditation session.
The Benefits of Continuous Glucose Monitoring

In earlier blog posts, I’ve discussed the concept of Metric-Derived Empowerment Cycles (MDECs).
Measurement devices now provide actionable data that incentivize and track the results of healthy behaviors. It can be a long journey from thinking about behavior change to initiating change to sustaining it. That’s human nature. We need all the help we can get.
Generating a metric, or “putting a number on it,” can be a very powerful tool to motivate behavioral change by quantitating a baseline and providing a measurable path to improvement. Continuous glucose monitors enable one of the most valuable MDECs we use at Banner Peak Health.
Chronically elevated blood glucose levels are associated with the development of diabetes, which elevates the risk for a wide range of illnesses, including heart disease, stroke, cancer, and kidney disease. The root causes of elevated glucose are multifactorial and include diet, stress, exercise, and sleep. The physiology of blood glucose is very complex.
What Is a Continuous Glucose Monitor?
The ability to measure glucose levels has come a long way since the days when practitioners would taste urine to detect sweetness, indicating excess sugar excretion. (The term diabetes mellitus is derived from Greek diabetes, meaning to pass through, and from Latin mellitus, meaning honey or sweet.)
By the 1840s, tests using chemical reagents could detect sugar in urine. By 1913, blood glucose levels could be measured in a lab. By the 1960s, blood glucose could be semi-quantitatively measured using a chemical test strip reacting with a drop of blood, though the process was cumbersome and not available for home use.
The true revolution in blood glucose monitoring came in the 1980s with the advent of handheld glucometers and reagents on test strips, allowing convenient self-monitoring. There were still significant constraints, however. One-time-use test strips were expensive, and the process of poking and testing was painful and time-consuming. Only the most dedicated of patients could comply with a two- to four-times-a-day testing regimen.
The technology in continuous glucose monitors, such as the current models, the Dexcom G7 and Freestyle Libre, has progressively improved over the last 15 years. The monitors have a very small tube, or cannula, that inserts into the subcutaneous region under the skin. The probe contains enzymes that generate an electrical signal proportional to the concentration of glucose in the interstitial fluid. Strictly speaking, blood glucose is not being measured directly. However, in most circumstances, the interstitial fluid is very close to the blood glucose level, with current models accurate to less than 10% deviation from blood levels.
The sensor remains attached to the skin for 10–14 days, depending on the model, and sends the results to a smartphone for patient viewing and subsequent transmission to a healthcare provider.
Modern Continuous Glucose Monitoring
The cost and complexity of early continuous glucose monitors relegated their use to the most complicated diabetic patients — those requiring insulin therapy and at greater risk for dangerously high and low levels of blood glucose. Today, the devices are also used for less complicated diabetic patients. They still require a prescription, however.
Just this year, Dexcom released a model, Stelo, that will be approved for sale without a prescription. It offers the same accuracy as their prescription model, the G7, but won’t be approved for those requiring insulin treatment.
The less expensive and more widely available Stelo model opens the way for continuous glucose monitoring to move from treatment of diabetes to prevention of diabetes.
Diabetes represents an unfortunate culmination of many years of progressive metabolic dysfunction. This lengthy process presents ample opportunity to modify behavior and prevent the onset of diabetes.
In medicine 2.0 (disease treatment), medications are the dominant treatment modality. In contrast, medicine 3.0 (disease prevention) relies predominantly on lifestyle choices — how you eat, sleep, exercise, and manage stress. Continuous glucose monitors, once relegated to the realm of medicine 2.0, are now poised to realize their full potential as a powerful tool for medicine 3.0!
Who Should Use a Continuous Glucose Monitor?
As part of screening blood tests, you’ve most likely had your fasting blood glucose level and possibly hemoglobin A1c (HgbA1c) measured. A fasting (12 hours without eating) blood glucose level can indicate your risk of diabetes:

Your HgbA1c level reflects your average glucose level over the past three months (see footnote 1) and is expressed as a percentage:

An elevated fasting blood glucose or HgbA1c indicates that you are at increased risk of developing diabetes or that you have diabetes. And these aren’t rare findings. An estimated 40 million adults in the U.S. have diabetes, and close to 100 million have prediabetes.
Several classes of medications can reduce the risk of progressing from prediabetes to diabetes as well as treat existing diabetes. However, the underlying causes of diabetes — insulin resistance, excess caloric intake, reduced exercise, and fat deposition — are best treated by reversing the lifestyle choices that created them in the first place. Medication can provide a backup safety net if lifestyle modifications don’t create enough benefit.
Continuous glucose monitoring offers a vital monitoring tool for anyone with borderline or elevated fasting blood glucose and HgbA1c levels to better understand their body’s unique physiology and guide lifestyle modifications.
How to Use Data From Continuous Glucose Monitoring
People often have an overly simplified understanding of blood glucose, envisioning a straightforward pipeline from the gut to the blood. Sugar goes in one side and comes out the other. The reality is much more complex.
I envision blood glucose as analogous to a beach ball, surrounded by multiple foam pellet guns bombarding the beach ball with shots of varying intensity from different directions. The movement of the beach ball is determined by the net effect of all the pellet guns. Some of these “pellet guns” are:
- Physical activity — Increased muscle cell usage consumes more glucose.
- Stress — Increased hormone levels of adrenaline and cortisol raise glucose.
- Illness — Infections increase adrenaline and cortisol, which raise glucose.
- Sleep deprivation — Lack of sleep increases adrenaline and cortisol, which raise glucose.
- Meal timing — Longer duration between eating reduces glucose levels.
- Medications — Some medications, such as glucocorticoids, can markedly raise glucose; others, such as thiazide diuretics and statins, can subtly raise glucose.
- Food intake — Certain foods raise glucose more rapidly; individual responses to different foods can vary considerably.
By wearing a continuous glucose monitor, you can learn about the unique effect of all these variables and more on your personal glucose levels.
Those using continuous glucose monitors to reverse prediabetes most commonly use them for several months.
The first step involves understanding the magnitude of the problem. Knowing your blood glucose level every five minutes, 24/7, provides a much more nuanced understanding of your metabolism than a one-time fasting level or an average level over 90 days.
The second step involves identifying the unique variables that influence your blood glucose levels. What happens after a fight with a family member, a poor night’s sleep, a head cold, a long hike, or a particular type of meal?
A big part of this learning process involves your response to different foods. Yes, a sugary soda will generate a rapid blood sugar spike in most people. However, we’re learning that there exists much greater variation in individual responses to different foods than previously thought. You may process a sweet potato very differently than someone else.
The third step involves using the continuous glucose monitor to track the progress of your behavior modifications. Basically, you run a set of experiments on yourself. What happens if you go to bed an hour earlier, meditate, eliminate a bedtime snack, eat brown rice instead of white, cut out soda and juice, or vary the carbohydrate content of your meals? Once you learn how you respond, you can change your habits and see the benefits.
Often after a month or two, the law of diminishing returns kicks in and the rate of new knowledge declines. If successful, you reach a new equilibrium of behaviors and maintain your blood glucose at a healthier level. You won’t need continuous glucose monitoring in the long term.
Some people may require more time or another round of usage. However, for those without medication-treated diabetes, the process should be relatively brief.
Final Thoughts
We’re living amid a silent epidemic of metabolic dysfunction. Many diabetics, and the vast majority of those with prediabetes, are unaware of their status.
At Banner Peak Health, we’re careful to identify risk factors like prediabetes and diabetes and are very aggressive in working with patients to mitigate their risks. Continuous glucose monitoring provides patients with a powerful tool to learn about their unique glucose metabolism and guide them to better health.
Footnote:
1. HgbA1c measurement relies on an interplay between red blood cells and glucose in the blood. Hemoglobin is a large, complex protein that binds iron and carries oxygen in the blood. Red blood cells are packed with hemoglobin, allowing them to transport oxygen throughout the body.
Red blood cells last about three months before they’re degraded, and their hemoglobin is broken down and recycled. Glucose sticks to hemoglobin molecules in a dose-dependent fashion. The higher the concentration of glucose, the more of it will stick to hemoglobin.
HgbA1c reflects the percentage of hemoglobin molecules with glucose stuck to them. Because red blood cells and the hemoglobin within them only last around 90 days, HgbA1c reflects an average level of glucose in the blood during that time.
Fish Oil: To Take or Not to Take

For me, 2024 is a year of introspection and growth.
I’m redefining my professional role and optimizing my own health. The two are intertwined under the umbrella of “me-search,” which involves using myself as a subject in a series of N=1 trials to better understand the latest healthcare techniques.
Being on the “cutting edge” of medicine requires a critical approach to evaluating and selecting medical options. Unfortunately, the metaphor of a sharp instrument doesn’t accurately describe the current landscape. It’s the opposite — an amorphous blob better represents the rapidly growing pool of heavily hyped, minimally evaluated medical treatments. Strolling down the supplement aisle or googling “weight loss” unleashes an avalanche of options.
Separating the wheat from the chaff isn’t easy.
For example, my new primary care doctor recommended I take a fish oil supplement to protect my heart. I trust her advice, but I also wanted to review the current medical evidence for fish oil supplements. Like many dietary supplements, the general consensus has swung back and forth.
