A Physician’s Guide to Prebiotic Supplements: What the Science Says
The supplement aisle at your local pharmacy is overwhelming. Rows of bottles promise gut health, better digestion, and improved immunity. How do you separate science from marketing hype?
I’ve spent years studying prebiotic supplements. At Banner Peak Health, we take a personalized, evidence-based approach to them. Let me walk you through what we’ve learned.
What Are Prebiotics?
The technical definition: Prebiotics are non-digestible dietary components that resist digestion throughout the small intestine and reach the colon, where they serve as a substrate for fermentation by gut microbes.
The simple version: Prebiotics are food for the bacteria in your gut.
Prebiotics don’t feed all bacteria equally. They selectively nourish the healthier, anti-inflammatory types, including Lactobacillus and Bifidobacterium.
These bacteria have the genetic makeup to process prebiotic compounds. When you consume prebiotics, you’re choosing which bacterial populations get stronger.
Common prebiotic compounds include inulin (found in onions, garlic, and asparagus), fructooligosaccharides (similar food sources), galactooligosaccharides (found in legumes), and pectin (found in apples and pears). If you’re eating fiber, you’re eating prebiotics.
Prebiotics for Gut Health vs. Probiotics
Patients often confuse these two terms, so let me clarify.
Probiotics are live microorganisms you consume directly, either in supplement form or through foods like yogurt, kimchi, miso, tempeh, and kefir. You’re swallowing the actual bacteria.
Prebiotics support the healthy bacterial populations already living in your gut. Probiotics are the guests you’re inviting to dinner, while prebiotics are the meal you’re serving to the guests already at the table.
Both have their place in a gut health strategy. Prebiotics for gut health work by feeding the good bacteria, which then produce beneficial compounds called short-chain fatty acids. This is where the health benefits begin.
The Science Behind Prebiotics for Gut Health
When your gut bacteria ferment prebiotic fiber, they produce short-chain fatty acids (SCFAs), primarily acetate, butyrate, and propionate. These compounds have wide-ranging health benefits.
Your gut lining is a barrier between intestinal contents and your bloodstream. A healthy barrier keeps nutrients in and pathogens out.
When this barrier breaks down (sometimes called “leaky gut” or dysbiosis), microbial compounds, such as lipopolysaccharides, can leak into circulation. This triggers inappropriate immune activation and chronic inflammation.
SCFAs strengthen this intestinal barrier. They also modulate immune response, improve stool consistency and frequency, support glucose management, and improve lipid profiles. Emerging research suggests they may support mood and cognitive function, though that evidence isn’t as strong yet.
SCFAs increase calcium absorption and may help decrease bone turnover markers in post-menopausal women. Studies show increased activity of osteoblasts (bone-building cells) in animal models.
The flip side is equally revealing. When researchers examine patients with systemic disorders, they consistently find dysbiosis. Type 1 diabetes, multiple sclerosis, rheumatoid arthritis, celiac disease, lupus, IBS, Crohn’s disease, inflammatory bowel disease, obesity, and liver cirrhosis all reflect disrupted gut microbiomes.
This doesn’t prove causation, but the pattern is clear: A balanced gut microbiome correlates with better health outcomes across the board.
Finding High-Quality Prebiotic Supplements
The supplement industry isn’t regulated like pharmaceuticals. Product quality differs between brands.
I look for third-party verification from organizations such as USP, NSF, or ConsumerLab. This testing confirms the product contains what the label claims and isn’t contaminated with harmful substances. It’s not always possible to find verified products, but that’s my starting point.
Most Americans consume only 10–15 grams of fiber daily. The goal is 30 grams or higher; I often aim for 40–50 grams with my patients. This gap is where prebiotic supplements become useful.
How to Test Prebiotic Supplements
A proper experiment requires a protocol. Here’s the approach I recommend:
Start with your goals. Talk to your doctor about what you’re trying to accomplish. Are you dealing with constipation? Looking to support metabolic health? Your goals determine which prebiotic supplement makes the most sense.
Start low, go slow. Your gut microbiome can change rapidly, but you don’t want to shock your system. Gradually increase your intake over several weeks.
Be consistent. Three to four weeks of regular use is the minimum trial period. You want to consistently feed those good gut microbes so they can flourish and produce downstream health benefits.
Monitor for side effects. Bloating, diarrhea, and flatulence are common when introducing fiber. Some products cause fewer side effects than others.
Track your results. If you’re dealing with constipation, you’ll notice improved bowel regularity and more complete bowel movements. You’ll spend less time on the toilet and feel less bloated.
For patients with more complex issues, we’ve explored microbiome testing kits. We’re not high on them for everyone, but they can be relevant tools for certain cases.
Food First, GI Supplements Second
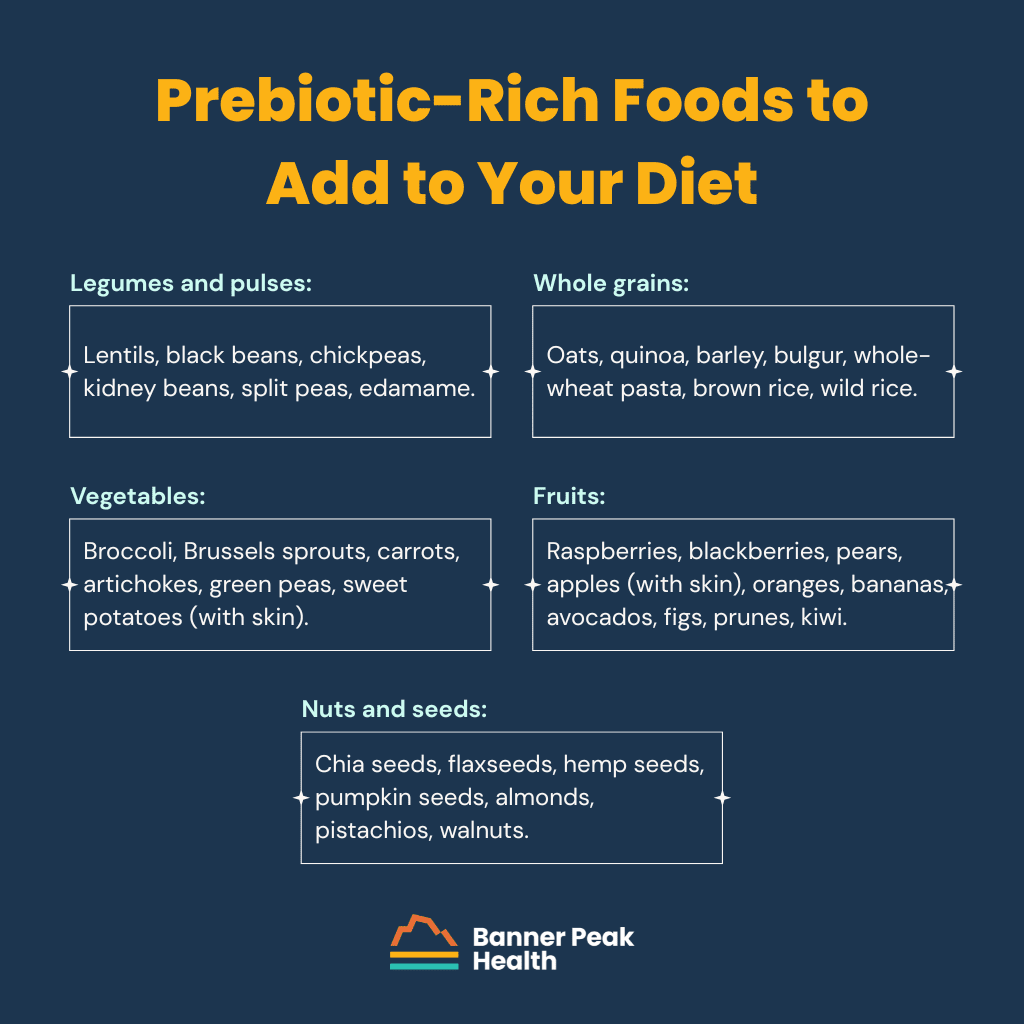
I recommend dietary fiber as the foundation of any GI supplements strategy. The list of prebiotic-rich foods is extensive:
- Legumes and pulses: lentils, black beans, chickpeas, kidney beans, split peas, edamame
- Whole grains: oats, quinoa, barley, bulgur, whole-wheat pasta, brown rice, wild rice
- Vegetables: broccoli, Brussels sprouts, carrots, artichokes, green peas, sweet potatoes (with skin)
- Fruits: raspberries, blackberries, pears, apples (with skin), oranges, bananas, avocados, figs, prunes, kiwi (with the skin for more fiber and vitamins)
- Nuts and seeds: chia seeds, flaxseeds, hemp seeds, pumpkin seeds, almonds, pistachios, walnuts
Consume a variety of soluble and insoluble fiber sources. Each type of plant food brings different phytonutrients and feeds different bacterial populations.
For constipation in particular, kiwi and prunes have solid research behind them. One multi-center randomized controlled trial found that eating two kiwis a day for four weeks improved complete spontaneous bowel movements in patients with functional constipation.
Prebiotic Supplements I Recommend
After trying multiple different fiber supplements myself, here’s what I’ve learned.
