The Ultimate Workout: How Rowing Machine Benefits Transform Your Fitness
The other day, a patient asked me about the most efficient means of exercise for someone with limited time and joint issues. Without hesitation, I recommended a rowing machine.
The benefits of rowing machines include comprehensive muscle engagement, cardiovascular improvements, joint protection, maintenance of spinal bone density, and mental wellness, making rowing ideal for almost anyone.
Top Rowing Machine Benefits: A Full-Body Workout
When evaluating any exercise, I first consider muscle engagement.
One of the primary benefits of rowing machines is that they engage 86% of your muscles simultaneously. The arms, legs, back, and core all work together in a synchronized motion that few other exercises can match.
Let’s compare muscle engagement across different activities:
- Walking: Engages only 30–40% of muscle groups, primarily lower body
- Cycling: Activates 40–50% of muscle groups, mainly legs with some core
- Running: Uses 60–70% of muscle groups with upper body involvement
- Swimming: Engages 80–90% of muscles, approaching rowing’s effectiveness
- Rowing: Tops the list at 86% muscle engagement
Swimming comes close to rowing in terms of full-body engagement, but it’s much easier to fit a rowing machine in your basement than install a swimming pool.
This comprehensive muscle recruitment makes rowing time-efficient. Rather than isolating muscle groups across different exercises, rowing engages nearly everything at once.
Another benefit of rowing machines is their low-impact nature, which is advantageous for individuals with joint issues. Unlike running or jogging, which pound your knees against pavement, rowing offers resistance without impact stress. Your joints move through their natural range of motion without the trauma of repeated impact.
Cardiovascular Benefits of Rowing Machines
The cardiovascular benefits of rowing machines deserve special attention. I particularly appreciate rowing’s adaptability to different training zones.
Want a steady Zone 2 cardio workout that builds endurance? Row at a consistent, moderate pace using a heart rate of power output to keep you in Zone 2.
Prefer high-intensity interval training? Alternate between sprint efforts and recovery periods.
Need a tempo workout? Find that middle ground with sustained challenging effort.
The rowing machine adapts to your cardiovascular goals, making it versatile for different training phases and fitness levels.
Mental Benefits: Another Advantage of Rowing Machines
Like most forms of exercise, rowing relieves stress and boosts mental well-being.
Rowing’s rhythmic nature puts many people in a peaceful state. I’ve had numerous patients report that their rowing sessions become a form of moving meditation, clearing their minds while strengthening their bodies.
Posture and Core Strength: The Hidden Rowing Machine Benefits
We live in an increasingly sedentary society. The resulting epidemic of poor posture contributes to numerous chronic pain issues.
The many benefits of rowing machines include strengthening your upper back, spine, and core muscles, which support proper posture. This strengthening protects your back from injury and improves how you stand and position your body throughout the day.
The strong core development from consistent rowing translates to better body mechanics in all daily activities.
The Solo-Community Balance
For home workouts, rowing machines are remarkably space-efficient. A single machine tucked in a corner provides a complete fitness solution.
Meanwhile, group rowing classes provide motivation, instruction for proper technique, and the social benefits that often help maintain exercise consistency.
This balance between solo exercise and community involvement makes rowing adaptable to different personality types and lifestyles. Whether you prefer solitary exercise or thrive in group settings, rowing accommodates your preferences.
Proper Technique: Maximizing Rowing Machine Benefits
Proper technique remains essential for maximizing rowing’s benefits while minimizing injury risk.
The best approach to learning proper rowing technique is working with an expert who can observe your form and provide real-time corrections. Video tutorials are a good starting point, but nothing replaces personalized instruction.
To that end, I’m excited to announce that Banner Peak Health will partner with CRUfit, a specialized rowing gym. This partnership will give our members access to expert instruction and a supportive community to enhance their rowing experience.
Today’s Takeaways
If exercise were a pill, it would be the safest, most powerful drug ever created. And if exercises were ranked by efficiency and effectiveness, rowing would be near the top of that list.
If you have limited time, joint concerns, or a desire for maximum efficiency in your workout routine, explore rowing as a primary exercise modality. The benefits of rowing machines include unparalleled muscle engagement, joint protection, cardiovascular adaptability, and mental wellness.
Whether you’re just beginning your fitness journey or looking to optimize an established routine, few other exercises can match the benefits of rowing machines. Your heart, muscles, joints, and mind will all thank you for giving rowing a try.
Benefits of Continuous Glucose Monitoring: My Journey With Stelo CGM
I see them everywhere — small white dots on triceps at the gym, the beach, and even medical conferences. Continuous glucose monitors have become the latest health trend, with Dexcom’s new over-the-counter Stelo leading the charge.
As a physician committed to preventative health, I embrace “me-search” — using myself as a subject in N=1 trials to better understand the latest healthcare technologies.
My latest experiment? Testing Stelo for myself to understand the benefits of continuous glucose monitoring (CGM).
The Metric-Driven Empowerment Cycle
Human nature drives us to improve what we measure. When we assign a number to something, we try to beat it. The Metric-Driven Empowerment Cycle (MDEC) leverages this tendency to create lasting health improvements.
Let’s break it down:
- Metric — The quantifiable number that measures your current state.
- Driven — The motivation to improve that number.
- Empowerment — The active process of making changes. You have the power to change these numbers — this isn’t passive.
- Cycle — This isn’t a one-time measurement but a repeating process. You measure, improve, and feel accomplished, which motivates you to continue.
We see this cycle in action every day. My wife tries to take 10,000 steps a day. Patients step on our scale, motivated by the number they see. These metrics create measurable paths toward improvement.
This cycle is particularly powerful when combined with the benefits of continuous glucose monitoring, as CGM provides immediate feedback that drives behavior change.
Why I Tried Stelo CGM
With borderline glucose levels in my own tests (fasting glucose of 104–106 and A1c of 5.6), I was a perfect candidate for Stelo.
While my numbers fell within the “normal” range, they sat at the upper boundary. Research shows cardiovascular risks begin increasing at A1c levels as low as 5.4 — meaning a population with “high-normal” results still faces health risks.
Until recently, CGMs required prescriptions. Dexcom previously manufactured only the G7 device (prescription only) but now offers Stelo for over-the-counter purchase, with key differences:
- Stelo lasts 15 days (G7 lasts 10).
- Stelo reads glucose levels every 15 minutes (though my device gave five-minute readings).
- Stelo reads glucose levels between 70–250 mg/dL (G7 ranges from 40–400).
- Stelo targets pre-diabetics or those wanting to optimize metabolic health.
From Static to Dynamic Health Monitoring
Traditional testing offers a snapshot — a single moment frozen in time. Consider the difference between an EKG and a stress test. One shows a photo; the other displays the whole movie.
One of the key benefits of continuous glucose monitoring is the shift from static to dynamic measurement. While traditional glucose monitoring only provides occasional snapshots (e.g., finger-stick tests, which show your level at one moment), the benefit of continuous glucose monitoring is that it reveals how your body responds to food, stress, sleep, and exercise in real time.
Over 100 million Americans have either diabetes or pre-diabetes, and most don’t know it. One study examined 60 individuals who tested normal through traditional measurements. When evaluated with CGM, 25% showed pre-diabetic patterns.
My Stelo Me-Search Findings
Stelo attaches to the back of your arm — the visible dot that’s becoming common — and pairs with a smartphone app. I learned a lot:
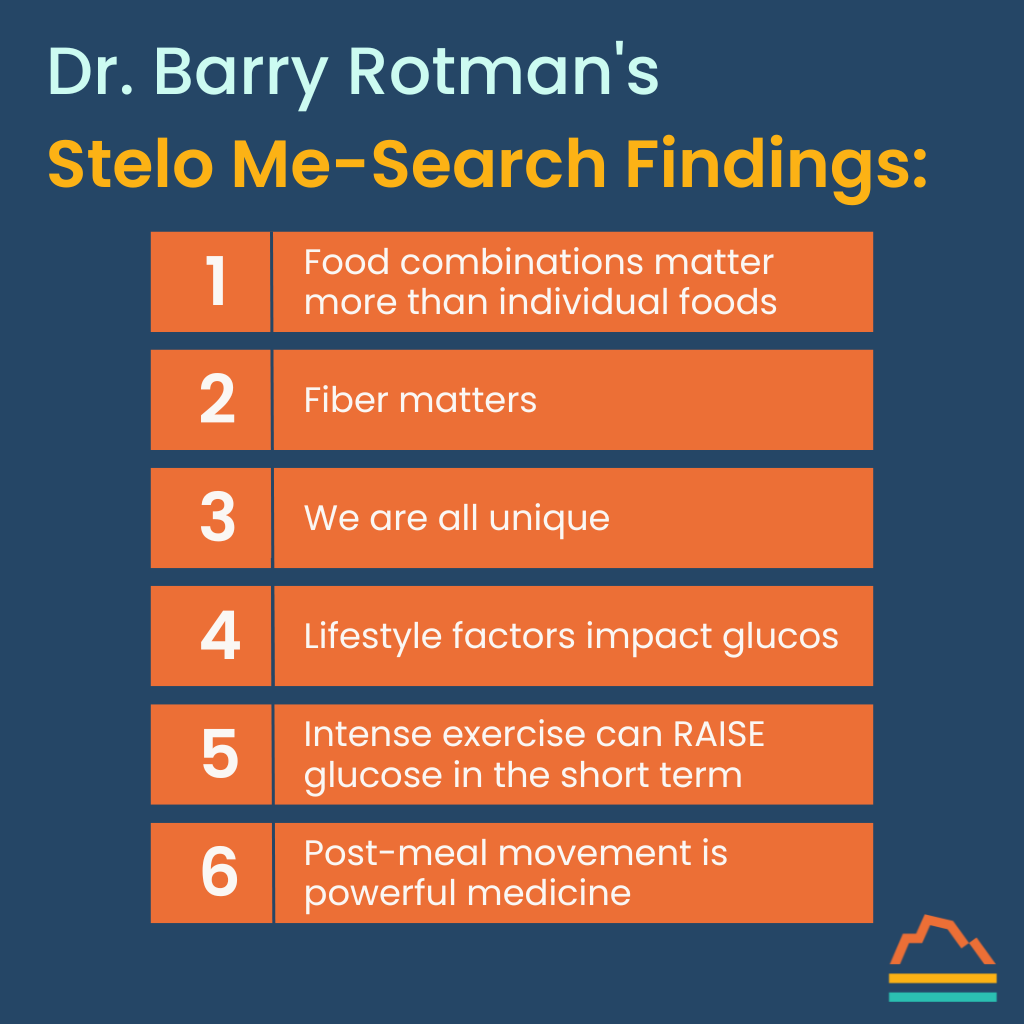
1. Food combinations matter more than individual foods
The glycemic index, describing how much blood sugar rises with each food, is inadequate in that it fails to account for what other foods are consumed at the same time. I tested this directly by eating my favorite dessert (halva, a Middle Eastern sweet made from glucose and sesame) on an empty stomach, causing a dramatic glucose spike. Eating the same treat after a meal produced a much smaller increase. Protein, fat, and fiber slow glucose absorption, dampening spikes.