Our story begins on a frigid ice floe in the North Atlantic…
Early Fish Oil Studies
In the 1970s, researchers noted that the native population of Greenland had lower rates of cardiac disease than those in Denmark or the United States, despite a diet much higher in saturated fats. These epidemiological findings led to the idea that people in Greenland who ate more marine vertebrates (whale, seal, and fish) had higher levels of n-3 fatty acids, which made them less likely to get heart disease.
In 1985, a new study demonstrated the cardioprotective effects of n-3 fatty acids in fish. A randomized cohort of heart attack survivors either ate two meals of oily fish a week or not. After two years, the group that ate oily fish had a 29% lower all-cause mortality rate than the group that didn’t.
Researchers then attempted to assess the benefit of n-3 fatty acids as a dietary supplement rather than through fish consumption.
Before exploring more recent fish oil studies, I want to describe some methodological challenges in conducting high-quality nutritional research.
The Challenges of Medical Research
The preponderance of poor-quality research has made nutritional advice the laughingstock of Western medicine. The frequent back-and-forth of conflicting advice makes the average politician appear steadfast:
Eggs are good for you. Eggs are bad for you. Don’t eat butter; eat margarine. Don’t eat margarine — it’s loaded with trans-saturated fat that will kill you. Calcium supplements make your bones strong. Calcium supplements are bad for your heart.
Flawed research methodologies generate conflicting advice.
Most nutritional research relies on epidemiological studies, observing who consumes what and the outcomes. This type of research has advantages: You can study many people, and more people will volunteer to fill out a questionnaire every year than eat prepackaged food for every meal for six weeks.
Epidemiological studies are also easier and less expensive, allowing them to run for many years. The study subjects represent the general population instead of the few people willing to volunteer for an interventional study.
However, dietary epidemiological studies have significant shortcomings. Can you remember everything you ate yesterday? Six weeks ago? Six months ago? Self-reported dietary questionnaires are a notorious source of error.
Also, individuals who may have suffered a bad outcome, such as cancer, can remember in much greater detail what they may have eaten in the past, introducing another form of bias.
However, the largest source of error stems from the principle that association does not equal causation. A study might find that ice cream consumption is associated with a higher risk of drowning, but this doesn’t mean ice cream consumption causes drowning. Rather, both are more likely to occur during hot weather.
There can be confounders: variables associated with both the possible risk factor and the clinical outcome being studied.
Epidemiological literature is replete with examples of supplements such as vitamin E and folate that purportedly reduce the risk of heart disease and antioxidant supplements that reduce the risk of cancer. They frequently overlook the potential “healthy lifestyle” confounder.
An individual who chooses to take a vitamin E or antioxidant supplement is often very different from someone who doesn’t take either supplement. The decision to take any supplement can be a marker for a whole host of other choices associated with better health outcomes — more sleep, less alcohol intake, more exercise, and an overall interest in maximizing one’s health.
Thus, the supplement didn’t cause a better health outcome per se. Rather, taking the supplement was a marker for variables associated with a better health outcome.
To create better nutritional studies, researchers have turned to the gold standard for interventional trials: the placebo-controlled, double-blind, randomized controlled trial.
What Is a Randomized Controlled Trial?
In a randomized controlled trial, half the participants are randomly assigned to receive the intervention and the other half to receive a placebo. Neither the study subject nor the researchers are aware of the treatment allocations.
The confounder problem is eliminated because, with a large enough study population, the randomization process should create two equivalent groups. Any confounders would be evenly distributed between the two groups and not contribute to a net difference in effect. This methodology forms the foundation of our assessment of drug therapies.
However, there is one tremendous difference between a randomized controlled drug trial and a nutritional supplement: Before starting a drug trial for a cholesterol-lowering medication such as rosuvastatin, none of the study participants would have rosuvastatin in their bodies.
That is not the case in many nutritional intervention studies, where study subjects have a range of baseline values. (Please see the appendix below for a more detailed discussion.)
For example, a study of vitamin D supplementation, a hormone the body makes in response to sunshine, may have a very different result when conducted in Norway, near the Arctic Circle, than in Costa Rica, near the equator. One could argue that the variability in baseline values shouldn’t be a factor because they’re the same in the intervention and control groups. However, this phenomenon can still critically weaken the studies and, I believe, heavily contribute to the uncertainty in interpreting fish oil supplementation studies.
In statistics, “power” refers to the likelihood of detecting a difference between study groups, should one exist. In practical terms, when designing a study, the smaller the effect size you hope to detect, the more study subjects you need to demonstrate a statistically significant result. The opposite is true for larger effect sizes.
Intuitively, this makes sense. If a hypothetical antibiotic cured 90% of everyone who received it compared to only 20% of those receiving a placebo, not as many study subjects would be needed.
However, a blood pressure medication that only reduced systolic blood pressure by a few points would require many study subjects to demonstrate a difference with statistical significance.
Whenever a study concludes that there was no treatment effect, was there actually no treatment effect, or was the study “underpowered” (that is, there weren’t enough study subjects for the magnitude of clinical benefit to demonstrate statistical significance)?