Psyllium Husk
Psyllium has the strongest data for treating constipation of all fiber supplements. The evidence is solid. For many of my patients with constipation, psyllium makes a dramatic difference.
Three reputable brands:
A note on safety: All psyllium products carry a Prop 65 warning due to lead content. Psyllium comes from plants that absorb lead from soil, so some contamination is inevitable.
ConsumerLab tests these products annually, and results differ by batch. One year, Yerba Prima tests best; the next year, it’s Organic India.
For patients with severe constipation, the trade-off is likely worthwhile. The amounts needed for therapeutic benefit are unlikely to cause major harm, but this concern has led me to explore alternatives.
Inulin
Emerging data supports inulin, particularly chicory inulin. A 2025 randomized controlled trial found 12 grams per day for four weeks increased stool frequency, improved abdominal symptoms, improved quality of life, and increased butyrate-producing Bifidobacterium populations.
Thorne FiberMend
I steer most patients toward this product. Thorne is an excellent brand overall, and FiberMend is NSF certified with third-party verification.
It’s a combination of rice bran, guar gum, and apple pectin. Pectin has decent data supporting its effect on motility. The product contains Sun Fiber (a standalone guar gum product with its own evidence base), so you get multiple benefits in one supplement.
FiberMend doesn’t have a strong flavor, so it’s easier to take than psyllium. It causes less bloating and flatulence than psyllium for most patients.
Sunfiber
If you want a simpler option, Sunfiber contains only guar gum. It’s well-tolerated and doesn’t cause the same GI side effects as psyllium.
The Banner Peak Health Approach to Prebiotic Supplements
At Banner Peak Health, we take a personalized approach to prebiotic supplements. Your goals, symptoms, and preferences all influence our recommendations.
Some patients can’t tolerate mixing powder into a drink every day. For them, encapsulated psyllium might be the answer. Frequent travelers may need portable packets they can take on the road.
We’ll help you figure out the best option for your body and your lifestyle. Then, we’ll monitor your progress together and adjust as needed.
If you’re interested in using prebiotics for gut health, start the conversation during your next visit. We’re here to help you become an informed, empowered partner in your own health, not a passive consumer of GI supplements.
What Is Ultra-Processed Food? Why Are Ultra-Processed Foods Bad for You? A Doctor Explains
The term “ultra-processed food” is everywhere right now, but it’s often confused with simple junk food.
So, what is ultra-processed food? Why are ultra-processed foods bad for you? As a physician focused on prevention, I explain the distinction to patients regularly, and the difference matters more than most people realize.
Fifty-three to 58% of Americans’ total daily calories come from ultra-processed foods. Historically speaking, human beings were only recently exposed to these substances. No surprise, then, that we’re learning exposure to this stuff has serious health consequences.
What Is Ultra-Processed Food?
There’s no universally agreed-upon definition, but the NOVA classification system provides a useful framework: Ultra-processed food consists of formulations of ingredients, mostly of exclusive industrial use, resulting from a series of industrial processes.
Ultra-processed foods contain substances with no real culinary use: things you’d never find in a home kitchen. High fructose corn syrup and hydrogenated oils are prime examples. Manufacturers add these ingredients to extend shelf life, improve appearance, and increase palatability.
Whole Foods vs. Minimally Processed Food vs. Ultra-Processed Food
Imagine your grocery store’s produce department. What do you find there? Uncooked beans, lentils, fruits, vegetables, nuts, seeds, eggs, and fresh meats.
These are whole foods, unadulterated products you could find in nature.
Minimally processed foods have been cleaned, chopped, frozen, or dried without fundamental chemical alteration. Frozen fruit, canned beans with some added spices and salt, and rolled oats fall into this category. Mechanical processing differs from chemical manipulation.
Ultra-processed foods occupy the opposite end of the spectrum. Consider deli meats: a perfectly round shape with rivets from something compressing it, wrapped in plastic shrink wrap. I’ve never seen an animal that looks like that.
Compare that to a butcher slicing from a whole turkey breast that’s been roasted in-house. The difference is stark.
Why Are Ultra-Processed Foods Bad?
We don’t know all the effects of every chemical additive, but common sense suggests avoiding substances humans never encountered throughout our evolutionary history.
Here are just a few reasons ultra-processed foods are bad for you:
Engineered for Overconsumption
Ultra-processed foods are scientifically engineered to be highly palatable, with high levels of sugar, fat, and salt. When you eat these foods, your brain responds as though it’s discovered something precious.
Historically, we were hunter-gatherers who didn’t have these nutrients in abundance. Your brain says, “Fat! Sugar! This is great. Let me gobble this up because I don’t know when I’ll find it again.”
If you pause and reflect on eating a bag of potato chips, you’ll recognize the addictive quality. This isn’t just perception; data supports the fact that these foods are genuinely addictive.
They activate brain reward circuits, flooding your system with dopamine and serotonin. Every bite delivers a rush of chemicals that says, “Give me more.”
Disrupted Hunger Signals
Need another reason ultra-processed foods are bad? They disrupt the gut-brain axis.
This is why GLP-1 agonists work so well: They modulate appetite and gastric motility, counteracting the disrupted signaling that ultra-processed foods create. You consume 2,000 calories but don’t feel full because your satiety mechanisms have been hijacked.
Many ultra-processed foods have high glycemic loads. Eat potato chips or candy, and you get a euphoric spike in blood sugar followed by a crash that leaves you hungrier than before.
Structural Brain Changes
Brain imaging studies show that ultra-processed foods structurally change your brain.
Areas involved in inhibitory control and reward processing are affected. More concerning, these changes occur in regions associated with neurodegenerative diseases like Alzheimer’s, multiple sclerosis, and Parkinson’s.
The Health Consequences
The downstream effects of eating ultra-processed foods include increased risk of diabetes, obesity, cardiovascular disease, and neurodegenerative conditions.
Multiple studies demonstrate increased all-cause mortality: Consume these foods in excess, and you’re more likely to die at an earlier age.
The Mediterranean Diet Connection
There’s a hypothesis about “healthy” diets like the Mediterranean diet. The benefits may not come solely from the healthy foods you add; they may come from the bad ultra-processed foods you remove.
I believe it’s a combination. You’re removing addictive substances that compel overconsumption, and you’re adding nutrient-dense whole foods.
I tell my patients to eat out less, avoid junk and bad ultra-processed foods, focus on plants, and include lean animal proteins. Once you understand these mechanisms (what’s actually happening to your brain when you eat these foods), that knowledge will compel you to change.
How to Identify Bad Ultra-Processed Foods
If you can’t pronounce an ingredient, it’s probably a chemical that doesn’t belong in your food.
Will it cause you to grow an extra arm? No. But human beings didn’t evolve with these substances as part of our daily intake.
Beware the Marketing
Health is a marketing scheme. Every bag of chips and box of cereal carries some health-related messaging.
“Eat these Fruit Loops! They have all the vitamins and minerals you need!” In reality, it’s all additives with no natural component.
The current fad is high-protein chips. Maybe they’re not the worst thing in the world, but instead of eating protein from a bag of chips, have a chicken breast with a salad, trail mix, a can of tuna, or Greek yogurt. These are better protein sources.
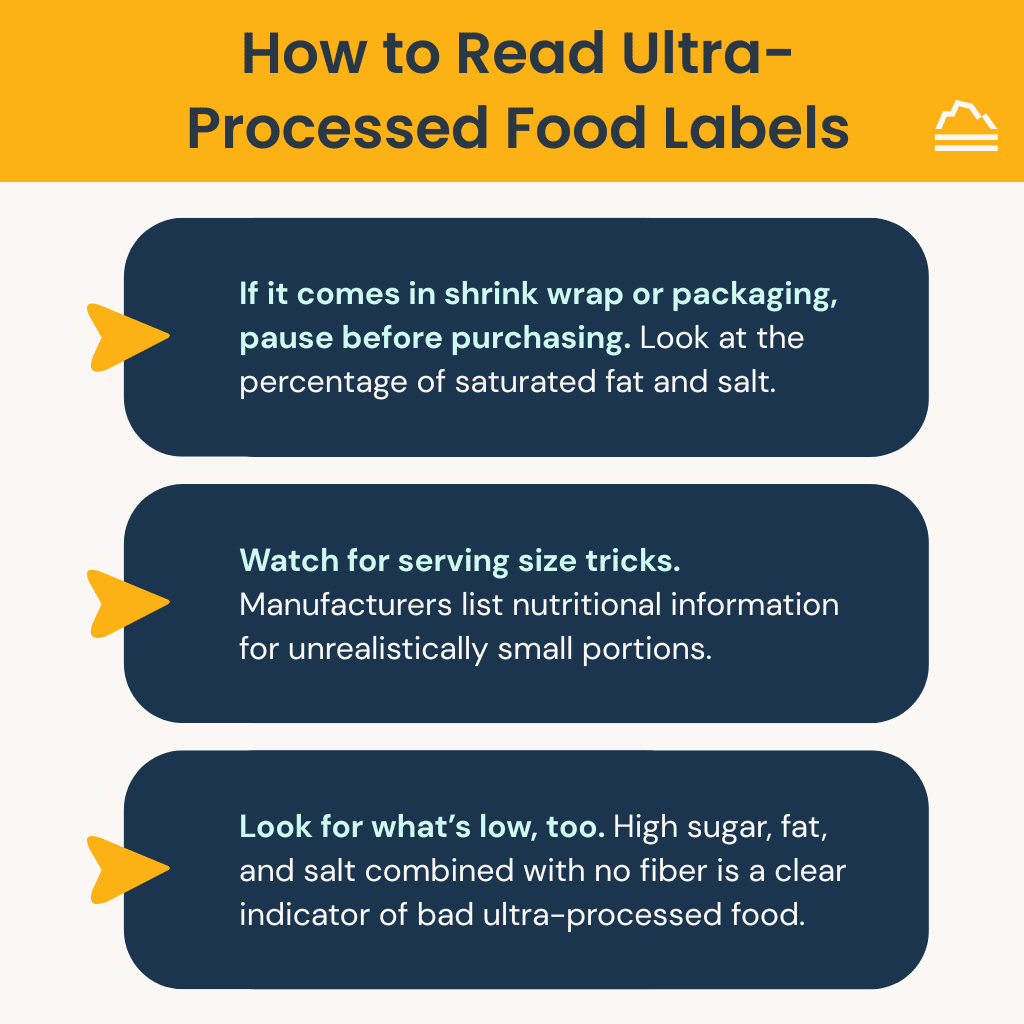
Reading Ultra-Processed Food Labels Effectively
If it comes in shrink wrap or packaging, pause before purchasing. Look at the percentage of saturated fat and salt. If something contains 50% or more of your daily salt intake, that’s a red flag.