2. Fiber matters
For example, apples and apple juice create different glucose responses. The fiber in whole fruit slows absorption and reduces spikes. I wore my Stelo during the Jewish holiday of Passover and followed the tradition of eating matzah, unleavened flatbread. The white matzah is made from refined wheat with less than one gram of fiber per piece. These shot my glucose up way higher than the whole wheat variety with 3 grams per piece.
3. We are all unique
The glycemic index also fails to account for individual variation. Yes, certain sugar-containing foods, especially beverages, will spike nearly everyone’s serum glucose. However, each of us processes our own response to different foods. My blood sugar response to a banana may not be that of yours.
4. Lifestyle factors impact glucose
Family stress elevated my glucose levels even with identical food intake. Sleep deprivation similarly increased my numbers. During a recent flight, the call went out for a doctor on the plane. I volunteered and assisted a young man who had fainted. My Stelo logged a spike beginning the exact moment of the call. Our metabolic health responds to everything, not just what we eat.
5. Intense exercise can RAISE glucose in the short term
Overall, exercise is one of the best methods for improving metabolic health. I was surprised to see elevations above the normal range during maximum biking efforts. The body’s hormonal efforts to provide enough energy for intense exercise can transiently raise the blood sugar until it is utilized by the muscles.
6. Post-meal movement is powerful medicine
After one lunch that raised my glucose levels, I took a walk. My numbers dropped by half in less than 30 minutes.
This dramatic response visually confirmed that walking after meals improves glucose control — 80–90% of glucose goes to muscles, so movement accelerates this process.
These insights demonstrate the comprehensive benefits of CGM for understanding personal metabolism. Continuous glucose monitoring reveals patterns that occasional blood tests could never detect, empowering users to make informed health decisions.
The Stelo App Experience
The Stelo app connects with Dexcom’s Clarity platform, allowing patients and physicians to analyze patterns and correlations. We can examine time in target range, daily patterns, and specific responses to foods or activities.
The note-keeping feature lets you record what you ate, stressful events, or exercise, creating a picture of your metabolic health.
Why Banner Peak Health Embraces Stelo
At Banner Peak Health, we look for nooks and crannies of cardiovascular risk that conventional medicine often misses. Insulin resistance is a significant yet often-overlooked risk factor we can now identify and mitigate, lowering the risk for atherosclerosis as well as progression to diabetes.
The benefits of continuous glucose monitoring are now a powerful tool for preventative medicine, even in non-diabetics — not just treating disease but preventing it through real-time feedback and targeted lifestyle modifications.
Today’s Takeaways
You don’t know something until you experience it yourself. My time with Stelo taught me more about my metabolic health than years of occasional blood tests.
As those little white dots become increasingly visible on arms everywhere, consider adding your own. The benefits of glucose monitoring could change your understanding of your body and empower you to make more informed health decisions.
Carpal Tunnel Syndrome Medical Devices: Your Guide to Treatment Options
In certain circles, evolution is described as just one theory among many explaining life on our planet. A prominent alternative is intelligent design — the idea that certain features are too complex to have arisen gradually through evolution.
I’m a firm proponent of evolution, the bedrock of modern biology. The human body offers many examples of features that function poorly, which would be products of unintelligent design.
Consider the human spine. Who would place weight-bearing support so close to our neural wiring? The wear and tear creates degradation of our spine and distorts our bones and discs, leading to pinched nerves. The millions suffering from sciatica would disagree with anything intelligent about this arrangement.
The carpal tunnel — and the need for carpal tunnel syndrome medical devices — represents another design flaw. There’s too much happening in too small a space.
This guide explores the most effective carpal tunnel syndrome medical devices available today, from ergonomic tools to specialized splints, helping you understand which options best suit your needs. But first, understanding how these devices work requires knowledge of the condition’s underlying causes.
What Is Carpal Tunnel Syndrome?
The carpal tunnel is a tiny space where your hand meets your wrist. The bottom consists of four small wrist bones. The top is the flexor retinaculum, a stiff ligament. Inside this space are nine flexor tendons that facilitate curling movements of your fingers and thumb — plus one little median nerve.
This median nerve controls thumb movement and sensation to the thumb, index, middle, and half the ring finger.
On a good day, there’s barely enough room for everything to function properly. Many factors can cause a bad day for your carpal tunnel. Because it’s surrounded by inflexible structures (bones and ligaments), anything causing swelling increases pressure within the tunnel and compresses the median nerve.
Signs and Symptoms of Carpal Tunnel Syndrome
When the median nerve gets compressed, several symptoms can occur:
- Numbness or tingling in the thumb, index, middle, and part of the ring finger
- Pain in the same distribution
- Weakness that makes gripping objects difficult
- Dropping things frequently
- Reduced thumb function
These issues interfere with daily tasks like writing, opening jars, and brushing your hair.
Many patients notice symptoms worsen at night. Why? When we sleep, we lose conscious control of our muscles. Our default state curls our wrists forward, further compromising the already cramped tunnel.
Understanding Carpal Tunnel Syndrome’s Root Causes
Before discussing carpal tunnel syndrome medical devices, we must consider underlying causes. Many conditions increase risk:
- Wrist trauma (fractures, dislocations, sprains)
- Inflammatory conditions (rheumatoid arthritis, lupus)
- Hormonal changes (pregnancy, menopause, oral contraceptives)
- Fluid retention (medication side effects, sodium intake)
- Hypothyroidism
- Obesity
Other conditions don’t increase swelling but make the median nerve more susceptible to damage:
- B12 deficiency
- Alcohol abuse
- Diabetes
A careful practitioner explores these underlying causes before recommending treatment.
Ergonomic Factors
Contrary to popular belief, typing itself doesn’t cause carpal tunnel syndrome. Studies show frequent typists don’t have higher incidence rates, likely because they’ve optimized their ergonomics.
It’s not typing frequency but wrist position that matters. Deviation from a neutral position (wrists flexed downward or upward) causes problems.
Think of your carpal tunnel as a straw packed with nine tendons and one nerve. When you bend your wrist, you kink that straw.
Other ergonomic risk factors include:
- Using vibrating machinery
- Exposure to extreme cold
- Poor bicycling ergonomics (gripping the handlebar, putting pressure on the carpal tunnel)
Carpal Tunnel Syndrome Medical Devices and Treatment Options
Treatment follows a progression from conservative to more invasive approaches:
1. Address Underlying Conditions
Identify and treat any underlying medical issues like B12 deficiency, diabetes, or hypothyroidism.
2. Ergonomic Assessment and Modification
Evaluate how you use your hands during daily activities:
- Keyboard height (ensuring neutral wrist position)
- Mouse design and positioning
- Proper equipment for occupational tasks
Specialized carpal tunnel syndrome medical devices include ergonomic keyboards, mouse pads with wrist support, and task-specific tools designed to maintain neutral positioning.
For cyclists, specialized gloves with padding on either side of the carpal tunnel create a groove that prevents direct pressure on this sensitive area.
3. Night Splinting
Since symptoms often worsen at night, wearing a neutral position wrist splint while sleeping can provide the canal enough time to straighten and heal. These carpal tunnel syndrome medical devices prevent your wrists from curling during sleep.
4. Day Splinting
If night splinting proves insufficient, wearing splints during daytime activities for four to six weeks may help. Modern carpal tunnel syndrome medical devices include flexible braces that allow some movement while maintaining neutral alignment.
5. Steroid Injections
When conservative measures fail, a physician can inject steroids to reduce inflammation around the median nerve.
6. Surgical Decompression
As a last resort, surgical release of the transverse carpal ligament creates more space in the tunnel.
Today’s Takeaways
Carpal tunnel syndrome stems from a design flaw in human anatomy, but proper management can prevent or resolve symptoms. Remember:
- Maintain neutral wrist position — don’t kink the straw.
- Consider whether underlying medical conditions might be contributing to your symptoms.
- Start with the least invasive carpal tunnel syndrome medical devices (ergonomic tools, night splints) before progressing to more aggressive treatments.
At Banner Peak Health, we evaluate every aspect of your health when addressing carpal tunnel syndrome. Rather than simply recommending carpal tunnel syndrome medical devices, we first identify and treat the root causes of your symptoms. If a medical device is necessary for your specific carpal tunnel situation, we’ll help you choose the one most appropriate for you.