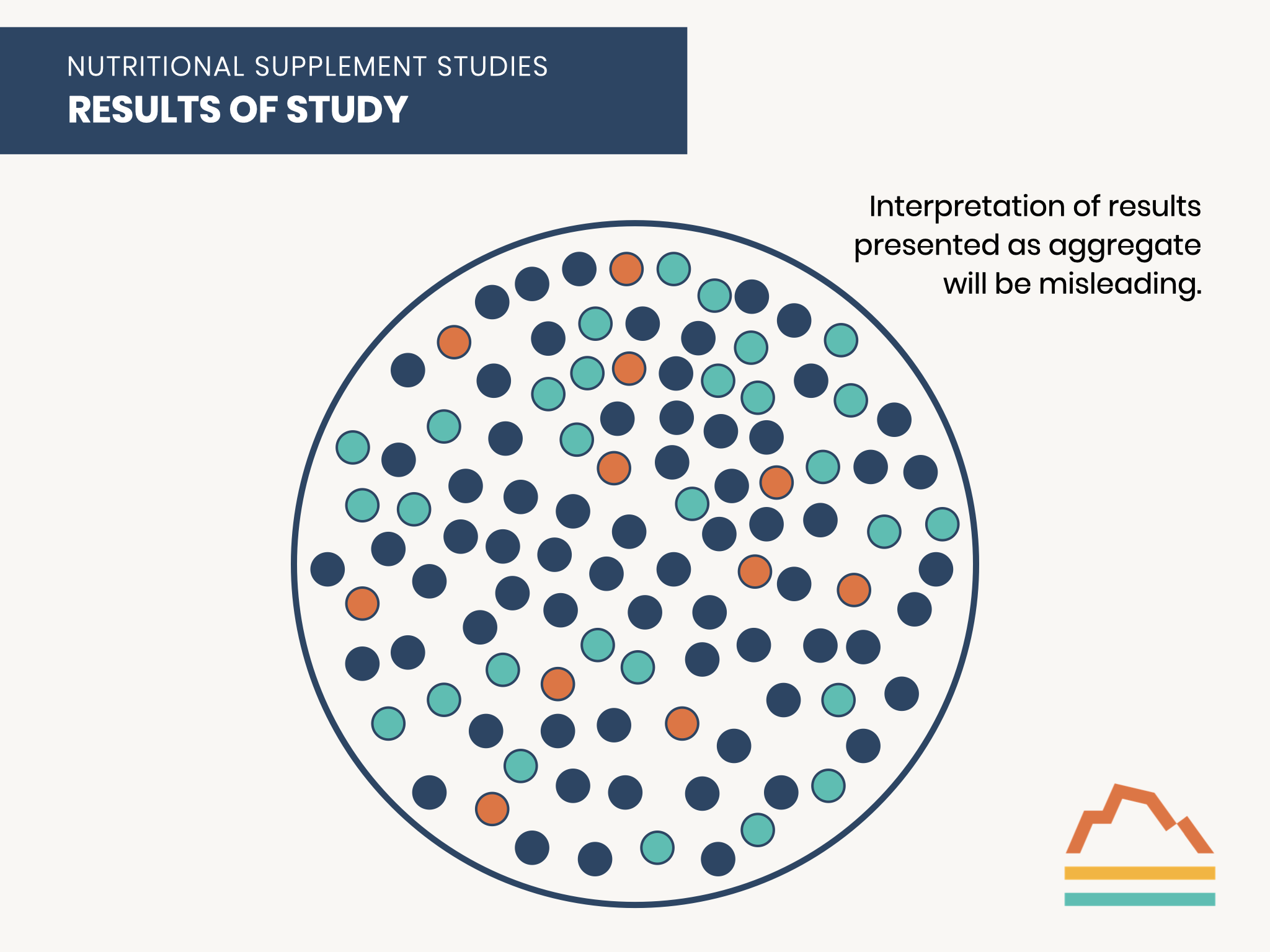
Let’s return to a hypothetical cohort of individuals enrolled in a nutritional supplement study, such as for fish oil. The study subjects are divided into three subsets based on their starting baseline level of n-3 fatty acids, the active ingredient in fish oil:
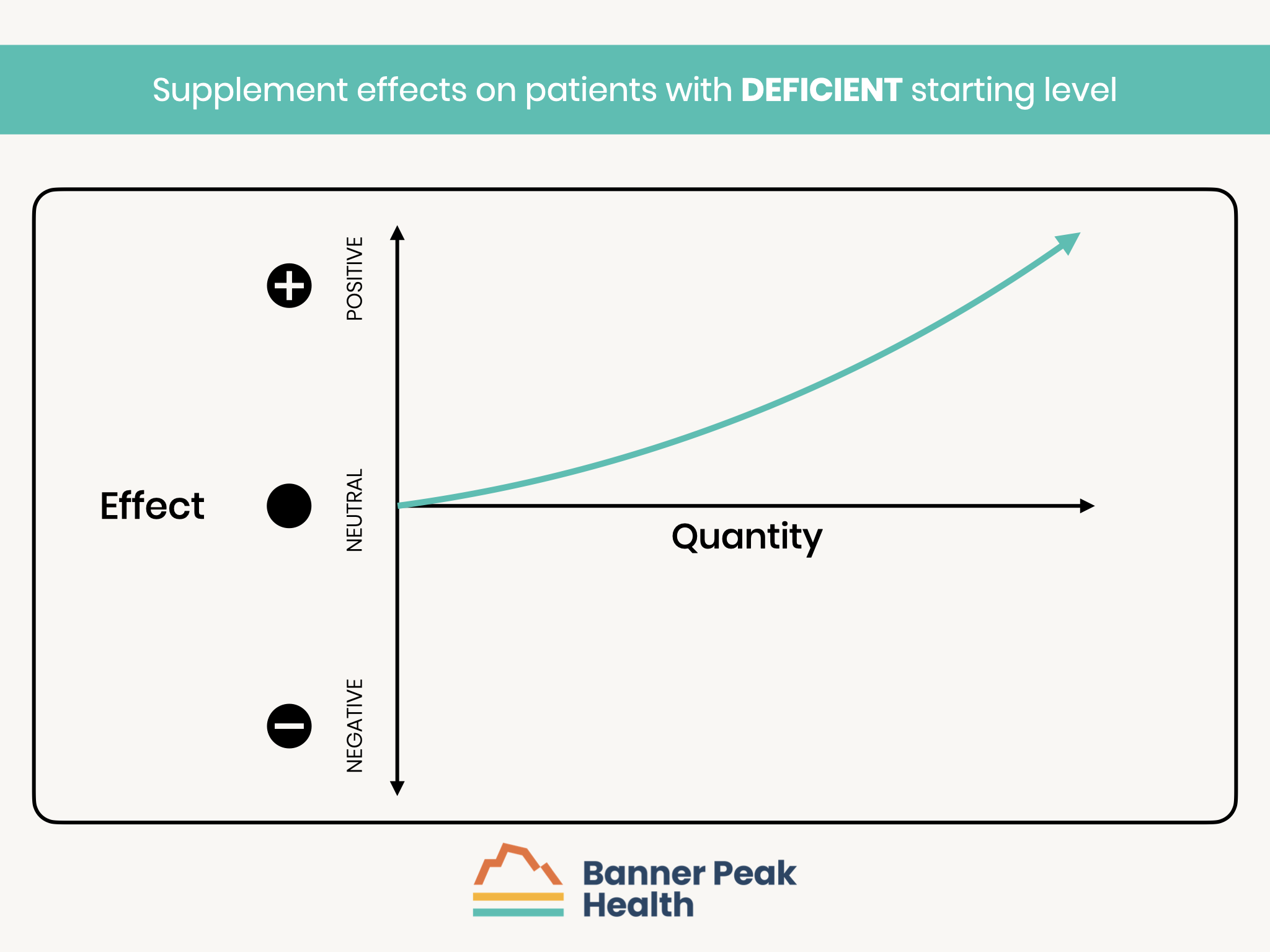
- Those with a deficiency of n-3 fatty acids are expected to have the greatest benefit from supplementation.
- Those with a normal level of n-3 fatty acids may receive little or no benefit from supplementation.
- Those with an excess of n-3 fatty acids may suffer side effects from further supplementation.
Ideally, you would measure each participant’s baseline level, categorize them into a subset, and study each group’s physiological responses separately.
Fish oil studies haven’t followed such protocols, but some offer interesting clues.
The VITAL Study
The VITAL study, published in the prestigious New England Journal of Medicine in 2019, became the definitive study for evaluating fish oil supplementation’s effect on cardiovascular disease and mortality.
With careful methodology and over 25,000 study participants, the study concluded that “omega-3 fatty acid supplementation did not reduce major cardiovascular events,” which became the prevailing wisdom.
Based on that study, I stopped taking fish oil supplements. However, that much-publicized conclusion masked a very different story.
First, the study demonstrated no significant difference in treatment groups for major cardiovascular events (the cumulative total of myocardial infarction, stroke, or death from cardiovascular causes). Yet, some outcomes showed benefits of fish oil supplementation: a 28% reduction in myocardial infarction (MI) and a 50% reduction in death from an MI.
The analysis I was most interested in was hidden in the supplemental material (available separately online but not included in the published document): The study participants weren’t stratified according to their n-3 fatty acid baseline levels.
However, they were analyzed according to whether they consumed more or less than an average of 1.5 fish meals per week, which would be expected to correlate with baseline levels. Out of 25,435 study participants, 13,514 reported eating less than an average of 1.5 fish meals per week.
The less frequent fish eaters showed a statistically significant 19% reduction in major cardiovascular events — the opposite conclusion of analyzing the entire cohort. By analyzing the subgroup of the population with a probable deficiency, the study demonstrated a statistically significant improvement with supplementation. This proves my point that the key to conducting a meaningful supplement study is to analyze those who actually have a deficiency.
When assessing whether to implement findings from a research study, “generalizability” becomes important — that is, are the participants and treatments evaluated in a particular study comparable to the patient sitting in front of you in the clinic? For example, a treatment that works great for young military recruits may not be the best choice for a frail 90-pound woman.
The VITAL study results are generalizable: if you have a suspected or documented low level of n-3 fatty acid, fish oil supplements are proven to reduce your risk of major cardiac events. Unfortunately, the press popularized the opposite conclusion.
Since the VITAL study’s publication, several large meta-analyses of fish oil supplementation for cardiac health have been published that support fish oil’s benefits. (A meta-analysis combines the data from multiple studies to create a much larger cohort to analyze.) This increases the study’s power and the ability to find statistically significant treatment effects.
Again, this supports my contention that early fish oil studies were effectively “too small” because only a subset of the participants were deficient in n-3 fatty acids and could be expected to benefit from supplementation.
My primary care doctor felt my n-3 fatty acid levels were borderline. In the context of my elevated blood pressure and borderline cholesterol levels, she believes fish oil supplementation will safely and effectively reduce my risk for adverse cardiac outcomes (in addition to other prescribed medications).
Fish oil supplements are very safe. Side effects are usually limited to gastrointestinal events such as indigestion and “fishy-tasting” belches. Fish oil has a very mild anticoagulant effect, which is one of the mechanisms for its beneficial effects. However, if you’re already on a prescribed blood thinner such as Plavix, Eliquis, or Xarelto, please ask your doctor about the risks and benefits of adding fish oil.
Some fish oil preparations contain mercury, a toxic metal. Unfortunately, our oceans are so polluted with mercury that it’s become part of the marine food chain.
Even the smallest creatures, such as plankton, can accumulate mercury. The fish that eat the plankton concentrate the mercury, and the bigger fish that eat the smaller fish continue to concentrate the mercury. Thus, larger fish, such as tuna and swordfish, have higher mercury levels than smaller fish, such as anchovies and sardines.
Higher-quality fish oil manufacturers use exclusively smaller fish and don’t have problems with mercury contamination.
I’ve begun taking fish oil from Nordic Naturals. They use only small fish and manufacture high-quality products, and their capsules don’t need to be refrigerated until after opening the bottle.
Fish oil can degrade if stored too long in a warehouse or exposed to extreme heat during shipping. I recommend ordering directly from Nordic Naturals — they’re careful about how they store and ship their products.
At Banner Peak Health, we strive to be at the forefront of healthcare, particularly prevention. We’re always looking for aspects of cardiovascular risk to identify and mitigate. Low levels of n-3 fatty acids are an important risk factor that can be safely treated with fish oil supplementation.
Appendix:
Many randomized controlled trials of dietary supplements suffer from the design flaw of aggregating all study participants regardless of their baseline levels.
This population can more accurately be considered as composed of three sub-groups: those with deficient, normal, or excess levels before any supplementation.