Watch for serving size tricks. Manufacturers list nutritional information for unrealistically small portions. That bowl of ramen noodles might claim to be four servings when you know you’ll eat the whole thing. Multiply accordingly.
Look for what’s low, too. High sugar, fat, and salt, combined with no fiber, is a clear indicator of bad ultra-processed food. Ask yourself, how was this made? Was it minimally processed and packaged, or does it contain refined flour and unrecognizable ingredients?
How to Start Removing Bad Ultra-Processed Foods From Your Diet
Be realistic with your expectations. Cleaning your entire pantry overnight isn’t sustainable for most people. Instead, find one ultra-processed food in your normal routine and replace it.
Maybe you eat chips every day. Replace them with popcorn you make yourself (not the bagged kind loaded with butter and additives, but kernels you pop and season lightly). Or, swap the chips for carrots, vegetables, and hummus.
If you don’t know how to cook, now’s the time to learn. When you prepare your own food, you control what goes into it, and you’ll know you’re eating fewer ultra-processed foods.
The Salad Challenge
Instead of snacking on bad ultra-processed foods, have one salad with lean protein every day for a month. See how you feel.
It doesn’t matter how much salad you eat. You won’t gain weight. You’ll only benefit from a nutritional and metabolic perspective.
Here’s what I put in my salads:
- Arugula
- Cucumber
- Tomato
- Spinach
- Kale
- Multiple colored peppers
- Carrot
- Onion
- Beets
- Feta cheese
- Lemon and olive oil dressing
- Dried herbs (basil, oregano, thyme, rosemary)
- Lean protein (chickpeas, beans, tuna, or chicken)
That’s potentially eight to 10 different plants in a single meal. See how many you can fit.
View Food as Fuel
People come to me wanting to feel better, optimize their health span, and reduce their risk of chronic illness. To accomplish those goals, you need to give your body the best fuel possible. If you owned a Lamborghini, you wouldn’t put diesel in it; that would ruin the engine. The same logic applies to your body.
This principle applies to how we raise our children, too. What do we put on their plates? Kids will inevitably eat snacks at birthday parties, but is that the food we keep in the house all the time?
If you want your child (or even your pet) to be as healthy as possible, provide the highest quality fuel.
Today’s Takeaways
What is ultra-processed food? Why are ultra-processed foods bad? Knowing the answers to these questions helps you make better choices.
Start small. Replace one ultra-processed food item with a whole food alternative. Learn to cook if you haven’t already. See how many plants you can include in your daily meals.
At Banner Peak Health, we work with patients to develop sustainable nutrition strategies that support long-term health. During your next visit, we’re happy to discuss your dietary habits and create a plan that works for you.
Is Dairy Good or Bad for You? A Physician Settles the Great Dairy Debate
For decades, campaigns like “Got Milk?” positioned dairy as a nutritional cornerstone. Today, it’s one of the most controversial topics in nutrition.
So, is dairy good or bad for you? The answer is neither… and both.
Like most nutritional principles, it comes down to moderation. Milk is milk. How we consume it, and how much, determines whether we experience health benefits or health risks.
The Nutritional Case for Dairy
People have been drinking milk for thousands of years. When you examine its nutritional content, the appeal is obvious: It’s nutrient-dense.
A single serving of milk delivers protein alongside an impressive array of vitamins and minerals: calcium, magnesium, potassium, zinc, selenium, vitamins A and B12, and riboflavin. Few other beverages pack this much macro- and micronutrient potential into one glass.
Research supports several health benefits, particularly for low-fat dairy and yogurt. The calcium and protein content (without excessive saturated fat) contributes to better bone health. This matters for osteoporosis prevention and reducing bone degeneration over time.
Some studies suggest links to lower cardiovascular disease risk. And perhaps most notable: Dairy consumption may be protective against colorectal cancer, likely due to increased calcium intake.
The Concerns: Prostate Cancer and Parkinson’s Disease
The primary concerns around dairy center on two conditions: prostate cancer and Parkinson’s disease.
Multiple meta-analyses suggest a modest association between high dairy consumption and prostate cancer risk. One data point: an 11% higher risk of developing prostate cancer for every 400 grams of milk consumed daily, or roughly two cups.
Modern dairy cows are bred to be hyper-producers of milk. This milk contains elevated levels of IGF-1 (insulin-like growth factor 1), a hormone that stimulates growth. In laboratory experiments, IGF-1 promotes the proliferation of prostate cancer cells and can inhibit apoptosis, the programmed death of normal cells.
There’s another proposed pathway: Whey casein protein may boost an enzyme called TOR, which has been shown to accelerate prostate cancer growth.
Association doesn’t equal causation. These findings show a link, not proof that milk causes prostate cancer. The relationship appears dose-dependent: Drinking large quantities increases risk, but moderate consumption likely does not. And if IGF-1 were truly driving cancer development, we’d expect associations with many cancer types, not just prostate cancer.
The same studies that suggest prostate cancer risk also show dairy may be protective against colorectal cancer. The picture is mixed.
The Parkinson’s disease connection is less clear. Studies show a dose-dependent relationship (high milk consumption correlates with increased risk), but researchers don’t understand why. The association isn’t seen with fermented dairy products like yogurt, only with milk itself.
Recent research has identified a strong link between pesticide exposure and Parkinson’s disease. Could pesticide contamination in milk explain the association? It’s speculative, but plausible.
We can’t say with certainty that pesticides cause Parkinson’s, but the connection warrants attention.
Is Dairy Inflammatory?
Many patients ask whether dairy causes inflammation. I searched the medical literature and found no clear data supporting this claim.
Despite what circulates online (advice to avoid milk when you have a cold or are trying to reduce inflammation), the evidence isn’t there.
Understanding Lactose Intolerance
Beyond disease associations, the most common dairy concern is lactose intolerance. It affects a staggering 65–76% of the global population to some degree.
Lactose intolerance is largely genetic. It’s more common in African, Asian, Latino, and Native American populations and far less common in those of European descent. As we age, the enzyme that breaks down lactose (called lactase) becomes less efficient or decreases in quantity.
The symptoms are familiar: abdominal pain, bloating, flatulence, and diarrhea. When lactose isn’t broken down in the small intestine, it passes into the colon. Gut bacteria then ferment it, producing hydrogen gas, the culprit behind the discomfort.
Diagnosis rarely requires formal testing. A therapeutic trial works well: Avoid dairy, see if symptoms improve, reintroduce it, see if symptoms return. If you want to continue consuming dairy, try taking a lactase enzyme beforehand and assess the results.
For those curious about a formal diagnosis, there’s a hydrogen breath test. You consume a lactose load, and clinicians measure hydrogen in your exhaled breath. Elevated levels confirm the diagnosis. But most patients never need this.