Zone 2 Training Benefits: The Complete Guide to Metabolic Health and Performance
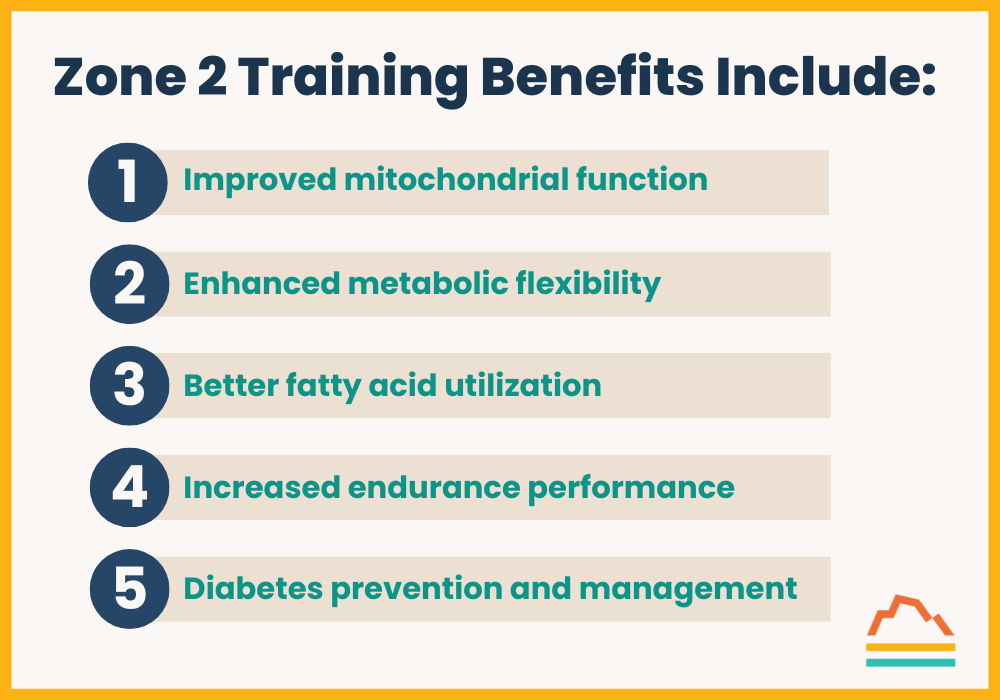
Zone 2 training benefits include:
- Improved mitochondrial function
- Enhanced metabolic flexibility
- Better fatty acid utilization
- Increased endurance performance
- Diabetes prevention and management
While it’s common knowledge that exercise is good for you, the specific advantages of Zone 2 training are less understood. In this comprehensive guide to Zone 2 training benefits, we’ll explore:
- How Zone 2 training transforms your body’s energy systems
- The optimal “dose” of Zone 2 training for maximum benefits
- How to measure and track your Zone 2 training progress
- The scientific evidence behind Zone 2 training benefits
The intensity of cardiovascular exercise can be divided into zones, ranging from no exertion to complete exhaustion. While there are various training zones, Zone 2 stands out for its unique benefits and powerful effects on metabolic health.
Let’s explore why Zone 2 training has become a cornerstone of both elite athletic performance and metabolic health improvement.
Understanding Zone 2 Training Benefits: The Science Behind Cardiovascular Exertion
I’m a huge fan of the Tour de France bike race. Two hundred of the world’s best bike riders pedal over 2,000 miles in three weeks. The competition is so intense that after scores of hours of racing, the top three finishers may be only minutes, or even seconds, apart.
As a recreational bicyclist, I’m fascinated by the bike handling skills and tactics of racing. As a physician, I’m awestruck observing the best endurance athletes on the planet.
Even among the world’s best riders, there are once-in-a-generation athletes. Tadej Pogacar, a Slovenian, won his first Tour de France at 21, the youngest champion since 1904. He won the Tour in 2020, 2021, and 2024.
Watching Tadej take off up a mountain, leaving behind the world’s best riders, is awe-inspiring. In addition to winning the one-in-a-billion genetic lottery, Tadej trains with Dr. Inigo San Millan, a top sports physiologist and coach.
Dr. San Millan raced as an amateur cyclist in the Basque region of Spain before earning a medical degree. He is now a research scientist at the University of Colorado in Boulder.
In addition to sports physiology, Dr. San Millan’s research focuses on metabolic disorders. Much of his work focuses on mitochondrial function, which is prominent in metabolic disorders and sports physiology.
In “Outlive,” Peter Attia cites a 2017 study by Dr. San Millan and George Brooks, which describes the foundational ideas behind Zone 2 training. The authors examined the mitochondrial function of three groups: world-class cyclists, recreational cyclists, and inactive people with pre-diabetes or diabetes.
By comparing how mitochondria function in the world’s best endurance athletes as opposed to diabetics, the study sheds light on metabolic flexibility — what fuel sources the mitochondria can “burn” for energy.
The Metabolic Benefits of Zone 2 Training: Energy Systems Explained
A brief discussion of energy metabolism biochemistry will help us understand Dr. San Millan’s study.
The mitochondria consume either fatty acids or glucose to produce energy. Fatty acids are the preferred fuel source. They have twice the energy density of glucose, 9 kcal/gram, compared to 4 kcal/gram.
Thus, a kilogram of fat (2.2 lbs) provides approximately 9,000 kcal of energy. The average person has many kilograms of fat, which can be mobilized for energy, providing a vast “gas tank.”
In contrast, the body’s storage of glucose in the form of glycogen is limited to around 600 grams, or approximately 2,400 kcal of energy — less than the energy from a quarter of a kilogram of fat. Food sources provide additional glucose, but the digestive system can’t effectively absorb many nutrients during intense exercise.
The liver produces glucose through a process known as gluconeogenesis, but it has a limited capacity and isn’t as energy-efficient as other fuel sources. Gluconeogenesis doesn’t contribute much energy for exercise but prevents low blood sugar during low food intake.
Not only are fatty acids a more plentiful and efficient fuel source for exercise, but their combustion byproducts are also “cleaner” than glucose ones.
Glucose metabolism generates lactic acid, which contains a lactate molecule and a hydrogen ion. Lactic acid has been described as the “bad” waste product from exercise. For example, we used to think that after an intense workout, your thighs burned because of lactic acid buildup.
This is only partially true.
The lactate molecule is beneficial, functioning as an energy source that adjacent muscle cells can consume. The associated hydrogen ion remains a bad factor, lowering the pH in the region and impairing further muscle functioning. The hydrogen ions from glucose metabolism generate a ceiling on muscular energy production’s quantity and duration. In contrast, fatty acids burn cleaner, generating only carbon dioxide and water.
However, the body’s ability to metabolize fatty acids has a finite capacity. With increased energy demand, the systems available to metabolize fatty acids become saturated. Less efficient glucose metabolism is recruited and added to fatty acid consumption to increase energy production further.
Back to the Study...
Inigo San Millan and George Brooks wanted to explore how efficiently each group of people used fatty acids, the preferred fuel source, before using glucose.
Each participant rode an exercise bike with a step-up protocol requiring progressively more power output every 10 minutes. At each step, each participant’s oxygen consumption, carbon dioxide production, power production, and serum lactate levels were recorded.
By analyzing this data, the researchers could calculate the composition of fuel sources used at each power level. For example, because lactic acid is a metabolite of glucose but not fatty acids, it would remain in the low range at lower power levels when fatty acids were the predominant fuel and climb at higher levels as more glucose was used.
Each participant started with more fatty acids burned than glucose. As power increased, additional glucose was consumed, and the percentage of fatty acids burned became smaller.
However, the key finding was the vast differences between the study groups.
The world-class cyclists produced staggering amounts of power while maintaining a stable serum lactate level, meaning they were extremely efficient at burning fatty acids and processing any lactate generated from the glucose they burned. They possessed the best mitochondria on the planet, derived from fortunate genetics and effective training regimens. (More on that topic later.)
In contrast, the deconditioned participants with pre-diabetes or diabetes had the opposite response. These participants had higher lactate levels at rest than the world-class cyclists had while producing large amounts of power. Even before exercising, these participants couldn’t readily access fatty acids and had to rely on glucose, which produced lactic acid.
With minimal exercise, the hydrogen ions from the lactic acid began rapidly building up and limiting exercise duration. This process drastically limited their power — a small fraction of the world-class cyclists. The recreational cyclists had outcomes between these two extremes.
Zone 2 Training Benefits: Evidence From Clinical Research
So, what explains the pre-diabetic and diabetic participants’ results?
Metabolic syndrome — the process of insulin resistance and other hormonal dysfunction that leads to pre-diabetes and potentially diabetes — degrades mitochondrial function through various mechanisms, such as fewer mitochondria and fewer proteins within each mitochondria. These processes limit the ability to metabolize fatty acids and effectively generate power for exercise.
Fortunately, these changes are reversible.
Zone 2
How does the study relate to Zone 2?
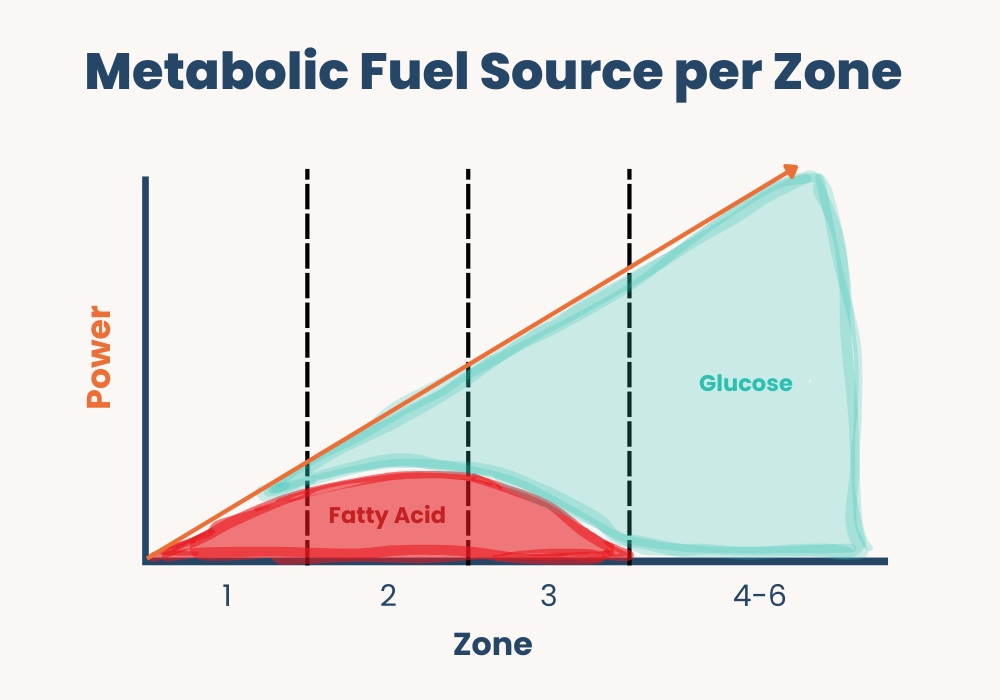
Dr. Inigo San Millan defines zones based on the body’s fuel source.
- Zone 1: An intensity that allows mitochondria to use fatty acids but doesn’t exceed their capacity.
- Zone 2: The intensity that maximizes mitochondrial fatty acid utilization for power.