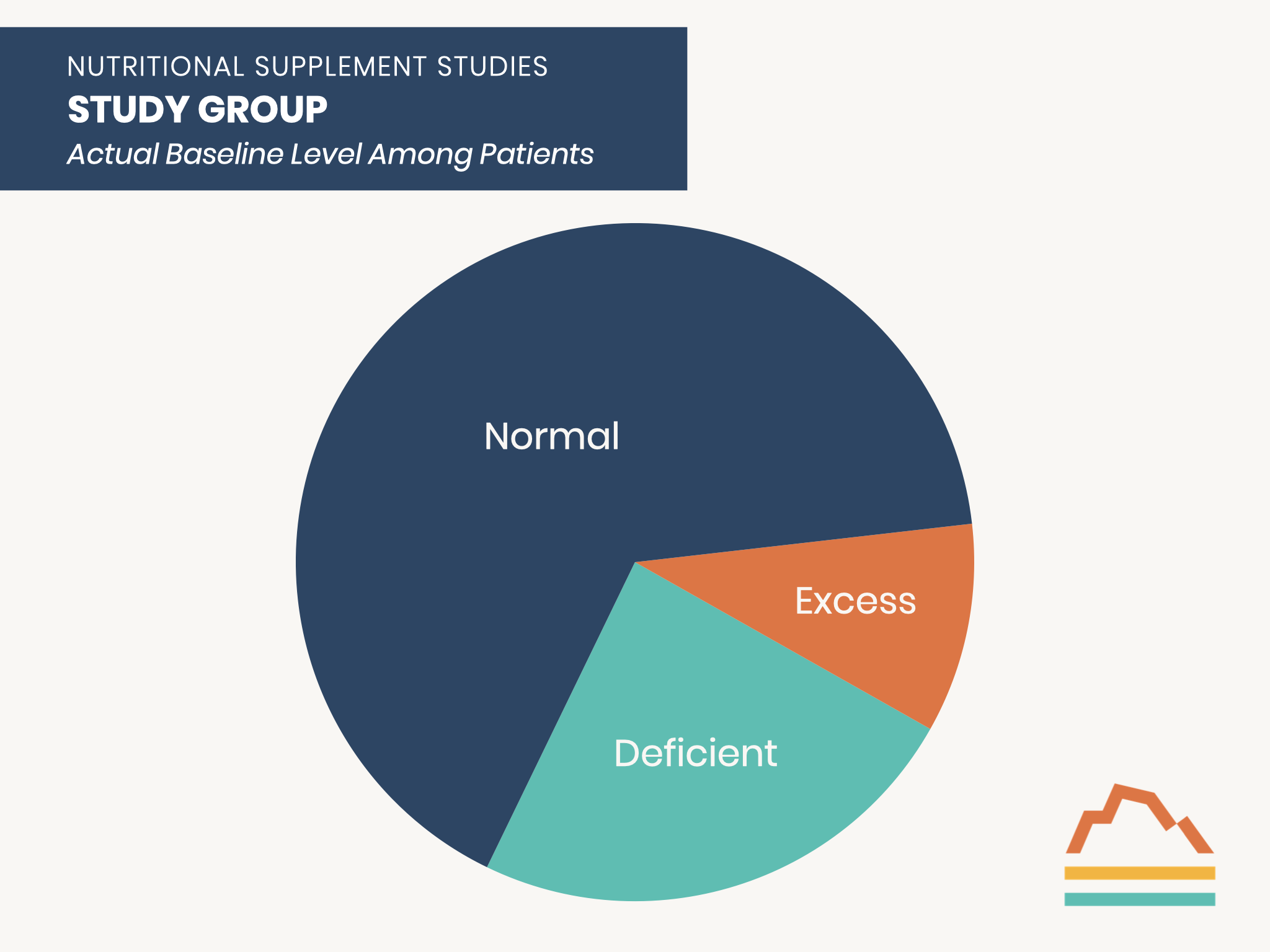
Those who are deficient at baseline are the ones who can benefit from supplementation.
Those with normal baseline levels would NOT be expected to benefit from supplementation.
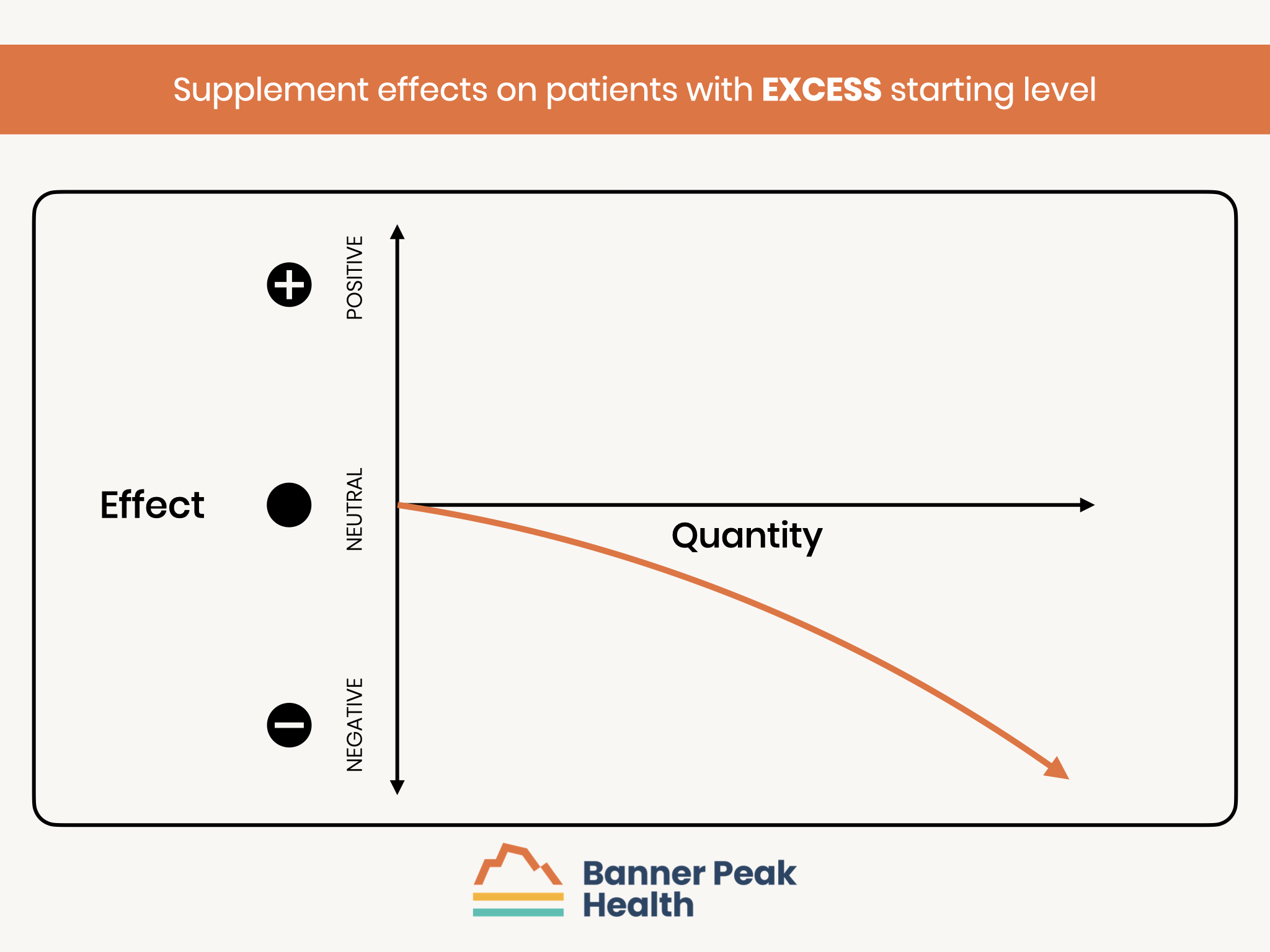
Those with excess levels at baseline are at risk of a worse outcome with additional supplementation.
Therefore, an analysis of the entire cohort may not have the statistical power to detect a treatment benefit because the number of participants with the possibility of improvement may be too small to reach statistical significance.
A Physician’s Experience With High Blood Pressure

I was perhaps nine or 10 years old when I first learned about blood pressure.
My father practiced general dentistry. One year, I accompanied him to a dental convention in San Francisco. For some inexplicable reason, in the massive convention hall, someone was giving away cups of Coca-Cola (a sugary, acidic beverage — one of the most caustic substances to the teeth ever ingested by humans). This was my first time sampling a caffeinated beverage.
As luck would have it, I stopped by another booth demonstrating the then-new technology of an automated blood pressure machine. I don’t remember my results, but I was told, “Your numbers are high. You should see your doctor.”
A repeat blood pressure measurement by my pediatrician turned out normal, and I was told, “You’re really sensitive to caffeine’s effects!” Thus began my understanding that my blood pressure was labile, sensitive to triggers that made it rise appreciably.
As an adult, I often display white coat hypertension: My blood pressure readings are more elevated when taken in a medical setting than at home. I’m an anxious person, and blood pressure measurement releases stress hormones such as adrenaline that can increase my blood pressure. Over the last year, I’ve generated some concerning readings in the doctor’s office in the 150–160/90 range.
Thus, I’ve been on both sides of the stethoscope when confronting white coat hypertension.
What Is White Coat Hypertension?
It’s often difficult for physicians to interpret office-based blood pressure measurements. As I discussed in a prior blog post, various factors related to office-based testing (for example, rushing into an appointment late) can introduce errors.
White coat hypertension — a condition where patients exhibit elevated blood pressure in a clinical setting — occurs in an estimated 15–30% of patients. Home testing isn’t without its pitfalls, either. Incorrect timing of readings, such as during moments of distress or pain, and automated blood pressure cuffs’ inaccuracy, can lead to errors.
As I often emphasize, the seemingly simple task of measuring blood pressure is anything but.
To get the most accurate readings, measure your blood pressure at home using the following criteria:
- Use a high-quality machine such as the OMRON cuff.
- Choose an environment where you can rest comfortably.
- Take three readings every five minutes and average the final two.
- Take your cuff to your doctor’s office to calibrate it with their manual cuff and stethoscope.
When carefully following these rules, I would get readings around 130/80 — much lower than in an office environment, but still not optimal. Furthermore, recent evidence suggests that white coat hypertension, even with normal at-home readings, may confer up to a 36% increased risk for cardiovascular events (such as heart attack and congestive heart failure) as well as up to a 200% increased risk of dying from heart disease.
My primary care doctor told me what I already knew: I needed to get my numbers down.