Practical Solutions for Dairy Sensitivity
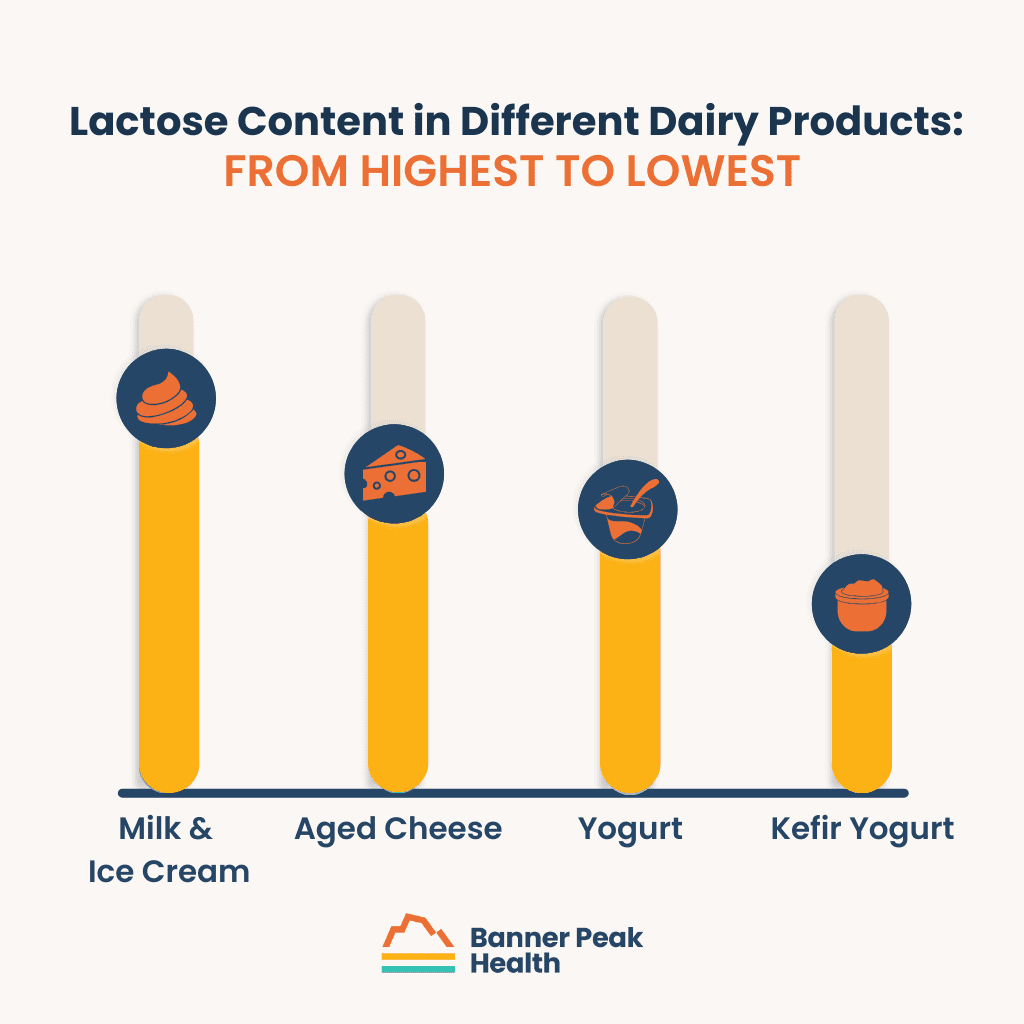
Not all dairy is created equal when it comes to lactose content.
Milk and ice cream contain the highest amounts. Harder, aged cheeses contain less, as the aging process reduces lactose. Yogurt has less than milk, and kefir yogurt has even less than regular yogurt.
If you’re somewhat sensitive (meaning you have reduced but not absent lactase enzyme), you may tolerate aged cheeses, kefir, or yogurt without issue but struggle with milk or soft cheeses. Experiment to find your threshold.
There’s A2 milk, a new option you may have noticed in grocery stores. Milk contains two types of casein protein, A1 and A2. Most commercial milk contains both, depending on cow breeds selected for high milk production. Some people tolerate A2-only milk better, even independent of lactose content.
If you want to keep milk in your diet but experience discomfort, A2 milk is worth trying.
My Approach With Patients
If you feel fine consuming dairy, you don’t have to avoid it.
I’m not opposed to dairy as a way to get adequate calcium and protein. These nutrients matter, and if dairy helps you meet your needs, that’s a reasonable approach, in moderation.
If there were clear data showing that a specific amount of milk caused cancer, I’d advise avoidance. But we’re dealing with associations, not causation, and many other factors contribute to cancer development (genetics being a major player).
If you’re managing cardiovascular risk, lean toward lower saturated fat options. A 0% Greek yogurt delivers the protein and calcium benefits without the saturated fat of whole-milk varieties. That doesn’t mean you can never enjoy full-fat dairy; just be mindful of the balance.
If the data changes, my opinion will change. Nutritional science is difficult to study rigorously. There’s little funding for large randomized controlled trials on food, since no pharmaceutical company stands to profit. Much of the data is observational, with inherent limitations.
I didn’t find strong evidence that dairy is “bad” for you, but I remain open to updating this perspective if new research emerges. That flexibility is how good medicine works.
Is dairy bad for you? Not inherently. Is dairy good for you? It can be. The answer, as with most nutrition questions, lies in moderation and paying attention to how your body responds.
The Physical and Mental Health Benefits of Hiking: Why Getting Outside Matters More Than Ever
I never feel like I have enough time in the day.
Between patient care, staying current with medical literature, and the endless stream of notifications demanding my attention, I’m constantly bombarded by reminders, meetings, and things to read. This probably applies to you, too, regardless of your career. We’re all drowning in distractions.
That’s why the benefits of hiking are indispensable.
The Physical Benefits of Hiking: More Than Just Cardio
Hiking offers tremendous physical benefits. It’s one of the most accessible forms of exercise across one’s lifespan.
You can hike into your elderly years. You might need a trekking pole for balance as you age, but it’s an activity you can take with you through life.
The benefits of hiking in nature include both cardiovascular and strength training components. When you climb hills, for instance, you engage your core, activate your leg muscles, and use your body differently than you would on flat ground.
Data shows that consistent hiking increases aerobic capacity and skeletal muscle mass. It improves blood pressure and VO₂ max, your body’s ability to use oxygen during exercise. When you’re hiking uphill, you’re doing more physical work, expending more energy, and building strength alongside endurance.
This combination makes hiking valuable. You’re hitting Zone 2 cardio training while loading your joints and muscles to support bone density and functional strength.
Nature Is Therapeutic
Being in nature is therapeutic. You can’t fully separate the physical benefits of hiking from the experience of being outdoors.
Humans evolved in nature. We’re designed to spend time listening to the wind rustle through leaves, observing animals, and being present in an environment akin to what our ancestors experienced.
When you remove yourself from notifications, emails, and endless scrolling, and when you put yourself in a position where you can just exist, you return to an internal place of solitude. It’s a respite from modern life’s stressors.
I attended medical school in Israel, where I found my love of hiking. Whether it was hiking through Ramon Crater (Mitzpe Ramon) or rappelling through canyons at Nachal Darga, I found a hobby and passion that I will continue for life.
Years later, it’s one of the reasons I wanted to move to Northern California. Being outdoors is nonnegotiable for my well-being.
What Is Rucking?
Rucking takes the physical benefits of hiking to another level.
Rucking means hiking with weight on your back. You might use a weighted vest or a backpack filled with 20 pounds, depending on your body size and fitness level. This increases the intensity of your workout without special equipment or gym access.
Rucking isn’t new. It’s been part of military training for years, since soldiers need to cover several miles carrying heavy gear. It’s a test of endurance and physical strength.
When I first started rucking, I threw a 15-pound dumbbell and an old pillow into a backpack and hit the trail. Now, specialized packs and vests are available, but you don’t need them to start.
The benefits are substantial. You’re loading your joints more and improving your bone density, which matters increasingly as we age and naturally lose bone mass. For women at higher risk for osteoporosis and osteopenia, any weight-bearing exercise is valuable. Rucking delivers.
When you carry weight on your back with proper form (poor form increases injury risk), you engage your core and maintain better posture. You work your postural muscles and improve core stability. For those of us who sit at work all day, this is another benefit.
Rucking lets you maximize time efficiency. Taking a 10-minute walk? Add weight and burn considerably more calories while building strength.
Safety note: Rucking is generally safe when done with proper form, but it’s not appropriate for patients with certain joint issues or back or neck problems. If you’re new to this type of exercise, consult your physician first.
Mental Health Benefits of Hiking: The Data Behind the Experience
The mental health benefits of hiking aren’t subjective. They’re measurable, documented, and consistent across medical literature.
Studies show that spending time in nature improves emotional regulation, decreases anxiety and depression scores, and increases overall mood. Researchers have compared urban walks with nature walks and found differences in stress markers, including circulating cortisol levels. Time in forests leads to better life satisfaction and improved cognition.
Research also shows decreased inflammatory markers after experiences of awe in nature. When you stand in front of the Grand Canyon or Yosemite, when you’re struck by the majesty and scale of the natural world, your body responds physiologically.
Stress decreases. Immune function may improve. PTSD symptoms reduce, too, according to some studies.
Mental Health Benefits of Hiking: Hiking as Moving Meditation
You don’t need to be an expert in meditation to benefit from mindfulness in nature. When you walk through the woods, focused on the leaves crunching beneath your feet or the sunlight filtering through the trees, you’re practicing a form of meditation without formal training.
You might use hiking time for deeper introspection. Where am I in life? What am I grateful for? What are my goals?
This intentional reflection becomes powerful when you’re removed from daily triggers and stressors.
Everyone Has Access to Nature
Some people live in urban environments far from wilderness trails. That doesn’t eliminate the benefits of hiking in nature.
In Manhattan, surrounded by brick and mortar, you can go to Central Park.
Walking in a park is different from walking on the street. You’re reducing carbon monoxide exposure. You’re surrounded by grass, plants, and trees. That’s therapeutic.
It’s not as immersive as a forest trail. You don’t feel removed from civilization. But it’s a start, and it’s accessible to most people.
You don’t need an Instagram-worthy backdrop. Find a local trail or park. Your own neighborhood also works if you’re intentional about it. Put weight in a backpack and walk around your block.