- Zone 3: Occurs when the power requirements exceed the mitochondrial capacity for fatty acid utilization and progressively more glucose utilization is required.
- Zone 4–6: The mitochondria no longer use fatty acids and are defined by other energy sources.
The study has profound implications for athletic training and improving the metabolic health of pre-diabetics and diabetics.
Dr. Inigo San Millan’s training regimen for Tadej Pogacar involved more time in Zone 2 than in any other zone. For Tadej Pogacar to become one of the world’s fastest endurance athletes, he had to spend lots of time biking relatively slowly.
What Is Zone 2?
Zone 2 is the optimal training zone for maximizing endurance and metabolic benefits. It’s characterized by a level of exertion where you can still hold a conversation, typically described as an “all-day” pace. This sweet spot of intensity is where the most powerful Zone 2 training benefits occur.
Zone 2 training intensity improves mitochondrial function by increasing the number and efficiency of mitochondria in muscle cells. In particular, it enhances metabolic flexibility, which maximizes the mitochondria’s consumption of fatty acids for fuel.
As we discussed, fatty acids are the preferred fuel because:
- The body has tremendous fatty acid storage.
- Fatty acid consumption burns cleanly, with no negative feedback loop blocking its metabolism.
- Fatty acid provides a foundation for further levels of metabolism.
Zone 2-enhanced mitochondrial ability allows athletes to go farther more efficiently and reach a higher peak output. Once the power requirement exceeds the mitochondria’s ability to metabolize fatty acids, the body relies on less efficient and more time-limited substrates, such as glucose.
I think of Zone 2 as the booster stage of a multistage rocket ship. The faster and farther it moves the rocket, the less the rocket relies on smaller subsequent stages.
In prior blogs, I’ve discussed the value of measuring VO2 max at peak output, noting that it measures the ability of the entire cardiopulmonary system to function. Zone 2 training at lower intensity provides the foundation that supports other energy systems that allow the body to reach peak output. A massive booster rocket gets you into the sky faster and farther.
Paradoxically, you must go slow to get fast. This is Dr. San Millan’s message and the secret to Tadej Pogacar’s success.
This message has been lost on recreational athletes, who, like me, have limited time for training and assume they should “go hard” whenever possible. Workout apps like Garmin and Strava reinforce this ethos with features to set new personal records, measure peak power outputs, and compete against your friends.
In contrast, effective Zone 2 training requires a relatively slow and deliberate training regimen.
How to Maximize Your Zone 2 Training Benefits: Creating a Personal Program
The first step to creating a Zone 2 training program is identifying your Zone 2 parameters.
This process is more nuanced than reading the workout equipment at the gym, which identifies your “fat-burning” zone as 50–70% of your maximum heart rate. This approximation overlooks many individual characteristics.
Two more accurate techniques for identifying one’s Zone 2 include:
- Replicate the protocol Inigo San Millan and George Brooks used. Measure fingerstick lactate levels or exhaled carbon dioxide and oxygen levels to calculate how intensely you can exercise before you leave the Zone 2 region of fatty acid metabolism. This level of intensity can be expressed in terms of heart rate or power output and can serve as a guide for further workout intensity.
- Use your rate of perceived exertion (RPE), a 10-point scale from absolute rest to complete exhaustion. RPE scores your intensity assessment based largely on your breathing rate, which correlates with exertion. (Carbon dioxide and serum acidity rise with activity level, leading to more rapid breathing.) Zone 2 corresponds to an RPE of 5–6 out of 10 and has a breathing rate that allows you to speak in full sentences.
How much Zone 2 training you need depends on your goals. Professional and elite endurance athletes may spend 80% of their training time in Zone 2, which can be tens of hours a week. The minimum effective dose for us “time-crunched” athletes would be three hours a week, providing noticeable benefits without hurting professional or personal commitments. It may take several months for the maximum benefit to accrue.
Key Zone 2 Training Benefits for Elite and Recreational Athletes
Zone 2 training has become vital to elite athletes’ competitiveness. It can also provide a welcome boost for recreational athletes.
For decades, I’ve biked five to seven hours a week. Given the hilly terrain where I ride, most of that time has been spent above Zone 2 going uphill or below Zone 2 going downhill. I’ll ride in Zone 2 for three hours a week and observe its effects.
In addition to allowing athletes to enhance performance, I suspect the greatest potential benefit of Zone 2 training is improving the metabolic health of those with pre-diabetes and diabetes. We’re amid an unprecedented epidemic of pre-diabetes and diabetes, which correlates with an elevated body mass index. One in three adults in the U.S. is estimated to have prediabetes; another 38 million are fully diabetic!
Mitochondria are the key to understanding insulin resistance and metabolic dysfunction, which leads to pre-diabetes and diabetes. Skeletal muscle cells metabolize up to 90% of the body’s glucose. These cells’ metabolic health, including their mitochondrial function, impacts how the body uses glucose.
Whenever we consume more calories than we burn, we’re in caloric excess. Excess calories are converted to fat and distributed throughout the body. Some locations, such as the thighs and buttocks, have minimal health effects. In contrast, other locations, such as the liver and abdomen, create problems.
Fat deposited within muscle cells impairs mitochondrial function by inhibiting fatty acid use and glucose uptake into the cell, reducing mitochondrial density and efficiency, and creating localized inflammation. When muscle cells can no longer adequately metabolize glucose and fatty acids, glucose levels rise, creating a vicious cycle leading to pre-diabetes and, ultimately, diabetes.
This frightening process has a silver lining: The most effective treatment involves rehabilitating the mitochondria within muscle cells through Zone 2 exercise! No pill, injection, or drug effectively prevents diabetes as much as diet and exercise.
Diet modification is crucial to reverse caloric excess, which deposits fat into cells such as muscle cells and impairs their function. Zone 2 exercise is the most potent tool for improving muscle cell mitochondrial function and can reverse the metabolic effects of pre-diabetes and diabetes.
Final Thoughts on Zone 2 Training Benefits
So, in summary, the key Zone 2 training benefits include:
- Enhanced mitochondrial function and density
- Improved metabolic flexibility
- Efficient fat utilization
- Better endurance capacity
- Diabetes prevention and management
- Enhanced athletic performance
- Sustainable long-term fitness improvements
Three hours a week of Zone 2 training appears to be a good minimum dosage for improving metabolic health and athletic performance. More would be better, but even three hours can be a significant commitment.
Zone 2 training “magically” provides a performance boost to recreational athletes who’ve plateaued within a busy schedule. More importantly, Zone 2 training “magically” corrects the metabolic dysfunction that causes pre-diabetes and diabetes.
At Banner Peak Health, we’re committed to helping you experience these powerful Zone 2 training benefits. Our experts will help determine your optimal Zone 2 parameters, design a personalized training program, and monitor your progress to ensure maximum results. Give us a call and be part of the magic.
How to Lower APOB for Cholesterol Management and Cardiovascular Health
One advantage of having spent 40 years in medicine is my ability to view medical information (such as how to lower APOB) not as a new idea, but as the culmination of a concept’s long-term evolution.
Inferring coronary artery risk from serum cholesterol measurements is exactly this kind of evolving story.
The Evolution of Cholesterol Understanding
In the 1950s, Ancel Keys initiated a series of epidemiologic studies that, while controversial, introduced the connection between saturated fats in the diet, cholesterol levels in the blood, and coronary artery disease.
In the 1970s and 80s, researchers began identifying low-density lipoprotein (LDL) receptors and focused on LDL mass as a more specific risk factor.
By the 1990s, diagnostic tests involving gel electrophoresis allowed us to look at particles’ cell size. In the early 2000s, NMR spectroscopy enabled us to quantitate particle size.
This multi-decade story shows a clear trajectory — from total cholesterol quality to LDL quantity, now to the size and quantities of particles within the blood.
Our understanding of how lipid metabolism impacts atherosclerotic disease has evolved alongside the progression of tests we use to clinically measure lipids. This evolution gives context for why APOB is so important.
APOB Is More Predictive Than LDL
Cholesterol doesn’t dissolve directly into our blood but resides in different particles, such as HDL, LDL, and VLDL. Each particle has attached lipoproteins that identify the particle and enable its uptake into cells, functioning like a passport.
Why is apolipoprotein B (APOB) the most predictive blood marker of coronary artery disease risk?
- APOB resides on all particles that carry cholesterol into vessel walls and create atherosclerosis (LDL, IDL, lipoprotein(a)). It’s a more robust risk measurement than merely noting the quantity of cholesterol in LDL, which was the preferred marker for decades.
- Only one APOB lipoprotein ever resides on each particle. This provides a headcount for the total number of dangerous particles.
Understanding How to Lower APOB
Think of your arteries as a residential street and the blood vessel wall as your yard, protected by a picket fence (the endothelial lining). Atherosclerosis occurs when fat moves from the street into your yard.
With this metaphor in mind, imagine two scenarios with the same amount of fat:
- All your fat (cholesterol) is in one big wheelbarrow. Your picket fence can effectively keep it out.
- The same volume of fat is distributed in thousands of little candy wrappers that blow around. These small pieces breach the fence and dump their contents onto your lawn.
When we talk about LDL, we’re just discussing total fat mass. But how that mass is distributed determines risk. A thousand small particles carrying fat are more dangerous than a few large ones.
If I tell you your LDL is 100 mg/dL, I haven’t told you whether your cholesterol is in one wheelbarrow or thousands of candy wrappers. APOB tells you the number of particles — the higher the APOB, the more particles, and the greater your risk.
This is why knowing how to lower APOB is crucial for achieving long-term health.
How to Lower APOB: Actionable Steps
1. Get Your APOB Measured
To lower your APOB, you must first have your APOB measured. Many practices won’t offer this, but it’s part of Banner Peak Health’s standard of care.
2. Assess Your Total Risk Profile
How aggressively you need to address any one risk factor depends on your constellation of all other risk factors. Have a physician carefully evaluate high blood pressure, insulin resistance, diabetes, smoking status, physical activity level, obstructive sleep apnea, family history, and more.
Understanding your total burden of risk determines how aggressively to work on lowering APOB.
3. Target Insulin Resistance to Lower APOB
Perhaps the greatest dietary advice misdirection of the last millennium occurred in the 1980s, when the healthcare establishment promoted reducing saturated fats as the goal for heart health.