I’m not alone. In the United States, an estimated half of all adults have elevated blood pressure. Over age 60, the rate rises to almost two-thirds (63%). Unfortunately, the majority of hypertension cases aren’t well-controlled.

Primary vs. Secondary Hypertension
The etiology of hypertension can be divided into primary and secondary hypertension. The latter refers to a specific, identifiable illness that raises blood pressure. Examples include:
- Hormonal disorders such as hyperthyroidism — too much thyroid hormone — and Cushing’s Syndrome — too much cortisol.
- Problems with vascular anatomy such as renal artery stenosis, which starves the kidney of blood supply and causes it to overproduce hormones such as renin, which raises blood pressure.
In only about 5% of hypertension cases can a specific cause be identified. The other 95% of cases are referred to as primary hypertension, also known as essential hypertension. (“Essential” means “we don’t know why,” analogous to the medical terms “idiopathic” or “non-specific.” Medicine has a wonderful vocabulary for camouflaging our lack of knowledge.)
We can’t identify the specific causes of essential hypertension, but we do have a good understanding of its associated risk factors, such as obesity, family history, age, physical inactivity, stress, sleep apnea, and alcohol and cigarette use. Reducing these risk factors can improve blood pressure.
Nonetheless, it’s important to recognize that each risk factor doesn’t correspond to a single disease process responsible for high blood pressure.
What Can Cause Essential Hypertension?
By writing this blog post, I’ve finally wrapped my head around the concept of essential hypertension. Understanding the differences in the philosophy of disease etiology between traditional Western medicine and Chinese medicine provides useful insights:
- Western medicine relies on a linear, reductionist philosophy and works to identify the single cause of a disease (too much of a hormone, a defective protein, a DNA mutation, etc.).
- Chinese medicine views illness as an imbalance of interconnected systems — a hanging mobile that gets knocked askew.
Following the Chinese medicine philosophy, essential hypertension can be represented by an old-fashioned watch run by countless interconnected wheels and gears. As one gear becomes defective, it impacts the gears around it, and so on.
Many gears can become damaged, any of which can wear out the others. The damage can be irreversible and is best prevented early on.
If left untreated, high blood pressure becomes a progressive disease. Many “gears” contribute to this process. Here are four common ones:

Vascular Changes
Arteries are the blood vessels that transport blood from the heart to the rest of the body. Arterioles are mid-sized arteries that direct blood to its appropriate location: for example, to the muscles for physical activity or the digestive tract after a meal.
Arterioles’ walls are lined with smooth muscle tissue, which contracts and relaxes to direct blood to the appropriate location. In response to elevated blood pressure, the smooth muscle lining thickens to exert control over the vessels. The thickening process makes the blood vessels stiffer, requiring greater pressure to move the blood through them, creating a vicious cycle of rising blood pressure.
Autonomic Nervous System Dysfunction
Prior blog posts have described the sympathetic and parasympathetic nervous systems’ roles in regulating the body’s organs.
The sympathetic and parasympathetic nervous systems control our blood vessels. They coordinate important reflexes such as ensuring adequate blood supply to the brain and maintaining adequate blood pressure when our bodies change positions. These baroreflexes can be reset in response to high blood pressure in such a manner that they raise the blood pressure even further to accomplish their functions.
Hormonal Responses
The Renin-Angiotensin-Aldosterone System (RAAS) is a series of hormones that regulate blood volume and pressure. The system has evolved to maintain adequate blood perfusion of our organs despite potential challenges that may lower blood pressure, such as acute blood loss or dehydration.
While it’s important to have a system that raises blood pressure in an emergency, persistent over-activation of the RAAS can continue the progressive rise in blood pressure by developing a higher set point.
Endothelial Cell Dysfunction
Endothelial cells line each artery’s interior. These cells are hormonally active with local signals that control even the smallest arteries’ constriction or relaxation. For example, nitric oxide is a locally released molecule that causes that region of the artery to open more.
Endothelin is a small protein that causes regional constriction of the artery. These and other locally vasoactive hormones function in a delicate balance to control blood supply through small arteries. High blood pressure disturbs this equilibrium, leading to an eventual predominance of the signals that tighten arteries and raise blood pressure.
Vascular changes, autonomic nervous system dysfunction, hormonal responses, and endothelial cell dysfunction are just four systems among many that regulate blood pressure. Furthermore, they all interact with each other, creating a domino effect that perpetuates a progressive rise in blood pressure if left untreated.
Unfortunately, high blood pressure paves the way for a distressingly long list of complications, including heart attack, stroke, kidney failure, abnormal heart rhythms, sexual dysfunction, blindness, and congestive heart failure. High blood pressure’s dangerous and progressive nature places a premium on early and aggressive control.

My Blood Pressure Treatment
The first step to lowering blood pressure relies on lifestyle modification and, if that fails, initiating drug treatment.
I had already been careful with my lifestyle choices — I was of a normal weight, followed a good diet, wasn’t a smoker or heavy drinker, and was physically active. There was no excess ballast to jettison to lighten my load. Thus, initiating drug treatment would be the next step.
I’ve been extremely fortunate to have lived 61 years without requiring a long-term daily prescription medication. I’ve devoted considerable attention to making healthy choices. I felt being “drug free” was my reward and an important part of my identity. As a physician, I was proud to have talked the talk and walked the walk.
Nonetheless, I’m aware that preventing illness is far more important than pride in not needing any prescription medications.
My primary care doctor prescribed a very low dose of a medication called olmesartan, an angiotensin receptor blocker (ARB). In general, a “start low and go slow” approach to initiating any medication allows the body more time to adapt to drug-induced physiological changes. In the case of blood pressure management, this may require more steps of increasing the medication dosage until the target blood pressure is achieved. However, it reduces the probability of side effects.
In my case, I’m a “lightweight” regarding any ingested substance, more sensitive than others in terms of dose and effect. At an early age, I learned that I can’t even tolerate a cup of Coca-Cola, and as an adult, I developed migraine headache syndrome with multiple food and medication triggers. Fortunately, I haven’t needed many medications, but of those I’ve been prescribed, half have triggered a migraine.
Why start with an angiotensin receptor blocker to reduce blood pressure? This medication category works by interrupting the Renin-Angiotensin-Aldosterone System’s (RAAS) signaling. Given hypertension’s progressive and chronic nature, the prescribed medications are usually taken for many years. Therefore, there can be little tolerance for side effects.
The ARB class of hypertension medications has one of the lowest risks for side effects as well as a solid record of reducing the risk of complications such as heart and kidney disease.
A simple story would entail me starting a low dose of olmesartan and effortlessly reaching a blood pressure at rest of 120/70 with no complications. However, life can be complicated.
Olmesartan comes in tablets ranging in dose from 5 mg to 40 mg. Given my history of medication sensitivity, I started by taking half of a 5 mg pill each evening with no change in resting blood pressure at home of around 130/80. After a week, I progressed to 5 mg each evening and immediately noticed the onset of a mild migraine headache.
I need to start and stop olmesartan a few times to definitively establish causation, but I’m not optimistic about this medication. I’ll probably need to try other ARB medications.
What I’ve Learned From My Blood Pressure Journey
Transiently elevated and moderately elevated at-rest blood pressure readings still confer an unacceptable risk level.
Because of elevated blood pressure’s progressive nature, the longer you wait to initiate treatment, the harder it’ll be to achieve adequate control.
Lifestyle modifications, such as weight loss and exercise, are vital for reducing blood pressure. However, many people, myself included, require medication treatment to achieve a sufficient reduction in blood pressure.
If it isn’t an emergency, it’s best to start antihypertensive medications at a low dose and gradually increase the dosage if tolerated.
Blood pressure medication side effects can occur. Arriving at a well-tolerated and efficacious medication regimen may require trial and error.
Finally, it’s far better to improve your health than to merely perceive yourself as being healthy.
The Transformation of Sleep Medicine
Like many doctors fascinated by new medical technology, I have succumbed to “me-search”: the urge to use new technology to study myself. Me-search optimizes my own health and teaches me how to use new technology to help patients.
Last October at a medical conference, I learned about Empower Sleep, a new sleep medicine telehealth company. Empower Sleep promises to transform sleep medicine using a device called the SleepImage Ring.
I’ve always struggled with sleep due to a smorgasbord of areas for improvement:
- Nasal obstruction due to hay fever
- Bruxism (nocturnal teeth grinding)
- Nocturia (arising more than once a night to urinate)
- Light sleeping (more sensitive to disruption from environmental stimuli)
- Advanced sleep phase disorder (arising too early in the morning)
- Preterminal insomnia (awakening before the end of the night, often associated with depressive illness)
Me-search overtook me. I had to try the SleepImage Ring for myself.
(Disclaimer: I have no financial interest in SleepImage or Empower Sleep. I do refer patients to Empower Sleep for treatment.)
What We’ve Learned About Sleep
From time immemorial, sleep was thought to be an inactive state between wakefulness and death. Sleep was understood as a passive, inactive state defined by lack of consciousness. Dreams represented a peek into this realm and were thought to carry mystical, psychological, and/or religious meaning.
In 1928, we gained the ability to peer into sleep’s biology when German psychiatrist Hans Berger developed a way to record the electrical activity of the brain’s neurons. The electroencephalogram (EEG) revealed distinctive waves of neuronal activity unique to sleep.