Fitting the Physical Benefits of Hiking Into Your Wellness Plan
The physical and mental health benefits of hiking make it a cornerstone of comprehensive wellness. It complements nutrition, sleep, and stress management:
- The light exposure helps regulate circadian rhythm, which improves sleep quality.
- The stress reduction supports better cortisol patterns, which affects everything from weight management to immune function.
- The social connections you make when you hike with others contribute to longevity and health outcomes.
You don’t need to live on top of mountains or visit Yosemite every weekend, but you do need to be intentional about prioritizing outdoor time. That means sacrificing another activity. Maybe you spend four hours on social media every night. That’s where you can shift your time.
You can’t just read about the benefits and do nothing. Spend 15 or 20 minutes thinking about how you’ll incorporate hiking or rucking into your life.
Maybe you substitute your gym treadmill for a trail walk every morning. Maybe you sign up for a backpacking trip. Maybe you commit to 10 minutes outside daily. Even those 10 minutes create measurable benefits.
How to Experience the Physical and Mental Health Benefits of Hiking
You don’t need special gear to reap the physical and mental health benefits of hiking.
Start by just walking outside. Get on a trail. Pay attention to your surroundings.
If you want structure or community, look at group tours or classes. REI offers excellent resources for beginners. Local hiking groups exist in most areas.
Check Meetup for social hiking opportunities. The social element adds another layer of benefit, and you’ll discover new trails through experienced hikers.
Download the app AllTrails. It’s a comprehensive, free app that displays trails near you with difficulty ratings, distances, and user reviews.
This doesn’t have to be as dramatic as a survival reality series. You’re not competing with anyone. You’re just giving yourself space to move, breathe, and reconnect with the environment we evolved in.
Start this week. Find 10 minutes. Step outside. Notice what changes.
Decoding the Labels: The Truth About Organic vs. Non-Organic Foods
You’re standing in the produce aisle, staring at two bundles of spinach. One has a USDA organic label and costs $5.99. The other is $2.99. You reach for the organic option, hesitate, then wonder: Is organic really better?
This question plagues health-conscious shoppers every week. Understanding what separates organic from conventional farming helps you make important decisions about your health, budget, and values.
What Is the Difference Between Organic and Non-Organic?
The difference between organic and non-organic produce starts with how food is grown.
When you see a USDA organic seal on produce, it means that food was produced according to strict federal regulations. These standards prohibit the use of synthetic pesticides, herbicides, fertilizers, genetically modified organisms, sewage sludge, and ionizing radiation, among others.
Organic doesn’t mean zero pesticide use. Organic farmers can use non-synthetic, plant-derived compounds to protect their crops. You’ll find products like neem oil (available over the counter for home gardeners), copper compounds, and sulfur. These natural substances help fight pests and disease.
USDA-certified organic farms must implement environmentally friendly practices, such as crop rotation, composting, and biological pest control. State-dependent organizations conduct farm inspections and testing to verify compliance with these standards.
For a product to carry the organic label, at least 95% of its ingredients must meet organic certification standards. Products labeled “100% organic” contain only certified organic ingredients.
Conventional farming takes the opposite approach, prioritizing yield and efficiency over soil integrity and environmental impact. These farms use synthetic fertilizers, herbicides, insecticides, and fungicides to make their crops resistant to diseases and drought.
Organic vs. Non-Organic Foods: Nutritional Differences
So, does organic produce contain more vitamins and minerals? The research presents a surprising finding: there’s only a minimal difference.
Several studies have shown that certain organic fruits may have higher antioxidant content and lower nitrate levels. When you examine the complete body of research on organic vs. non-organic foods, though, no substantial nutritional differences emerge. You can’t reasonably choose specific products based on superior nutrient density.
The real benefit of organic produce lies elsewhere: reduced exposure to synthetic pesticides.
Conventional produce contains higher levels of pesticide residue, although all levels fall within the Environmental Protection Agency’s safety limits. The EPA regulates the quantities of pesticides to keep consumers safe.
In 2025, a European analysis detected pesticide residue on 85.7% of conventional produce samples versus 40% of organic samples. Multiple meta-analyses confirm that pesticide residue appears about four times more frequently on conventional crops than on organic crops.
Regulations vary by region. More than 80 pesticides banned in the European Union remain approved for use in the United States. European countries tend to implement stricter food safety standards earlier than American agencies, a pattern that extends into pharmaceutical approval.
Health Implications of Pesticide Residue
The EPA maintains that pesticide exposure from conventional produce poses no health risk at typical consumption levels.
Limiting your fruit and vegetable intake because of pesticide concerns is a mistake. Every credible health organization agrees that eating more produce (organic or conventional) provides greater benefits than avoiding it.
The challenge lies in studying pesticide effects on humans.
Most pesticides function as endocrine-disrupting chemicals (EDCs). These compounds mimic or block natural hormones like estrogen, androgens, and thyroid hormones. EDCs can also inhibit enzymes your body uses to produce hormones. The result: potential disruption of both hormone production and your body’s response to hormonal signals.
Researchers have identified several possible health effects.
- Pesticide exposure may impact fertility, though no definitive link exists. If you’re struggling to conceive, reducing your pesticide exposure might be worth considering.
- Some evidence suggests that pesticide exposure during pregnancy may affect fetal neurodevelopment by disrupting hormone signaling.
- Studies have explored potential links to hypothyroidism, though the data remains inconclusive.
- Pesticide exposure may be linked to Parkinson’s disease, according to some studies.
Glyphosate is a herbicide that appears in many conventional crops, particularly oats. You’ll often see organic oats labeled “glyphosate-free.” The World Health Organization classifies glyphosate as a probable human carcinogen based on epidemiological associations with non-Hodgkin’s lymphoma. The U.S. EPA disagrees, stating glyphosate is unlikely to be carcinogenic at real-world exposure levels.
Another pesticide, chlorpyrifos, showed stronger evidence of harm. Epidemiological studies identified adverse neurodevelopmental outcomes in children exposed during pregnancy, with a dose-response relationship. Higher exposure during the first and third trimesters led to a greater likelihood of neurodevelopmental problems.
Chlorpyrifos was banned in the EU in 2020, and in 2021, the EPA effectively banned its use on food and feed crops in the U.S. Two years later, the U.S. Court of Appeals for the Eighth Circuit overturned that ban and sent the matter back to the EPA for further proceedings. As of this writing, the EPA is re-evaluating chlorpyrifos regulations.
Studies examining long-term health associations face a limitation: people who consume organic produce tend to be healthier overall. These individuals make other health-conscious choices, creating unavoidable bias in observational data. Associations between organic food consumption and lower rates of obesity, hypertension, and metabolic disease don’t prove causation.
No randomized controlled trials or meta-analyses have shown long-term health benefits from organic produce. The primary proven advantage is reduced pesticide exposure. The nutritional benefits of consuming produce far outweigh the potential risks associated with pesticides.
Environmental Impact: Beyond Personal Health
Your food choices affect more than your body. Organic and conventional farming have vastly different environmental footprints.
Organic farming yields healthier soil, characterized by increased organic matter and enhanced microbial diversity, which in turn improves long-term soil fertility and water retention. Reduced synthetic pesticide use means more insects, pollinators, and beneficial soil organisms thrive. These elements create a natural, healthy soil environment that produces better crops over time.
Conventional fertilizers and pesticides create another problem: runoff. Heavy rain can wash these chemicals into local water sources, contaminating rivers, lakes, and groundwater. This affects the aquatic organisms and animals that rely on these water sources.
Water treatment facilities remove most contaminants before human consumption, but runoff remains an environmental concern.
Strategic Shopping: The Dirty Dozen and Clean Fifteen
Cost is most families’ biggest barrier to buying organic. You don’t need to purchase all organic produce to reduce your pesticide exposure. Strategic choices make the biggest difference.
The Environmental Working Group (EWG), a nonprofit organization, helps consumers make better decisions. The EWG analyzes data the USDA collects on pesticide residue in produce.
The USDA’s testing methodology is interesting: instead of testing produce straight from the farm, testers wash and prepare samples as consumers would at home, which reflects real-world pesticide exposure. They rinse produce under running water for 15 to 20 seconds. If the item requires peeling, they peel it.
The EWG ranks produce based on four variables:
- Abundance: The percentage of samples with at least one detected pesticide
- Diversity: The average number of different pesticides on a single sample
- Intensity: The concentration of pesticides
- Toxicity: Estimated toxicity based on pesticide concentration
This analysis produces two lists: the Dirty Dozen (highest pesticide residue) and the Clean Fifteen (lowest pesticide residue).
The Dirty Dozen includes produce with higher pesticide levels: spinach, grapes, blackberries, blueberries, and strawberries. Berries consistently rank high for pesticide residue.
The Clean Fifteen features items with thicker peels or protective layers: pineapple, corn, avocado, onions, and watermelon. You remove these protective layers before eating, so you don’t need to invest extra money in organic versions.
Here’s an example: Most grocery stores stock both organic and conventional bananas. Bananas have thick peels that you remove before eating, so you’re probably fine choosing conventional bananas. The price difference is minimal, but the pesticide exposure difference is negligible.