In 1987, the American Heart Association recommended total fat should be reduced to 30% of total calories. By 1990, it was federally mandated that food labels quantify saturated and total fat.
Macronutrients are a zero-sum game. We get our calories from fat, carbohydrates, and proteins. The drive to reduce total fat led to an increase in carbohydrate intake.
This shift in diet played a prominent role in an obesity epidemic and, with it, insulin resistance, pre-diabetes, and diabetes. Currently, half of all adults are either insulin-resistant, pre-diabetic, or diabetic.
How does this relate to knowing how to lower APOB? The endocrinological changes associated with insulin resistance alter how we metabolize fatty acids. Cells become dysfunctional in utilizing fatty acids, and we put more triglycerides into our bloodstream.
With diabetes and insulin resistance, we have more smaller, lipid-rich particles, which increases the risk of coronary artery disease. For the same amount of LDL, a person with diabetes will have a higher APOB.
One of the great ironies is that the link between saturated fats and atherosclerotic disease is weak and controversial, while the link between diabetes and atherosclerosis is strong and well-established.
How to Lower APOB: A Step-by-Step Guide
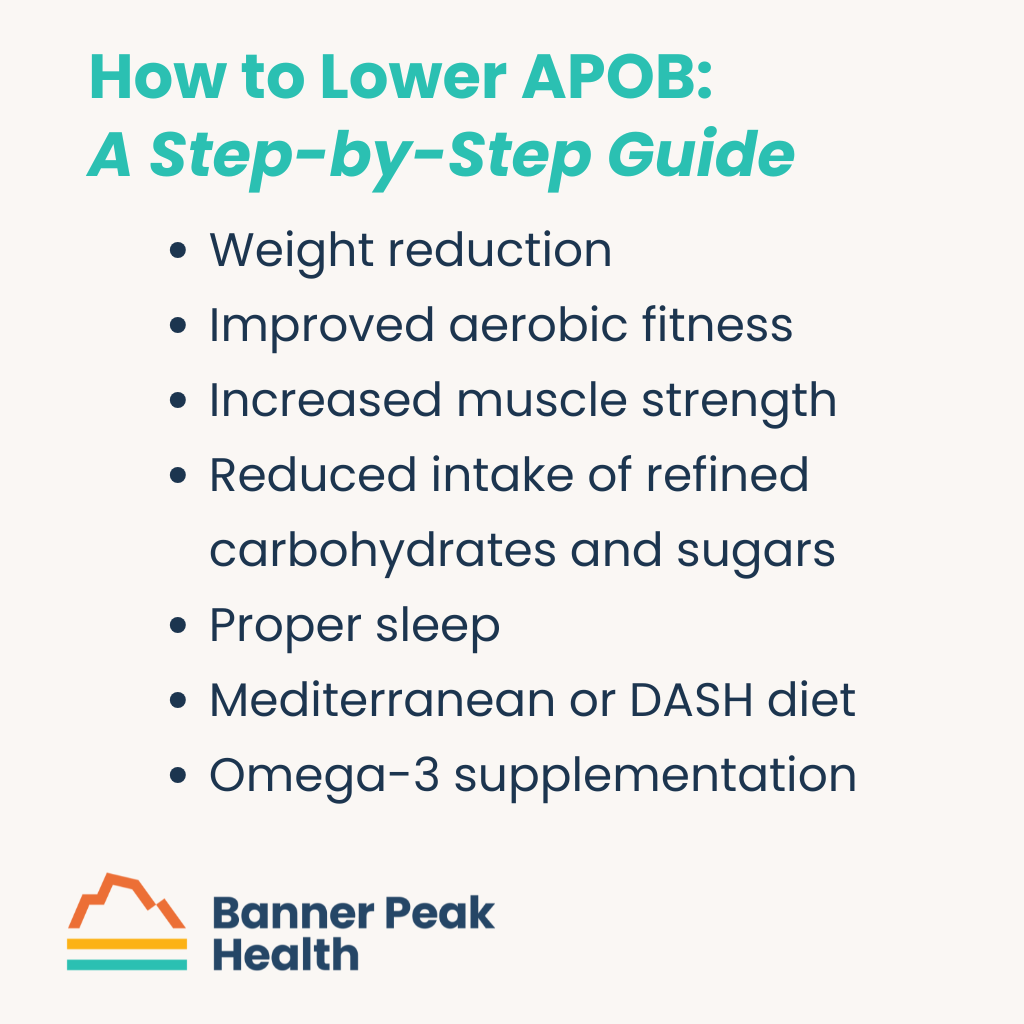
Want to know how to lower APOB? Make these lifestyle modifications:
- Weight reduction — Even modest weight loss can improve lipid profiles.
- Improved aerobic fitness — Engage in regular cardiovascular exercise.
- Increased muscle strength — Incorporate resistance training to improve metabolic health.
- Reduced intake of refined carbohydrates and sugars — Focus on complex carbohydrates.
- Proper sleep — Aim for 7–9 hours of quality sleep.
- Mediterranean or DASH diet — Embrace plant-forward eating patterns with lean proteins.
- Omega-3 supplementation — For those with borderline levels, fish oil supplements may help. (I like Nordic Naturals. They use smaller fish, which have lower mercury contamination, manufacture high-quality products, and their capsules don’t need to be refrigerated until after opening the bottle. Fish oil can degrade if stored too long in a warehouse or exposed to extreme heat during shipping, so I recommend ordering directly from Nordic Naturals — they’re careful about how they store and ship their products.)
Today’s Takeaways: How to Lower APOB
To lower your APOB effectively:
- Get it checked — you can’t manage what you don’t measure!
- Analyze your total atherosclerotic risk with your physician. Determine if medication is needed.
- Focus on lifestyle modifications that address insulin resistance — weight loss, exercise, reduced carbohydrates, and improved sleep.
The most potent lifestyle tools for lowering APOB are those that combat insulin resistance and diabetes — not necessarily reducing saturated fats. This represents a shift in how we approach heart health that many people, and even physicians, haven’t fully embraced yet.
At Banner Peak Health, we understand these nuances and are excited to develop a personalized plan to lower your APOB and reduce your cardiovascular risk. Reach out today.
Creatine Supplementation: Not Just for Bodybuilders
Recently, my best friend’s 14-year-old son presented him with a PowerPoint presentation titled “Why You Should Let Me Take Creatine Supplements.”
That’s when I knew creatine had become mainstream.
Creatine is traditionally seen as a supplement for pubescent young men eager to develop their bodies and bodybuilders aiming to look ripped. But what about the rest of us?
I looked at the research and was pleasantly surprised to discover fairly solid evidence suggesting benefits across a wide range of applications — including improved physical function in older adults and adults with chronic disease, memory enhancement, and as an adjunct to drug- and therapy-based depression treatments. (To be clear, studies didn’t show it as a stand-alone treatment for depression but as a supplement to working with a therapist and medication.)
There’s also a suggestion of benefit across many other conditions, from improving function for those with muscular dystrophy to enhancing glucose control in diabetics and improving mobility for people with knee degenerative arthritis.
What Exactly Is Creatine?
Creatine isn’t a protein, but it’s derived from three amino acids: arginine, glycine, and methionine. It plays a role in the body’s production of adenosine triphosphate (ATP), the chemical we use to move energy within our cells.
Creatine occurs naturally in animal products, and the body can manufacture some of the creatine it needs.
Taking creatine as a supplement allows the body to turbocharge its energy metabolism by enabling greater availability of ATP within cells for energy-intensive tasks. These tasks can include muscle cells lifting heavy weights or brain neurons working to consolidate memory or process complicated thoughts.
Why Muscle Mass Matters
Many young people want to improve their muscle mass for aesthetics, but as we age, the importance of preserving muscle mass goes beyond appearance.
How strong we are and how much muscle mass we have is linked to how well we preserve functional capacity and reduce fall risk as we age. We’re in the midst of an epidemic of sarcopenia — muscle mass loss. With it comes a decline in function.
Therefore, any safe, tolerable method to preserve and enhance muscle strength as we age is valuable.
How Creatine Works
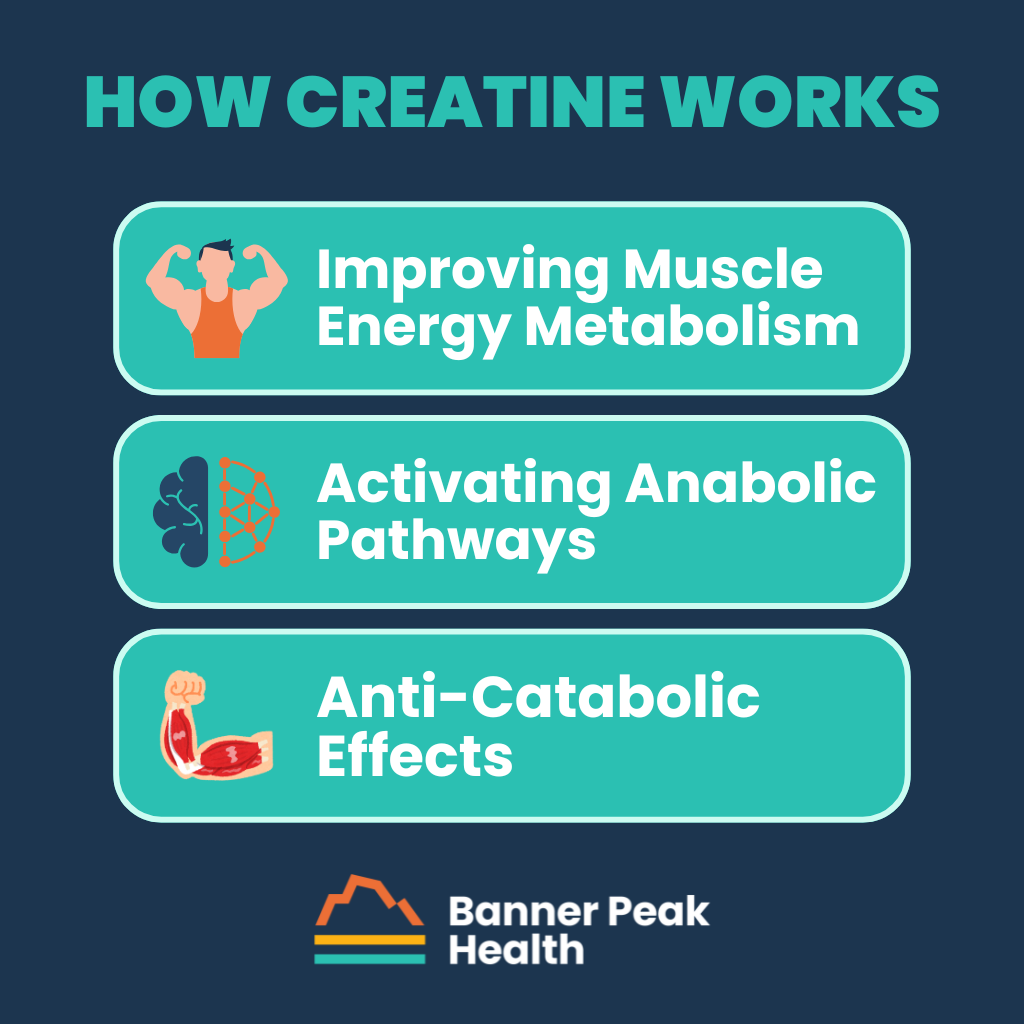
Improving Muscle Energy Metabolism
Creatine improves muscle energy metabolism.