By the 1950s, an EEG-defined sleep phase associated with rapid eye movements (REM) and dreaming had been characterized, and the concept of sleep architecture was born. By the 1960s, EEG-based polysomnograms (PSG) were used to diagnose and treat sleep disorders.
We now know that sleep occurs in 90-minute cycles that repeat through the night. Each cycle contains lighter portions, S1 and S2, and deeper portions, S3, called slow-wave sleep (SWS). Each cycle also contains REM sleep and brief arousals.
The composition of those 90-minute cycles changes throughout the night: more slow-wave sleep occurs early, and more REM sleep occurs later. The amount of slow-wave sleep diminishes as we age, while the percentage of REM sleep is preserved.
Many other factors can affect sleep’s composition, including:
- Illnesses such as obstructive sleep apnea (OSA)
- Medications such as benzodiazepines (drugs like Valium)
- Beverages such as alcohol
The Current State of Sleep Testing
EEG-based polysomnograms have been the dominant method of diagnosing sleep disorders for over 50 years, forming the foundation of sleep medicine. However, a polysomnogram is an extremely cumbersome test.

The patient must travel to a special overnight clinic and fall asleep with 22 separate wires attached to their body, which measure:
- Brain wave activity
- Airflow
- Eye movement
- Oxygen saturation
- Heart rate and rhythm
- Muscle tone in the chin, chest wall, and legs
Newer home sleep studies have reduced the number of attachments needed and allowed the patient to sleep in their own bed. However, both in-clinic and at-home studies may influence the sleep being measured.
Think about how well you slept last week. For most of us, the night-to-night experience of sleep varies. Any single night of sleep (let alone with 22 wires attached!) may not represent a typical night.
Neither in-clinic nor at-home tests are practical for multiple nights of testing. Repeating a study allows for the assessment of treatment modalities and sets up a series of trial-and-error experiments to optimize sleep.
Fortunately, we’re amidst a quiet revolution in our understanding of sleep’s physiology.
The Sleep Revolution
For the last hundred years, we’ve classified sleep based on the brain’s electrical activity as measured by an electroencephalogram. However, sleep entails not just brain activity but characteristic changes throughout the entire body, including breathing, heart rate, blood pressure, and body temperature.
About 15 years ago, researchers began developing a new method for analyzing sleep based on changes that occur to our autonomic nervous system (ANS). The autonomic nervous system is a network of nerves that regulate unconscious processes that keep our body functioning, including breathing, digestion, and heart pumping.
The autonomic nervous system is divided into two categories: the sympathetic (SNS) and parasympathetic (PNS) nervous systems:
- The sympathetic nervous system mediates our “fight or flight” response — increasing our breathing rate, shunting blood to our muscles, making the heart pump harder, and putting more fuel into the bloodstream for muscular activity.
- The parasympathetic nervous system mediates “rest and digest” functions such as improving blood flow to the digestive tract and secreting digestive enzymes.
The sympathetic and parasympathetic nervous systems exist in a delicate balance, as every organ receives signals from both systems.
For example, in the cardiopulmonary system (heart and lungs), signals oscillate back and forth in a teeter-totter fashion, and each breath subtly alters the heart rate:
- During each breath in, called inspiration, the sympathetic nervous system predominates and slightly speeds up the heartbeat.
- During each breath out, called expiration, the parasympathetic system slightly predominates and slightly slows down the heartbeat.
Thus, continuous recording of every heartbeat demonstrates variation in timing that correlates with the respiration rate. Exactly how much variability reflects the strength of the sympathetic nervous system’s input relative to the parasympathetic nervous system’s. A stronger parasympathetic nervous system creates more variability and correlates with better health outcomes.
Breathing also affects the amount of blood pumped each time the heart contracts. Each heartbeat during expiration moves a bit more blood than each heartbeat during inspiration.
A new technique called cardiopulmonary coupling (CPC) generates one waveform reflecting the change in heart rate and a second waveform reflecting the change in blood output. By analyzing the relationship between these two waveforms, researchers assess how the autonomic nervous system functions during sleep.
Cardiopulmonary coupling is a brand-new lens we can use to view sleep. EEG describes sleep from the vantage point of the brain’s wave changes, while cardiopulmonary coupling divides sleep into different stages based on differences in the autonomic nervous system.
CPC vs. PSG: What’s the Difference?
Cardiopulmonary coupling results and polysomnogram results classify non-REM sleep (NREM) differently.
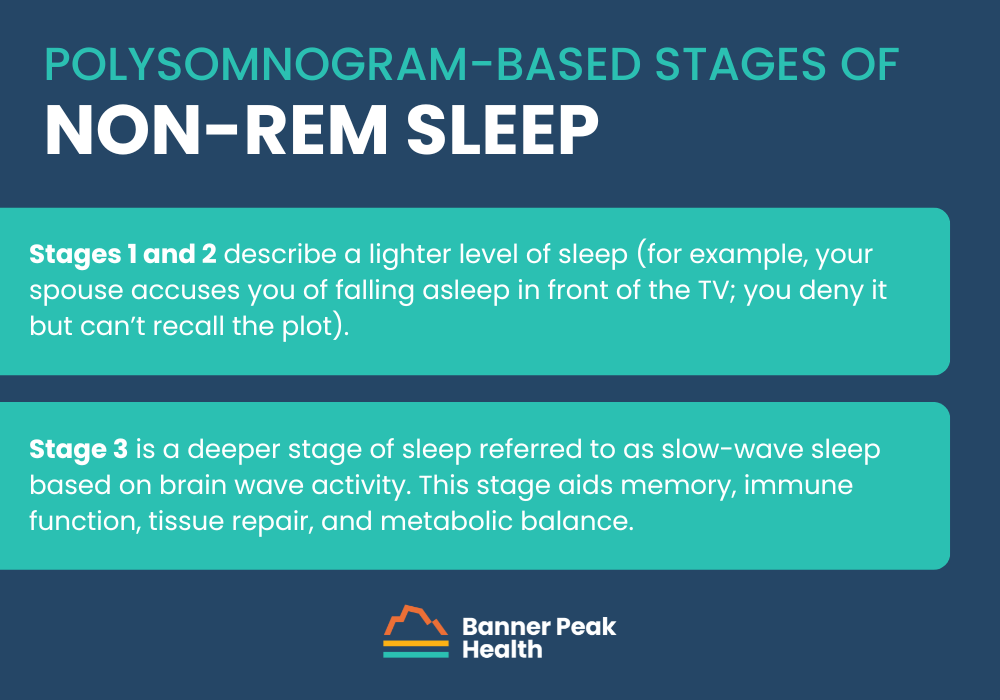
The traditional polysomnogram-based classification divides non-REM sleep into three stages of progressive depth:
- Stages 1 and 2 describe a lighter level of sleep (for example, your spouse accuses you of falling asleep in front of the TV; you deny it but can’t recall the plot).
- Stage 3 is a deeper stage of sleep referred to as slow-wave sleep based on brain wave activity. This stage aids memory, immune function, tissue repair, and metabolic balance.
Meanwhile, cardiopulmonary coupling categorizes non-REM sleep into stable and non-stable components. Stable non-REM correlates with slow-wave sleep but possibly provides a more accurate measure of this physiologically vital sleep stage.
The biggest advantage of cardiopulmonary coupling over polysomnograms is the ease of testing. A small rubber ring worn on your finger (like the SleepImage Ring, which uses cardiopulmonary coupling) provides almost as much information as 22 bulky wires (as in the case of a polysomnogram).
How Does the SleepImage Ring Work?
The SleepImage Ring harnesses an amazing new technology called photoplethysmography (PPG). Photoplethysmography powers our current array of consumer wearable devices, including the Fitbit, Garmin watch, Oura Ring, and WHOOP band, as well as medical grade, FDA-approved wearables such as the SleepImage Ring.
Photoplethysmography shines very small LED lights into the skin, illuminating tiny arteries under the surface. Adjacent sensors measure the reflected LED light, tracking the pulsatile pressure waves in the subcutaneous arteries and the color of the hemoglobin (oxygen-carrying protein) in the blood.
The pressure waves’ timing and amplitude measure the autonomic nervous system’s performance, and the hemoglobin’s color in the blood measures how well the lungs deliver oxygen to the body. The SleepImage Ring can also measure nocturnal movement and skin temperature.
Combining these data points paints a thorough picture of a person’s sleep. How many awakenings were there overnight? How much time was spent in vital stages such as REM and stable non-REM? Are there episodes of low oxygen indicating obstructive sleep apnea?
My SleepImage Experience
I started using the SleepImage Ring, hoping to gain insights that would minimize my sleep challenges. To my dismay, I discovered two new areas for improvement I’d been unaware of: a mild case of obstructive sleep apnea and an imbalance of my autonomic nervous system during non-REM sleep.
After monitoring multiple nights of sleep, my SleepImage Ring provided an assessment of my mild obstructive sleep apnea that was much more accurate than my one prior polysomnogram.
The SleepImage Ring tracked a tremendous amount of variation in the apnea-hypopnea index (AHI), the number of times per hour my breathing was compromised, ranging from 3 (normal) to 22 (moderate severity). My average was about 10, or mild.
Interestingly, in the traditional polysomnogram I underwent about 10 years ago, I struggled to sleep and the test revealed an apnea-hypopnea index of 5 (high normal). I suspect this is because the polysomnogram yielded only one night of compromised data.