Today’s Takeaways
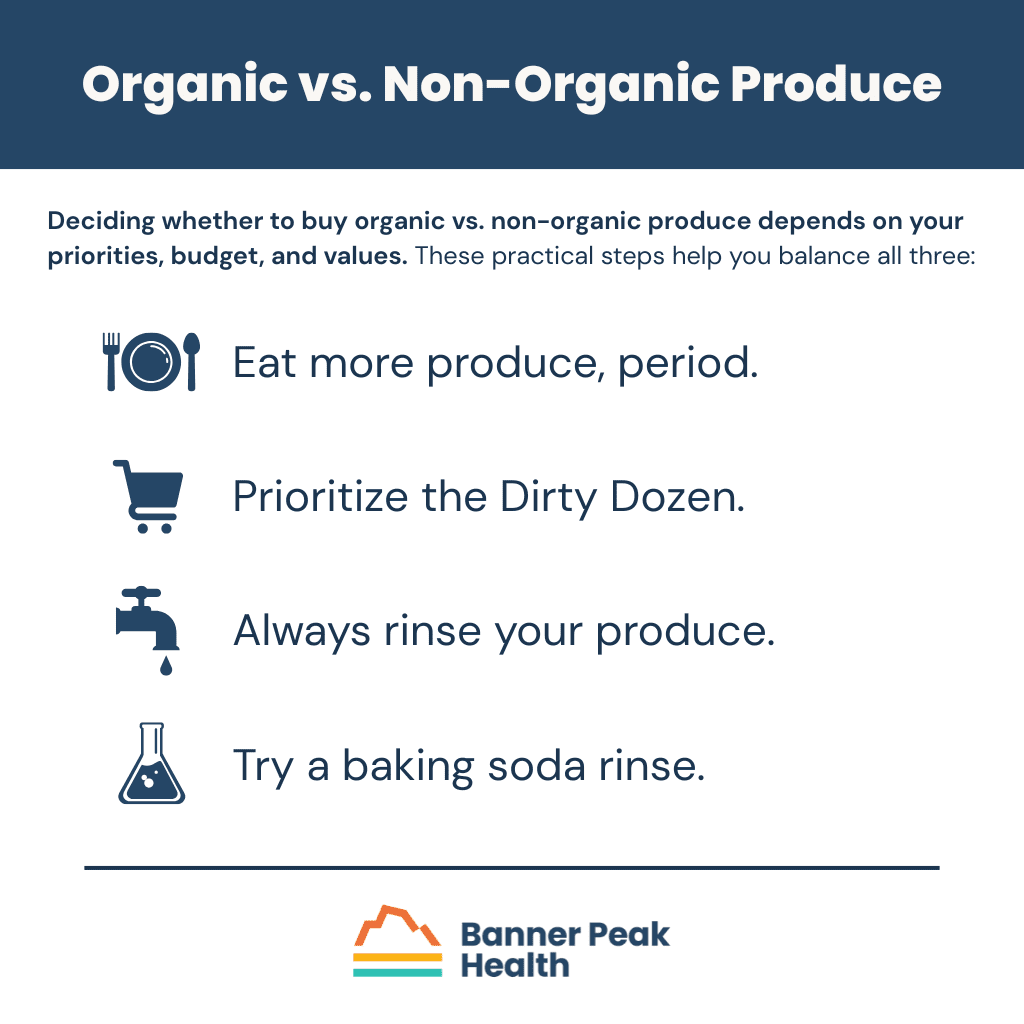
Deciding whether to buy organic vs. non-organic produce depends on your priorities, budget, and values. These practical steps help you balance all three:
Eat more produce, period. Don’t limit your fruit and vegetable intake over pesticide concerns. The nutritional benefits outweigh potential risks.
Prioritize the Dirty Dozen. If you want to reduce pesticide exposure, focus your organic purchases on the produce ranked highest for pesticide residue. This provides the most value for your money.
Always rinse your produce. The USDA’s pesticide data comes from washed produce. At a minimum, rinse all produce (organic or conventional) for 20 to 30 seconds under running water.
Try a baking soda rinse. Research shows soaking produce in a baking soda solution removes a large percentage of surface pesticides. A 2017 study found that soaking apples for 12 to 15 minutes in baking soda water removed substantial amounts of surface contaminants (though pesticides that penetrate deeper into the peel remained). Peeling produce eliminates more pesticides but also removes beneficial vitamins, minerals, and fiber.
In my house, we buy organic for the items on the Dirty Dozen list. When organic isn’t available, we use a baking soda rinse. The process is simple: mix about half a cup of baking soda with water, soak your produce for 12 to 15 minutes, then rinse thoroughly.
We don’t measure precisely or create exact percentages. The goal is practical protection, not laboratory precision.
So, is organic really better? The answer depends on what “better” means to you. Organic produce exposes you to fewer synthetic pesticides and supports more sustainable farming practices. It doesn’t provide dramatically superior nutrition. Whether that trade-off justifies the higher cost is up to you.
Make informed choices based on your circumstances, and remember that any produce is better than no produce.
Foods That Fight Inflammation: Your Defense Against Silent Damage
Most people think inflammation means a swollen ankle or arthritis pain. But chronic, low-grade inflammation damages your body silently, with no visible symptoms and no obvious warning signs.
I can measure inflammation with blood tests like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). When someone has rheumatoid arthritis with swollen joints, these markers spike. But the standard American diet creates pro-inflammatory cascades that these tests won’t necessarily detect.
We’re not checking tumor necrosis factor alpha (TNF-α) or interleukin-6 (IL-6) levels in routine practice. Yet we know that processed foods, saturated fats, and sugar increase the production of these inflammatory molecules. They damage your body slowly, contributing to cardiovascular disease and cancer over decades.
Even without clinical measurements, these processes happen beneath the surface. If you want to maximize lifespan and healthspan, address inflammation through anti-inflammatory foods.
How Modern Diets Create Inflammation
The standard American diet, high in saturated fat and sugar but low in fiber, triggers inflammation through several pathways.
Within two hours of eating a high-fat, high-sugar meal, research shows increased IL-6 levels in the blood. These levels drop afterward, but repeated exposure creates chronic inflammation.
Artificial sweeteners and excess sugar alter how immune cells function. They increase pro-inflammatory cytokines like IL-6 and TNF-α. These foods also change your gut microbiome, increasing pro-inflammatory bacteria while decreasing beneficial species.
When harmful bacteria proliferate, they impair gut barrier function. Substances that belong in your gut leak into your bloodstream, triggering inflammatory cascades from white blood cells.
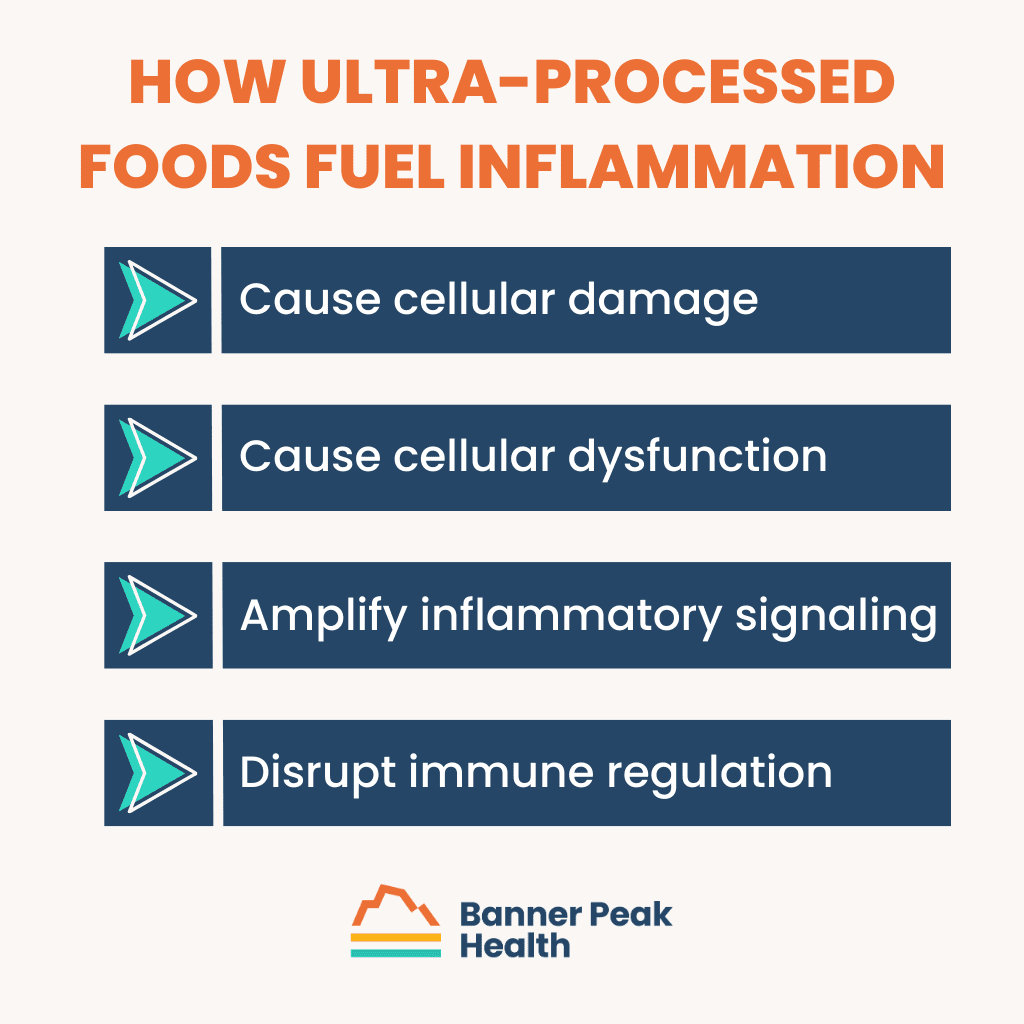
Ultra-processed foods create oxidative stress, generating reactive oxygen species (free radicals). These cause cellular damage and dysfunction, amplifying inflammatory signaling and disrupting immune regulation.