Creatine is synthesized into phosphocreatine, which helps rapidly regenerate ATP during high-intensity exercise. This allows us to train more in terms of volume and intensity, leading to more stimulus that grows and maintains our muscles.
This improved energy metabolism also enhances mitochondrial function, the energy-generating power plants within our cells.
Activating Anabolic Pathways
Creatine also activates other signals to maintain our anabolic pathway — the whole host of hormonal signals that cause us to maintain muscle mass.
It increases other hormones such as insulin-like growth factor 1 (IGF-1) as well.
Anti-Catabolic Effects
Additionally, creatine has an anti-catabolic effect — it protects muscle from being broken down.
Besides helping young bodybuilders, creatine builds and preserves muscle mass for those of us with a bit more mileage. Reducing sarcopenia has been shown to preserve functional capacity as we age.
How Creatine Boosts Brain Health
Enhanced Brain Energy Metabolism
Just as in muscle, creatine enhances brain energy metabolism.
By providing more ATP, creatine allows greater energy access for neurons’ high-energy tasks, such as cognitive processing and memory formation.
Increased Synaptic Plasticity
Creatine has also been shown to increase signals that allow for synaptic plasticity — how many connections each neuron has, which is how our brain works.
Creatine enhances the number of synaptic connections, critical for memory and learning.
Neuroprotective Effects
Creatine also activates neuroprotective pathways, protecting neurons and brain cells from hazardous oxidative stress and inflammation.
Downsides to Taking Creatine
In healthy individuals, creatine is safe when taken at low doses (3–5 grams per day). Possible mild side effects include:
- GI upset
- Muscle cramping
- About 1–2 pounds of weight gain from greater fluid content within muscle cells
Additionally, because creatine can put a greater strain on compromised kidneys, individuals with kidney impairment or risk factors for kidney problems (such as high blood pressure or diabetes) may need to discuss creatine supplementation with their physician.
Who Should Take Creatine?
I divide supplements into three categories:
- Known risks that probably exceed benefits
- Known benefits that probably exceed risks
- Not enough data to assess the risks or benefits
For most people, creatine is in the second category. Try it and determine if it works for you. That’s what I’m doing, having recently started supplementation myself. I’ll see what happens.
Final Thoughts on Creatine Supplementation
There’s a vast array of supplements and medical devices available to consumers. Even for someone who’s been in the medical field for almost 40 years, like myself, it’s tough to separate the wheat from the chaff and determine what’s safe and worthwhile.
I can’t imagine how hard it would be for a non-medical person to figure this all out, which is why I love my job. I get to do the research and share the results with you.
The Evolution of Concierge Medicine in Walnut Creek: An 18-Year Perspective
I’ve been practicing concierge medicine in Walnut Creek for 18 years — practically since its inception in our area.
The healthcare landscape was different back then, with patients and doctors alike struggling against the constraints of traditional fee-for-service care.
The Birth of a Movement
Concierge medicine is a relatively new phenomenon, thought to have originated in Seattle in 1996. Two doctors, Howard Maron and Scott Hall, became inspired to create a small concierge medical practice after Dr. Maron’s time caring for the Seattle Supersonics NBA team.
Their insight was simple yet profound: if you can focus intensely on meeting professional athletes’ needs, why not offer the same dedicated care to others?
Ten years later, I became an early concierge medicine adopter in Walnut Creek.
A Personal Catalyst for Change
My father practiced general dentistry for over 45 years and was truly my role model — a man dedicated to practicing his craft without compromise. His passing in 2005 catalyzed my professional growth.
I realized I could no longer uphold the professional standards he had modeled for me within a traditional fee-for-service practice. This recognition inspired me to launch a solo concierge medical practice in July 2007.
At that time, I was only the second doctor in the county to take this leap. Today, after the passing of that pioneering physician, I find myself as the longest-practicing concierge doctor in the United States — the “OG” of concierge medicine in Walnut Creek.
Pioneering Challenges in Walnut Creek
Being among the first to offer concierge medicine in Walnut Creek came with two marketing challenges: educating people about concierge medicine’s value proposition and demonstrating why I should be their concierge doctor.
Many prospective patients had never heard of concierge care. Others confused it with “concierge services” in hotels. Explaining the revolutionary shift from volume-based to value-based care required patience and persistence.
Group Practice: The Next Evolution in Concierge Care
For 17 years, I practiced solo concierge medicine while observing tremendous growth in the number of other practitioners providing concierge care in our county.
In 2023, I began transitioning from a solo concierge practice to a group concierge practice, culminating in Banner Peak Health’s founding in 2024.
During this transition, I discovered the many advantages of a group concierge practice:
- Shared Knowledge: Multiple physicians collaborating creates a learning environment that enhances everyone’s knowledge and enthusiasm for practice.
- Resources and Technology: Economies of scale make evaluating and incorporating new technologies more feasible.
- Continuous Coverage: Patients always have access to a physician familiar with their medical history, even when their primary doctor takes time off.
- Team Spirit: A positive, collaborative atmosphere directly benefits patient care quality.
- Long-Term Stability: With multiple physicians, patients enjoy continuity of care beyond any single doctor’s career.
The group practice model allows us to maintain the personalized care that defines concierge medicine while adding the strength that comes from a coordinated team. Our philosophy is simple but powerful: happy staff and physicians lead to happy patients, ultimately creating better health outcomes for everyone.
Concierge Care’s Changing Landscape
Reflecting on the past 18 years, I’ve observed significant evolution in concierge medicine in Walnut Creek.
Many locals have noticed that traditional fee-for-service medical care can unfortunately no longer meet their needs. With this realization has come sustained and ongoing growth in demand for concierge medical services.
Simultaneously, more physicians have recognized the constraints of fee-for-service medicine can’t meet their standards of healthcare excellence. The increasing number of concierge practices gives patients more options, but it also makes it imperative for patients to be discerning in their choice of practice — and for us at Banner Peak Health to continue evolving and innovating.
The Future of Concierge Medicine
I believe concierge medicine will continue the trend we’ve pioneered at Banner Peak Health: physicians moving from solo practice to group concierge practice.
This evolution reminds me of the automotive industry’s development. When Henry Ford produced the Model T in 1914, it was famously available in “any color you want, as long as it’s black.” Fast forward over 110 years, and today’s automotive market offers endless customization options.
This diversification didn’t happen by chance. Market forces naturally lead to greater specialization and niche offerings as providers seek to better meet consumer demands. What began as a one-size-fits-all product evolved into customized solutions for different preferences and needs.
Similarly, concierge medicine represents this same market-driven evolution in healthcare. Fee-for-service medicine is the Model T — one standard approach to care. But now that we’re in the concierge medicine market space, practices are developing specialized niches and service structures to address specific patient populations and healthcare concerns.
Banner Peak Health is part of this continued evolution, where practices innovate and find new ways to satisfy patients’ healthcare needs. Some practices may emphasize cutting-edge technology, others preventative care, and still others specialized treatment approaches — all representing natural diversification that comes with a maturing market.
How to Choose a Concierge Practice That’s Right for You
Considering concierge medicine in Walnut Creek? Let these questions guide your search for the ideal concierge physician:
- Does medical innovation occur?
- Is there multigenerational knowledge transmission?
- Does the practice have economies of scale for new techniques and equipment?
- Is there team spirit and a supportive environment?
- Will there be continuity in your care as physicians retire?
As our county’s oldest concierge medicine practice, Banner Peak Health embodies the advantages of experience combined with an eye toward the future. We’re proud to lead the next generation of concierge care, combining the personalized attention patients deserve with group practice’s collaborative advantages.
I’m excited to see where the next 18 years of concierge medicine will take us.
Effective Lower Back Stretches and Exercises to Beat Pain
Unfortunately, lower back pain isn’t rare. A CDC study from 2019 showed that 39% of adults experienced some form of back pain in the prior three months, and an NIH document from 2023 revealed that 8% of Americans suffer from high-impact chronic pain (HICP).
The range of lower back pain is vast, from soreness after an exuberant workout to complete disability, which is why we need a structured approach to thinking about and addressing it.
Pain Is Sending You a Message
Pain sends you a message, and you need to open your mail. Lower back pain falls into three categories:
- Some potential anatomical issue in your back
- Impaired strength or flexibility in your back
- Ergonomics — how you’re using your back may be off
This framework gives us a clear path forward:
- Rule out anatomical problems
- Modify your ergonomics to reduce the burden you place on your back
- If lessening the burden isn’t an option, strengthen your back to meet the burden you place on it
1. Rule Out Anatomical Problems
Many people believe the more their back hurts, the more they need imaging like an MRI. That’s not necessarily the case. There are evidence-based guidelines for what kind of radiologic imaging is needed and when.
Red flags that necessitate anatomical imaging include:
- Recent significant trauma or mild trauma in older individuals
- Pain or numbness radiating down an arm or leg
- Changes in bowel or bladder function
- History of cancer
- Worse pain at night or at rest
- Associated fevers, chills, or unexplained weight loss
- History of inflammatory joint diseases
- Pain lasting more than six weeks despite conservative treatment
If any of these red flags are present, imaging is recommended. Work closely with your physician to determine the appropriate next steps.