Disheartened about receiving yet another sleep impairment diagnosis, I worked with Empower Sleep to use their cardiopulmonary coupling technology to address the problem. Not only is the SleepImage Ring better at diagnosing illnesses than polysomnograms are, but it also provides a better route for treating those illnesses.
Because my obstructive sleep apnea was mild, there was a good chance it could be treated without a CPAP machine. I was given a list of alternative therapies to try to reduce obstruction of my upper airway.
I incrementally added treatment modalities: nasal steroids to shrink the nasal mucosa and widen the opening of the nasal passages; lip tape to close my mouth, which pinched the tongue to prevent it from falling backward and obligated nasal breathing; and a soft rubber nasal device that further opens my nasal passages and reduces obstruction.
My bedtime routine has become more involved, and I’ve become quite a sight to behold in bed. But the process works! I now have several months of SleepImage data demonstrating the progressive reduction in my apnea-hypopnea index.
There’s still a fair amount of variation in my apnea-hypopnea index, but the average is now only a bit above normal. More importantly, I have more energy during the day.
My second discovery, an autonomic nervous system imbalance during non-REM sleep, represents a more complicated challenge because it’s a new disorder. Before the advent of cardiopulmonary coupling, autonomic nervous system impairments weren’t diagnosed by tracking sleep stages.
Because the disorder is so new, we don’t have good assessments of normal values associated with aging. There are only clues. We do know that EEG-based slow-wave sleep does somewhat correlate with the stable non-REM sleep stage.
We also know that slow-wave sleep declines with age. Therefore, we expect our autonomic nervous system’s function to decline, as well. Unfortunately, just as our skin gets “old and wrinkly” with age, so does our sleep.
Does my impaired autonomic nervous system function during sleep represent a normal age-related change, or can I improve it? As an athlete, I want to maximize the stable non-REM fraction of my sleep. That’s when “all the good stuff happens,” particularly the release of testosterone and growth hormone.
Unlike my clear victory over obstructive sleep apnea, I’m still working to overcome my impaired autonomic nervous system. I’ve expanded my meditation practice, targeting 20 minutes in the morning and 12 minutes before bedtime. (If you’d like to join me, review my step-by-step meditation guide.)
I’m also trying a very low dose of the antidepressant Lexapro, which I’ve used successfully to treat mild depression in the past. I’m not currently depressed, but there is a high probability that depression may be associated with a distinctive form of autonomic nervous system dysfunction during sleep.
My sleep data may represent a low-grade depression that medication can improve. The jury is still out on these interventions — I’ll keep you posted.
My Take on the SleepImage Ring
The SleepImage Ring represents a transformation in sleep medicine. More patients can be conveniently screened for sleep disorders, and more people can be effectively treated, especially those with obstructive sleep apnea.
Previously, only those with obvious obstructive sleep apnea symptoms underwent testing. Many people have the illness and don’t know it — I was one of them. They can now be diagnosed through greater use of sleep testing.
Also, less than half of people who are prescribed a CPAP machine to treat their obstructive sleep apnea can tolerate using it. Now we can use a trial-and-error method to build effective treatment regimens for those with mild and moderate obstructive sleep apnea, sparing them a CPAP machine.
The sleep medicine revolution has begun!
Exercise — The Real Fountain of Youth
In my last blog post, I introduced the Metric-Driven Empowerment Cycle (MDEC, pronounced “em-deck”), in which new health-monitoring technologies provide actionable data that informs behavior modification, which improves the patient’s health. MDEC-based healthcare focuses on preventing illness rather than simply treating it.
Most of the time, that data-informed behavior modification includes some form of exercise.
Exercise’s Impact on Heart Disease
Physicians have been prescribing exercise as medicine since Hippocrates’ day, but exercise benefits weren’t researched until 1953, when British epidemiologist Dr. Jeremy Morris studied transit workers on double-decker buses.
Dr. Morris compared the rate of coronary heart disease (CHD) among bus drivers, who sat for 90% of their shift, with conductors, who climbed over 600 steps a day. The sedentary drivers’ CHD rate was 42% higher than the conductors’.
Dr. Morris confirmed these findings in another study. He compared the rate of CHD among postal workers with desk jobs against that of workers who walked to deliver the mail. The former group had a 33% higher CHD rate.
Dr. Jeremy Morris died in 2009 at age 99. He swam, jogged, and cycled well into his old age.
We now have many decades of literature documenting the staggering health benefits of exercise. It reduces the risk of dementia, mitigates the effects of menopausal hot flashes, minimizes depression, prevents diabetes... I could go on.
Despite the billions of dollars spent on anti-aging drug research, exercise remains the best route we have to the mythical “Fountain of Youth.”

How Exercise Has Helped Me
I’m an avid cyclist. I’ve pedaled thousands of miles in my life, and I’m convinced that my many decades of commitment to fitness have reduced the impact of my genetic predisposition to cardiometabolic disease.
Obesity and diabetes run down both sides of my family tree. Both my parents were physically active, not overweight, and didn’t have diabetes or coronary heart disease. However, all their siblings were overweight and had manifestations of cardiometabolic disease such as high blood pressure, diabetes, and coronary heart disease.
In attempting to practice what I preach, I devote considerable effort to cardiovascular and strength training, working to maintain a normal weight with healthy levels of muscle and fat mass. Nonetheless, my parameters, such as blood pressure, cholesterol levels, and glucose levels, are still borderline — not the levels one would expect given my level of fitness and body composition.
I’m working hard against my genes. For both personal and professional reasons, I’m passionate about exercise’s role in maximizing health and longevity.
I look forward to helping all my patients set personal records and achieve athletic goals. Of course, the greatest gains will accrue to those who are currently the least fit.
The Exercise Dose-Response Curve
The human body is a machine that has evolved for movement. An inactive machine will rapidly break down, i.e., our bodies will devolve into a diseased state if we don’t keep moving.
None of our vital structures will operate appropriately. The heart won’t pump as efficiently. The joints will become stiff and more susceptible to injury. The body can go into caloric excess with surplus energy stored as fat, which gets distributed into abnormal locations such as the liver and muscle cells, creating inflammation and insulin resistance. And so on.
Fortunately, just as physical inactivity can trigger a negative cascade of events, physical activity can reverse the process.
There is an exercise dose-response curve that describes how health benefits change with increasing quantities of both cardiovascular and strength training exercise:
- The first section of the curve has a steep upward slope, reflecting a region that is the “best deal,” or the most improvement in health for even a minimal increase in exercise.
- The next region has a wide range of quantities of exercise in which “more is better” in terms of benefit.
- A small section of the maximum amount of exercise reflects a region in which “more is worse.”

Exercise is the most valuable for the least fit. For these people, exercise corrects a diseased, malfunctioning body. Those with higher levels of fitness can still improve their health but don’t have the same magnitude of dysfunction that needs to be addressed.
Once you advance beyond the steep upslope that rescues the physically inactive, the curve climbs appreciably before flattening. In this region of the curve, incrementally more fitness brings additional health benefits.
Large epidemiological studies illustrate this association by examining the link between longevity and VO2 max, the maximum volume of oxygen your body can use during peak exertion. VO2 max represents the fitness of your entire cardiopulmonary system, which is improved through exercise.
These studies demonstrate a consistent, stepwise improvement in longevity, beginning with the lowest rung of fitness and continuing to the top tier. In fact, the magnitude of benefit from moving from least fit to moderately fit (not even the top tier!) exceeds the reduction in mortality risk of quitting cigarettes or overcoming diabetes. Strength training and muscle mass maintenance also benefit the preservation of function and longevity.
Eventually, the graph slopes downward, which applies to extreme athletes (who compete and train for intense long-distance events, such as running an ultramarathon). They can train so hard that they overwhelm the stress/recovery cycle, creating a chronic inflammatory state with deleterious health effects.
This group comprises a minute fraction of the population but illustrates the concept that “too much of a good thing may no longer be a good thing.”
Final Thoughts
My goal is to see everyone reap the benefits of increased exercise. I also want to keep an eye out for those who may be overtraining.
Of course, the devil is in the details. Creating appropriate training regimens and motivating everyone will be an exciting professional challenge. Exercise will become the foundation of Medicine 3.0 at Banner Peak Health!
Medical Innovation — Our Approach
I’m a huge fan of physician Peter Attia, author of the book Outlive. He’s used his popularity to reshape the vocabulary of preventative medicine.
Attia defines “healthspan” as the number of years we can live with a high level of function, as opposed to “lifespan,” which is the number of years we’re alive regardless of health status.
He’s also coined the terms “Medicine 2.0” and “Medicine 3.0.” The former, a reactive, disease-based approach, treats existing illnesses. The latter prevents illness from developing by using a far-sighted approach.
Attia has become one of the best-known proponents of the “Longevity Medicine” movement, focusing on how to help people lead longer and more fulfilling lives. Prevention has always been a core aspect of primary care medicine, but Peter Attia has refocused its goals and created a growing demand for a more sophisticated level of prevention than has been available in traditional medicine.
Inspired by Peter Attia, I want to bring state-of-the-art preventative healthcare to Banner Peak Health, practice Medicine 3.0, and maximize patients’ healthspan.
Introducing the Metric-Driven Empowerment Cycle
I studied political economy as an undergraduate, focusing on how political and economic forces shape our society. I’ve retained this vantage point throughout my medical career.
In my last blog post, I described the term “diagnostic desert,” analogous to the term “food desert,” which is the scarcity of grocery stores in lower socio-economic neighborhoods. With no lucrative drug, surgery, or diagnostic procedure, vast areas of our healthcare system are underserved.