Foods for Anti-Inflammation
The solution involves ingesting foods for anti-inflammation, namely by increasing plant diversity in your diet.
Plants contain phytonutrients that improve gut biodiversity and increase short-chain fatty acid production. Both are necessary for controlling inflammation.
The Power of Color
Anthocyanins, water-soluble flavonoid pigments, give plants their vibrant colors and have powerful anti-inflammatory effects. These compounds make blueberries blue, purple grapes purple, and red peppers red.
Berries contain the highest anthocyanin content among commonly consumed foods. But any brightly pigmented produce delivers these benefits.
Compare a sweet potato to a white potato. The bright orange color signals higher anthocyanin content and greater anti-inflammatory potential.
Dark-colored beans surprised me during my research. Black beans and red beans contain a ton of anthocyanins. The darker the bean, the more anti-inflammatory compounds it contains. Purple cabbage and purple sweet potatoes provide an extra boost of these protective pigments.
When you see bright colors in vegetables and fruits, you’re seeing anthocyanins. Eat the rainbow. It’s that simple.
Turmeric: The Most Studied Anti-Inflammatory Food
Turmeric contains curcumin, a polyphenol compound used in traditional Chinese medicine and Ayurvedic medicine for centuries. It’s probably the most well-studied supplement for reducing inflammation.
Add turmeric to eggs, rice, chicken dishes, or soup. Indian cuisine uses it extensively. However, adding turmeric to food doesn’t match the doses used in clinical studies.
A 2023 meta-analysis examined 66 randomized controlled trials on turmeric and curcumin. Across the board, supplementation decreased CRP, TNF-α, and IL-6 compared to placebo.
These studies used 500–1,000 milligrams of curcumin daily. If you struggle with chronic joint pain despite dietary changes, consider supplementation. Curcumin has very low bioavailability on its own, so look for formulations designed for better absorption.
Thorne makes a quality product using Meriva, a curcumin formulation that’s been widely studied and demonstrated to improve bioavailability. Always consult your doctor before starting any supplement regimen.
Maximizing Absorption
Piperine, a phytochemical in black pepper, acts as a bio-enhancer for curcumin. When you add turmeric to your dishes, include black pepper. The combination boosts bioavailability.
This won’t match the 1,000 milligrams used in clinical studies, but it helps your body absorb more of the curcumin you do consume.
Implementing Foods That Fight Inflammation
To fill your diet with foods that fight inflammation, start by increasing plant variety in every meal. Each plant provides different anti-inflammatory compounds.
For instance, don’t just eat spinach. Add arugula, kale, and other greens. Each features a unique phytonutrient profile.
Focus on deeply colored produce. Choose purple cabbage over green, sweet potatoes over white, and black beans over pinto. The pigments themselves are anti-inflammatory compounds.
Add turmeric to your cooking regularly. Mix it with black pepper for better absorption. If joint pain persists despite dietary changes, discuss curcumin supplementation with your physician.
Today’s Takeaways
Chronic inflammation damages your body even when you can’t see or feel it. The standard American diet promotes inflammatory cascades through processed foods, sugar, and a lack of plant diversity.
Combat inflammation by eating anti-inflammatory foods: colorful produce rich in anthocyanins. Add turmeric with black pepper to your meals. Consider high-quality curcumin supplements like Thorne’s Meriva formulation if you struggle with persistent joint pain.
At Banner Peak Health, we recognize that inflammation underlies many chronic diseases. Making strategic dietary choices today protects your health for decades to come.
The Benefits of Phytonutrients: What Your Nutrition Facts Label Doesn’t Tell You
I’ve spent my career encouraging patients to read the nutrition facts labels on their food, but those labels only tell part of the story.
The most powerful compounds in your broccoli, berries, and Brussels sprouts never appear on any nutrition facts label. These invisible nutrients, called phytonutrients, determine whether your diet protects you from chronic disease.
Phytonutrients: The Hidden Nutrition Gap
Phytonutrients are bioactive compounds found exclusively in plants. Unlike vitamins, you won’t die without them, but there’s a massive difference between not dying and thriving.
These compounds include polyphenols, flavonoids, carotenoids, and phytosterols. If you don’t consume a wide variety of plants, you miss out on nutrients that reduce your risk of cardiovascular disease, diabetes, obesity, and cancer.
How Plants Use Phytonutrients to Protect Themselves (and You)
Phytonutrients are a plant’s defense system. They’re responsible for the colors, flavors, and aromas in fruits, vegetables, whole grains, nuts, and seeds.
These compounds also act as natural pesticides, inhibiting the growth of bacteria and fungi. They help plants cope with drought, extreme temperatures, and UV radiation. When plants face stress, they produce more of these protective compounds.
When humans consume these plant defense mechanisms, they protect us, too. The same compounds that shield plants from UV damage help prevent oxidative stress in our cells, and the natural pesticides that protect plants from pathogens boost our immune system.
Plants can’t run from danger. They’ve developed sophisticated chemical defenses instead. When you eat those plants, you inherit their phytonutrients: their protection.
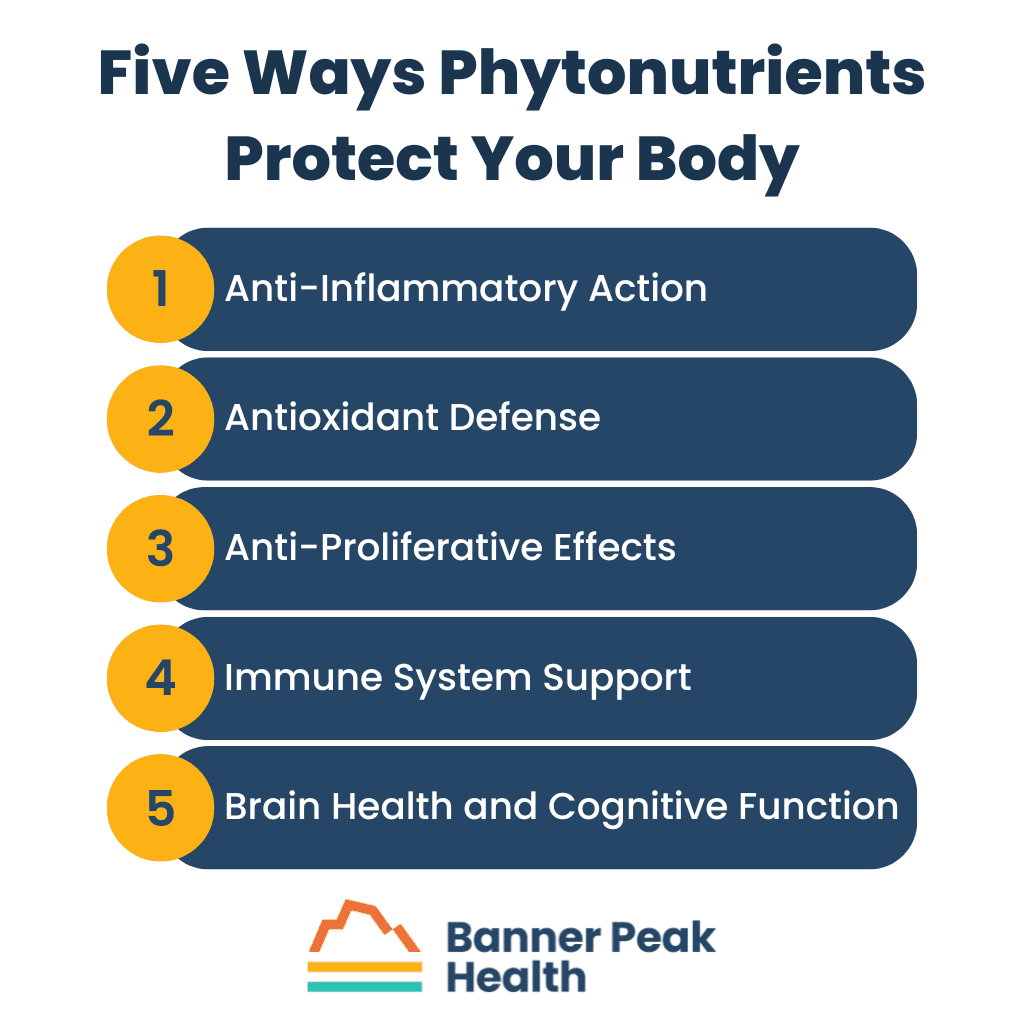
Five Ways Phytonutrients Protect Your Body
Anti-Inflammatory Action
Phytonutrients, particularly polyphenols, suppress the release of pro-inflammatory cytokines like tumor necrosis factor alpha (TNF-α) and interleukin-6 (IL-6). They simultaneously increase anti-inflammatory cytokines like IL-10.