2. Modifying Your Ergonomics
Most of us spend the majority of our day sitting. How we sit is very important for our back health.
Here are some basic ergonomic modifications:
- Use a chair that supports your lower back.
- Adjust chair height so your feet rest flat on the floor.
- Use armrests that gently support your arms with elbows close to your body.
- Position your seat so your thighs are parallel to the floor.
- Consider a lumbar roll or cushion to support the natural curve of your lower back.
- Keep your computer screen at eye level to avoid neck strain.
- Sit close to your desk so you’re not hunching forward.
- Keep your elbows at 90 degrees when using your keyboard.
- Consider using a standing desk to alternate between sitting and standing.
- When lifting objects, use your thighs, not your back.
These are just a small set of ergonomic modifications — examples of the kind of thought you need to give activities you do for many hours each day.
3. Boosting Back Strength and Flexibility
Strength and mobility enhance how we interact with the world, making everyday tasks easier. They prevent future painful episodes and reduce existing pain.
By addressing lower back pain syndromes properly, we reduce the risk of what I call the “sad triad” — pain leading to sleep impairment, which leads to emotional impairment. When we strengthen our backs, we don’t just address pain — we bolster our overall well-being.
Effective Lower Back Stretches and Exercises
Incorporating back-strengthening exercises and stretches for lower back pain into your routine can improve your overall health, prevent injuries, and help you maintain better posture.
How do I answer the question of which lower back stretches are best for you? The options available online, in fitness classes, or with trainers are endless. I return to my basic advice that applies to all exercise: the best exercises are what you’ll continue to do that won’t get you injured.
For some, a class setting incentivizes exercise that might not be done independently. In that case, yoga, Pilates, a fitness class, or a personal trainer could be the best route. For others, the convenience and simplicity of home exercise is best.
A Note on Using Exercise Equipment for Lower Back Pain
Some people incorporate free weights and machines into their back exercise. However, the risk-benefit ratio for most people is not advantageous unless you’re already very experienced and have been trained with meticulous technique.
Use your own body weight for back exercises — no additional equipment required.
Three Effective Lower Back Stretches
Here are some of my favorite stretches for lower back pain, which I perform one to two times per week (not daily). Strength exercises follow the stimulus-recovery-improved strength model and don’t require daily dosage.
1. Front Plank
- Lie face down on an exercise mat.
- Place your elbows directly under your shoulders with forearms parallel to each other.
- Extend your legs behind you with feet shoulder-width apart.
- Engage your core by contracting your abdominal muscles.
- Lift your entire torso off the ground, balancing on your forearms and toes.
- Maintain a straight line from head to heels; avoid sagging in the lower back.
- Hold this position for as long as you can while maintaining proper form.
- Start with 15 seconds and increase the duration as you gain strength.
2. Bird Dog
- Start on a mat on your hands and knees.
- Position hands directly under shoulders and knees under hips.
- Engage your core muscles by contracting your abdominals.
- Simultaneously extend your right arm forward and left leg backward until parallel to the floor.
- Start with 30 seconds on each side.
- Slowly increase duration as you gain strength.
3. Superman
- Lie face down on a mat with arms extended in front and legs straight behind.
- Engage your core by drawing your navel toward your spine.
- Simultaneously lift your arms, chest, and legs off the ground.
- Hold for 30 seconds.
- Increase duration as you become stronger.
Extra Credit: Belly Breathing
When tensing your core for these exercises and experiencing discomfort, there’s a tendency toward rapid, upper-torso-based breathing. Continue belly breathing despite the tension in your core.
This is not only good training but also a great example of how slow breathing helps with your pain response as you hold the last seconds of progressively longer positions.
Beyond Lower Back Stretches: A Comprehensive Approach
Lower back stretches are important, but they’re not stand-alone solutions.
Back pain is a signal, and you have to open the mail. With a trusted physician, discuss potential red flags, how you’ll modify your ergonomics, and how you’ll incorporate appropriate stretches for lower back pain.
This comprehensive approach will keep you pain-free and functional throughout the years.
The Health Benefits of Ginger Shots: A Look at the Evidence
Red state versus blue state. Vax versus anti-vax. Chiefs versus Eagles. As a society, we’re growing more polarized, and healthcare is no exception.
The “nature is best” camp views medical technology with suspicion, leading to decisions that potentially put people at risk, such as declining to receive vaccines.
On the other hand, the “science knows best” camp relies entirely on medical discoveries of the last few hundred years, neglecting to acknowledge that our species survived for hundreds of thousands of years before the advent of modern medicine and, therefore, at least some viable healing modalities must have existed.
I’m fascinated by the growing movement of medical science evaluating and validating the health benefit of traditional medical practices, what I call “grandmother” medicine — what she and her countless prior generations knew but only now is being touted as the latest discovery.
Ginger shots fit this paradigm. The benefits of ginger shots are gaining attention, with a Google search yielding everything from Vogue magazine articles to Cleveland Clinic health newsletters touting its many virtues. What’s all the excitement about these ginger shot benefits?
What Are Ginger Shots?
Ginger shots refer to freshly processed whole ginger root, which contains many active ingredients. These compounds include gingerols, shogaols, and zingerone — the biochemical components responsible for ginger’s characteristic flavor and the ginger shot health benefits we’ll explore.
Most scientific studies don’t actually use fresh ginger shots, which are more potent but more challenging to standardize for research. Instead, they typically use capsules with dosages ranging from 0.3–3 grams per day.
The literature I’ve reviewed includes meta-analyses — statistical methods that combine results from many individual studies. While these studies used different formulations and dosages of ginger, the overall conclusion remains consistent: Ginger offers numerous health benefits across multiple bodily systems.
Ginger Shot Benefits: Where the Evidence Is Strongest
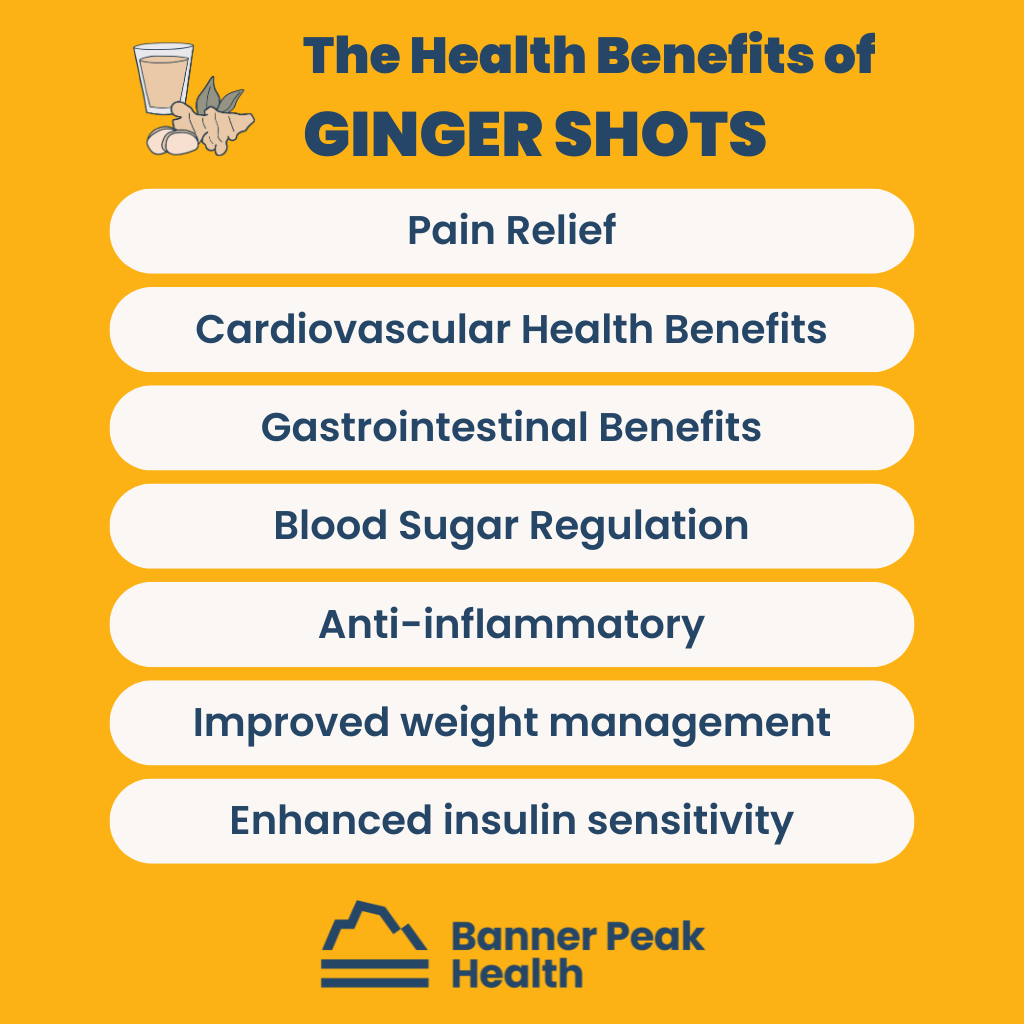
The scientific research shows convincing evidence for ginger’s benefits across several categories:
Pain Relief
Ginger shows strong evidence for reducing various types of pain, including:
- Menstrual cramps
- Osteoarthritis pain
- Delayed onset muscle soreness (DOMS)
Any weekend warrior knows DOMS all too well — that stiffness when you wake up Monday morning, painfully reminded of Sunday’s activities. Ginger appears to mitigate this response.
Cardiovascular Health Benefits
Research shows ginger improves several cardiovascular health markers:
- Improved endothelial function (how well your blood vessels work)
- Reduced risk of coronary artery disease
- Reduced systolic and diastolic blood pressure
- Lower triglycerides
- Reduced LDL (“bad”) cholesterol
These benefits of ginger shots could contribute to overall heart health and reduced cardiovascular risk.