Most preventative healthcare falls into this category. Tragically, our current system incentivizes doctors to prescribe patients medication rather than work with those patients to help them live healthier lives.
Pharmacology plays a vital role in prevention, particularly in reducing the risk of hypertension and elevated cholesterol. However, our most potent tools for overall risk reduction stem from how we eat, sleep, exercise, and handle stress.
Practicing medicine at this level appears old-fashioned and low-tech. However, recent technological advances have enabled convenient, real-time, continuous monitoring of biomarkers in these areas. A small ring can measure the physiology of your sleep. A patch on your arm can record how your blood sugar varies throughout the day. By recording actionable data, these technologies provide the tools to fine tune and enhance the wearer’s health.
Harnessing these technological tools, we can follow a reiterative process to increase healthspan:
- Identify the health status to be improved
- Optimally measure the health status
- Use the diagnostic information to modify behavior
- Watch the new behavior improve health status
- Rinse and repeat
This cycle represents the foundation of preventative care at Banner Peak Health. We call it the Metric-Driven Empowerment Cycle (MDEC).
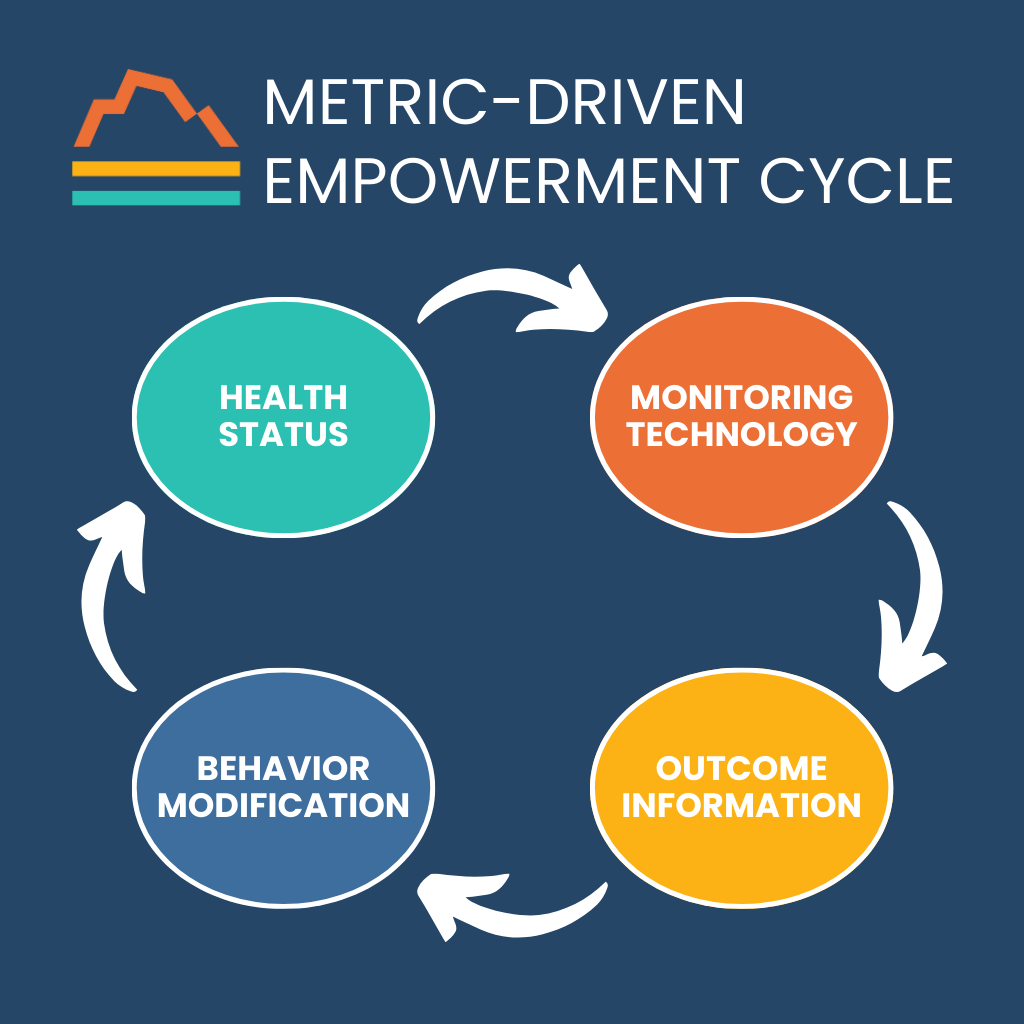
For example, we have a general sense of the quantity of sleep we get. When was bedtime? When did the alarm go off? Any awakenings during the night? However, our quality of sleep is unknown. By definition, we are unconscious when we sleep. Sleep is made up of restorative phases, such as REM and deep sleep, which conditions such as obstructive sleep apnea can disrupt.
Now, consumer wearables and medical devices allow the ongoing assessment of sleep quantity and quality. This technology allows us to diagnose potential problems and monitor and adjust treatment strategies.
Optimizing metabolic health offers another important area for monitoring technology. We know that elevated glucose (sugar) levels are associated with diabetes mellitus, which is a risk factor for many bad outcomes, including heart disease and strokes. However, pre-diabetes, a condition of insulin resistance but not full-fledged diabetes, can confer a significant risk of these bad outcomes as well. An estimated one in three adults in the United States is pre-diabetic.
New wearable technology can diagnose and manage this extremely common, “hidden” risk factor. A continuous glucose monitor remains on the skin for 10–14 days, noting glucose levels every five minutes. The monitor sends that data to a smartphone, which allows highly personalized diagnosis and treatment.
It’s yet another example of the MDEC:
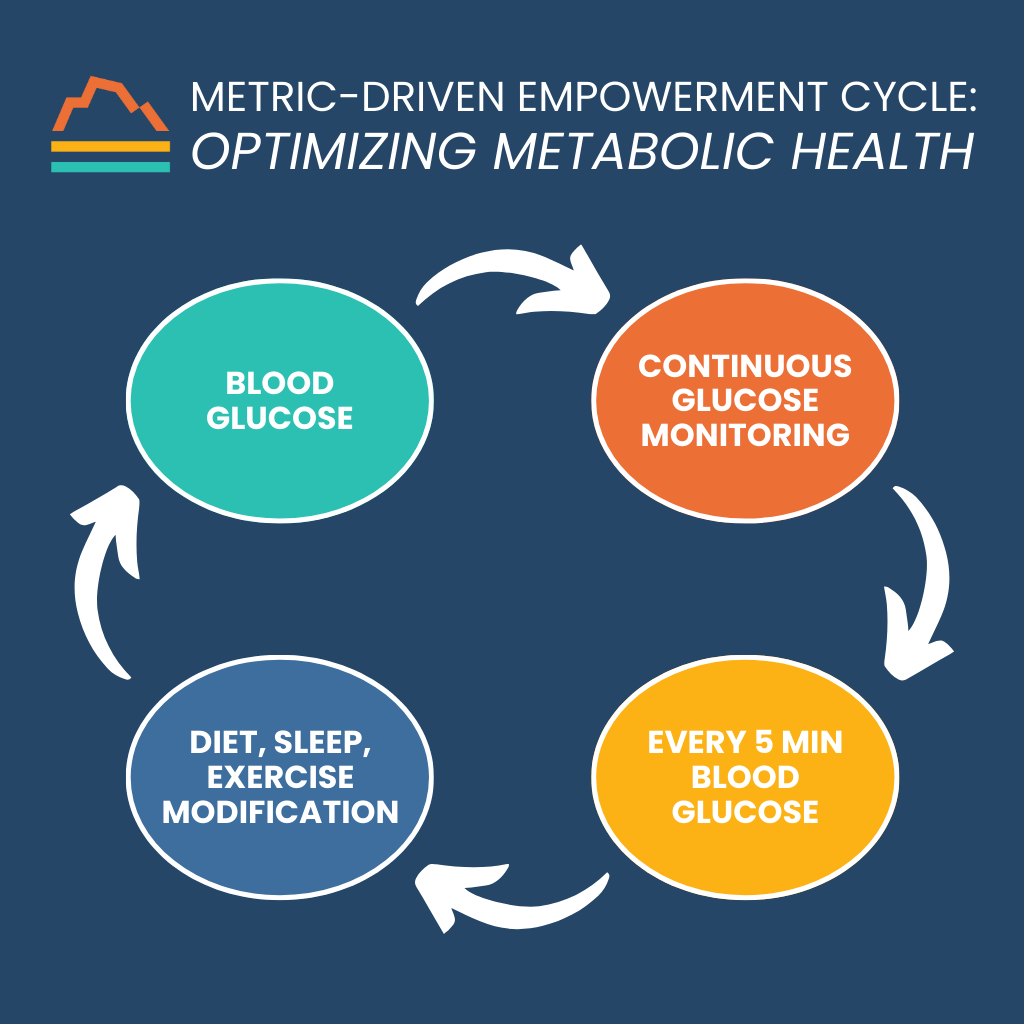
Final Thoughts
The Metric-Driven Empowerment Cycle provides a new paradigm of care at Banner Peak Health. Now, we can offer the highest quality of care for our patients: medical care that prioritizes prevention and empowers patients by blending the latest medical technology with an old-fashioned determination to work hard.
We want patients to live longer and better!