Gastrointestinal Benefits
Some of the strongest evidence for ginger’s effectiveness is in its anti-nausea properties:
- Pregnancy-associated nausea (ginger is the go-to solution here because it’s safe for consumption during pregnancy)
- Chemotherapy-induced nausea
- Post-operative nausea
As someone who’s recommended remedies to countless patients dealing with nausea, ginger’s efficacy in this area is particularly impressive.
Blood Sugar Regulation
In the endocrine category, ginger demonstrates significant effects on blood glucose:
- Improved glycemic control in those with type 2 diabetes
- Reduced fasting blood sugar by approximately 20 points
- Reduced hemoglobin A1c by 0.5–1% — the same magnitude of effect as many prescription medications
Potential Benefits of Emerging Evidence
Beyond the well-established benefits above, research suggests ginger may offer additional health advantages:
- Anti-inflammatory and antioxidant effects
- Improved weight management
- Enhanced insulin sensitivity
While the evidence in these areas isn’t as robust, the consistent pattern of positive findings suggests ginger likely has a wide range of health-promoting properties yet to be fully documented.
How to Get the Most Ginger Shot Benefits: Shots vs. Capsules
A typical ginger shot contains approximately 25–30 grams of fresh ginger, though this varies depending on the brand and preparation method. The concentration of bioactive compounds like gingerols and shogaols also varies between products.
You’ll likely get a higher concentration of active ingredients from fresh ginger shots, but the practicality of long-term use presents challenges. Without significant dedication, it’s much more convenient to use capsule preparations, which fortunately have solid evidence supporting their efficacy for delivering ginger shot health benefits.
When choosing how to obtain the benefits of ginger shots, consider:
- Shots may deliver more potent doses but are less practical for daily long-term use.
- Capsules are more convenient and have substantial scientific backing.
- Commercial shots often contain added sugar, which may undermine some health benefits.
Ginger Shot Side Effects and Precautions
The side effects of ginger consumption are generally minimal. Both shots and capsules can be associated with:
- Mild gastrointestinal disturbance
- Bloating or indigestion
- Unpleasant taste or aftertaste
In rare cases, larger amounts may cause:
- Heartburn
- Diarrhea
- Stomach discomfort
More seriously, large amounts of ginger may increase bleeding risk in some individuals. Ginger may also interact with certain medications, including blood thinners and some diabetes medications.
Consult with your healthcare provider before regularly consuming ginger shots.
The Proven Benefits of Ginger Shots: Bridging the Divide
What’s most fascinating about ginger shots is how they bridge the divide between traditional wisdom and modern science. The evidence supporting ginger shot benefits is clear: your grandmother was right all along.
This hybrid approach — acknowledging traditional practices’ wisdom while subjecting them to scientific scrutiny — represents the best path forward. Rather than remaining in polarized camps, Banner Peak Health embraces both our ancestors’ time-tested remedies and modern medicine’s rigorous verification methods.
Why the Traditional Medical Approach to Sleep Is Failing Us
How do we fall asleep? Do we actively go out and get sleep, or do we create a set of conditions where we allow sleep to come to us?
This may seem like a hypothetical or philosophical distinction, but it’s vital to understanding sleep management.
The advent of the sleeping pill has led to the misconception that sleep is something you can actively obtain, or “go get.” Unfortunately, that’s a false promise.
The Sleeping Pill: A Dangerous Path
The sleeping pill has led us down a detrimental path for two main reasons.
First, sleeping pills are dangerous. There’s robust evidence that sleeping pills are associated with an increased risk of falls, pneumonia, motor vehicle accidents, cognitive impairment, and premature death. At the societal level, they’ve created a very high burden of side effects.
Sleeping pills are also often taken for chronic daily use for years on end, which is off-label (meaning it’s neither how they were studied nor what the FDA approved them for). The sleeping pills’ safety and efficacy have only been demonstrated in trials of several months’ duration (more on this in a bit). Even then, the absolute magnitude of sleep provided was minimal at best.
Secondly, sleeping pill culture has created a false understanding of how we fall asleep. The healthiest and most efficient route to sleep focuses not on how to obtain sleep but on how to identify and maximize the multiple necessary prerequisites to create the conditions for healthy sleep.
The sleeping pill masquerades as a single, simple solution to an undoubtedly multifactorial problem. This is far from the truth. Complicated problems require complicated solutions.
The Pharmaceutical Industry’s Sleep Scam
Just as Big Pharma pulled a fast one on the American people with the narcotic opioid epidemic, drug companies pulled a fast one with the way they got people to think about sleeping pills. It was a scam, and the story needs to be told.
The National Sleep Foundation was founded in 1990 as a nonprofit organization dedicated to educating providers and individuals about proper sleep. Donations funded it, including those from pharmaceutical companies.
In 1992, Sanofi released the first non-benzodiazepine sleeping medication, Ambien (also called zolpidem). By 2008, the National Sleep Foundation, with funding from Sanofi-Aventis (they had merged by then), created a “Sleep Smart Campaign” designed to educate people about insomnia and encourage them to seek medical care.
The campaign included data suggesting up to one-third of Americans were at risk for insomnia. They claimed to educate people about sleep hygiene, but encouraged them to “discuss an appropriate way to take a sleep aid with your healthcare provider.” This wasn’t education — it was an infomercial from a nonprofit.
The result? Prescription sleeping pill rates skyrocketed from 1999 to 2010. A large survey conducted in 2010 found that there had been 53.4 million prescriptions for zolpidem in the United States. We became a nation of chronic sleeping pill users, despite embarrassingly weak data supporting the efficacy and safety of long-term use of medications like zolpidem.
Ambien has never been studied for use beyond 12 months. Even then, there were only two studies — one with 33 patients and one with 89 patients.
Fortunately, the tide began to turn as the side effects of sleeping pills became more apparent. These included increased risk of falls and fractures, cognitive and motor impairment, suicidal ideation, pneumonia, and motor vehicle accidents.
A movement arose to curtail the widespread use of sleeping pills, particularly for those over 65, for whom the risk of side effects is much greater. The National Health and Nutrition Examination Survey revealed that in 2003, an estimated 4.7% of Americans were taking sleeping pills. By 2018, that number had reduced by approximately one-third to 3.4%.
Most importantly, there was a marked improvement in the use of sleeping pills among those over 80, who are at the greatest risk of adverse side effects.
Rethinking Healthcare’s Approach to Sleep
Unfortunately, turning to a simple prescription is all too common. Our current healthcare system doesn’t support a broader, deeper, multifactorial approach that would be more appropriate and help us sleep better.
I use the metaphor of a leaky roof and a raincoat. Doctors in traditional fee-for-service medicine don’t have the time or background to investigate why the roof is leaking (the underlying causes of insomnia). Instead, they quickly prescribe a sleeping pill — the raincoat.
A comprehensive approach to sleep requires careful consideration of the many possible causes of insomnia:
- Concomitant physical diseases like asthma, Parkinson’s disease, and congestive heart failure
- Mental health disorders such as PTSD, depression, anxiety, and bipolar disorder
- Prescription medications associated with insomnia, including steroids, long-acting beta-agonists, and diuretics
- Personal lifestyle substances like nicotine, alcohol, and caffeine
- Lifestyle issues including chronobiology related to light exposure
To merely prescribe a pill bypasses this wide range of potentially reversible or modifiable disorders that could improve sleep without resorting to potentially hazardous sleeping pills — pills that were never studied for safety for the duration they’re currently being used.
That’s what I seek to address as a concierge physician.
Rather than seeing you for a 10-minute appointment, hearing a quick rundown of your sleep habits, and writing a prescription, I may spend an hour speaking with you before I make a recommendation about improving your sleep.
And if I ever prescribe any medication, I’ll be available if you have questions or encounter unforeseen difficulties.
Demographic-Specific Sleep Considerations
Sleep recommendations differ for various age groups. Those over 65 are at markedly increased risk for side effects from sleeping pills, yet they also suffer more concomitant illnesses that put them at risk for sleep problems.
For athletes and high-performance individuals, maintaining appropriate sleep is even more important to optimize recovery. Quality sleep is essential for physical restoration and peak performance.
Graduating From Sleep Medication
As weak as the evidence is for sleeping pills in treating chronic insomnia, the literature is solid on the best alternative: cognitive behavioral therapy for insomnia (CBT-I).
There’s a shortage of providers who offer this service. The pandemic has created a huge access problem for healthcare, especially for therapists trained in cognitive behavioral therapy.
At Banner Peak Health, we connect our members to either in-person therapy, telehealth options, or textbook resources to use the safest and most efficacious form of insomnia treatment.
I highly recommend “Say Good Night to Insomnia” by Greg D. Jacobs. This book has helped many patients, including elderly individuals dependent on sleeping pills, successfully transition away from medication.
Exciting Developments in Sleep Research
The sleep medicine field is advancing rapidly with new technologies that allow us to monitor sleep quality outside traditional laboratory settings. At Banner Peak Health, we’re particularly interested in several innovations:
Wearable Sleep Tracking
The Oura Ring measures body temperature, movement, and heart rate to track sleep stages, sleep efficiency, and overall sleep quality.
Unlike bulky wristbands or watches, the Oura Ring is comfortable to wear during sleep and provides detailed metrics that help us understand sleep patterns over time.
Heart Rate Variability (HRV)
HRV measurement offers a window into the autonomic nervous system’s function during sleep.
Higher heart rate variability typically indicates better recovery and lower stress levels. By monitoring HRV during sleep, we can gain insights into how well your body is recovering and whether your sleep is restorative.
Sleep Imaging Systems
The SleepImage device enables a more detailed analysis of sleep architecture without requiring an overnight stay in a sleep lab. This device can help identify disruptions in sleep cycles and breathing patterns that might be missed with more basic monitoring methods.
By incorporating these technologies into our practice, we can make more precise recommendations for improving sleep quality. However, these tools are supplements to, not replacements for, addressing the causes of sleep problems.
Today’s Takeaways
- Think beyond the sleeping pill. When it comes to sleep, broaden your vantage point to see beyond “quick-fix” medication.
- Think like an internist. Create a “differential diagnosis” by listing the multiple factors you may need to address in order to improve your sleep.
- Remember the fundamentals of good sleep:
- Exercise
- Reduce stress
- Be cautious of your caffeine intake
- Create an environment conducive to sleep
Finally, make sure your physician’s sleep medicine philosophy aligns with your own. Otherwise, you probably won’t see the health results you want.