This dual action reduces chronic inflammation at the cellular level.
Antioxidant Defense
Free radicals form naturally as cells age, but environmental factors like smoking, pollution, and UV radiation accelerate their production.
Phytonutrients neutralize these free radicals before they damage your cells. This antioxidant activity protects your DNA, proteins, and cell membranes from oxidative damage.
Anti-Proliferative Effects
Sulforaphane, found exclusively in cruciferous vegetables, promotes apoptosis (programmed cell death) in cancer cells. It arrests cell cycle development, preventing the rapid division that characterizes cancer growth.
Sulforaphane even inhibits angiogenesis, the process tumors use to create new blood vessels for their growth.
Immune System Support
Phytonutrients increase the function of various white blood cells: B cells, T cells, and macrophages, the cells that eat pathogens.
Certain phytonutrients increase our body’s ability to recognize threats and boost macrophage activity, causing them to consume more invaders.
Brain Health and Cognitive Function
Phytonutrients increase brain-derived neurotrophic factor (BDNF) and nerve growth factor (NGF). Both are necessary for synaptic plasticity and neuronal survival, which link to improved learning, memory, and overall cognitive performance.
Beyond “Eat the Rainbow”: Advanced Strategies for Phytonutrient Consumption
Eating colorful foods increases phytonutrient intake. Anthocyanins give foods their vibrant colors, and color diversity equals phytonutrient diversity. But there are more sophisticated approaches.
Preparation Matters
Raw vegetables contain the highest phytonutrient levels. Heat degrades these compounds: higher temperatures and longer cooking times cause more damage.
Steam or lightly sauté your vegetables. Aim for al dente texture: cooked but still firm. If your vegetables are super soft, you’ve reduced their nutritional content.
The Garlic and Onion Hack
When you cut garlic or onions, you trigger the enzyme alliinase. This enzyme creates allicin, which provides many health benefits.
Chop your garlic and onions first, then let them sit for 10–15 minutes before cooking. This waiting period allows the enzyme to produce maximum allicin, increasing antioxidant activity, anti-inflammatory effects, and anti-tumor properties.
Sprouting: The 100X Multiplier
I sprout seeds at home with my kids. It’s simple: put seeds in a jar, add water, and wait. But the science behind it amazes me.
When seeds sprout, their enzymatic activity explodes. They’re trying to grow into plants, which requires massive biochemical changes. These enzymatic processes create higher nutrient levels.
Broccoli is the best example. Mature broccoli contains high sulforaphane levels, but broccoli sprouts contain 10–100 times more sulforaphane than mature broccoli. After just five days of sprouting, you get roughly 10-fold higher content of this anti-carcinogenic compound.
You rarely find sprouts in stores because of shelf stability issues, but making them at home takes minimal effort. Get a sprouting kit (basically mason jars with mesh lids), add seeds and water, rinse daily, and harvest fresh sprouts in two to five days.
Practical Implementation
Don’t reach for supplements. If you’re swallowing a pill to replace a healthy diet, you’re missing the point.
Even if turmeric supplements demonstrate anti-inflammatory effects, taking them while eating processed foods and artificial sweeteners defeats the purpose.
Focus on getting phytonutrients from whole foods first. Add diversity to every meal:
- Get creative with spices: South and East Asian cuisines excel at this. Use garlic, turmeric, cinnamon, ginger, and other spices instead of relying on salt.
- Eat seeds and nuts daily. Add them to your yogurt, blend them in smoothies, mix them into pancake batter, or eat them as snacks.
- Use multiple types of greens: don’t just eat spinach. Add arugula, kale, and other varieties. Each provides different phytonutrient profiles.
Today’s Takeaways
You can’t overemphasize the importance of phytonutrients in your diet. These compounds don’t exist in most people’s nutritional framework, yet they determine whether you merely survive or actually thrive.
Start simple: Increase the quantity and diversity of plants in your diet. Prepare them properly to preserve their phytonutrient content. Try sprouting for a dramatic increase in nutrient density.
Those invisible compounds on your food label might be the most important nutrients you consume.
Best Nasal Sprays for Congestion: A Doctor’s Complete Guide
Many people turn to nasal sprays for quick relief from stuffed noses, but with so many options available, choosing the right nasal spray for congestion can be overwhelming.
Before reaching for any particular nasal spray for congestion, it’s important to understand what’s happening inside your nose.
Understanding Nasal Congestion
When patients suffer from congestion, they’re often experiencing one or both of the following issues:
- Runny nose: Excessive mucus production
- Stuffy nose: Inflammation, making it difficult to pass air through the nasal passages
These symptoms stem from different causes, requiring different treatments. The best nasal spray for congestion in one situation might be ineffective in another.
Common Causes of Nasal Congestion
Understanding what triggers your nasal congestion is the first step toward finding the best nasal spray for your condition. Here are the most common causes I see in my practice:
Allergic Rhinitis (Hay Fever)
Your immune system overreacts to allergens, causing inflammation and increased mucus production.
Nonallergic Rhinitis
Nonallergic triggers, such as weather changes, cause congestion and/or a runny nose.
Occupational and Environmental Irritants
Cold air, cigarette smoke, air pollution, wildfire smoke, perfumes, and detergents can all trigger nasal congestion.
Medications
Many common medications cause nasal congestion as a side effect:
- Antidepressants
- Erectile dysfunction medications
- Blood pressure medications (particularly beta blockers and alpha blockers)
Chronic Alcohol Use
Regular alcohol consumption can trigger chronic nasal congestion and a runny nose, though the mechanisms aren’t fully understood as of this writing.
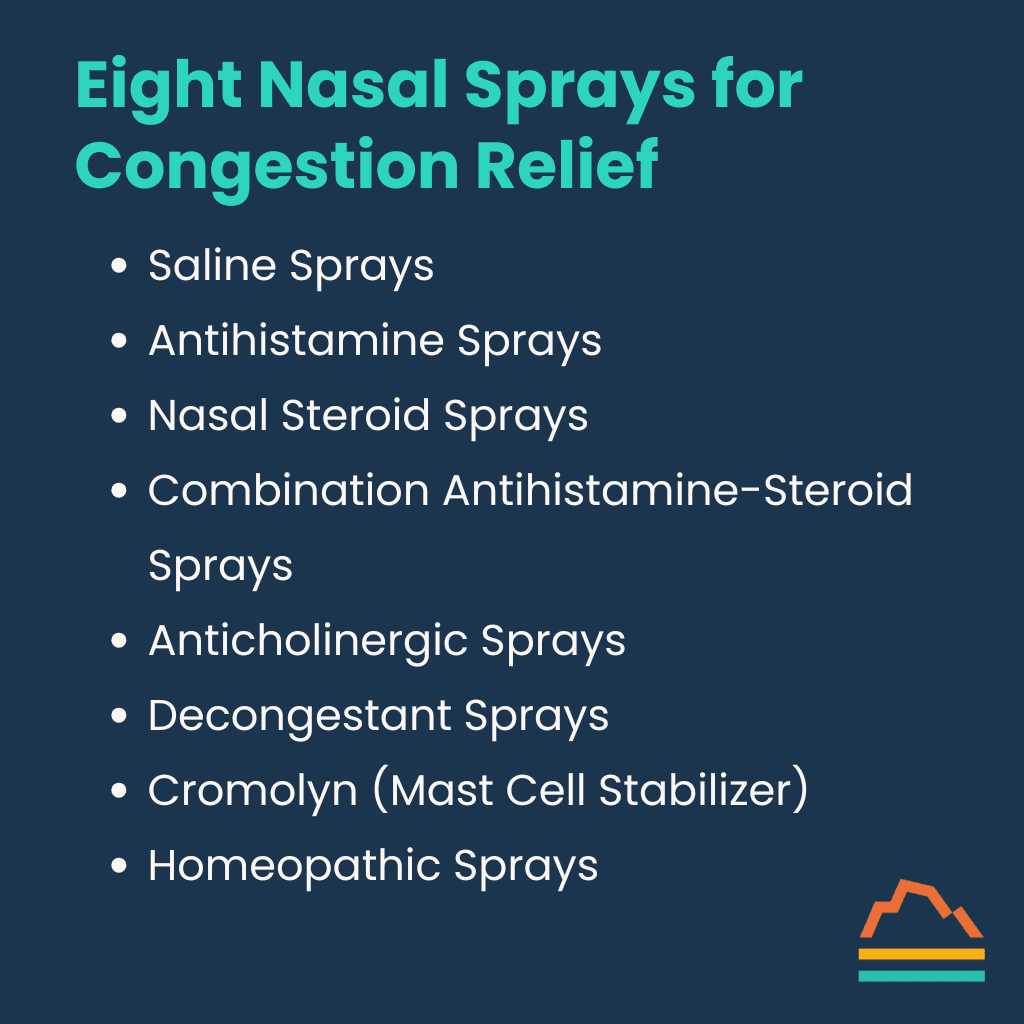
Nine Types of Nasal Sprays for Congestion
Now that we understand nasal congestion’s causes, let’s review different types of nasal sprays for congestion:
1. Irrigation
This isn’t technically a spray, but it’s important to include. Neti pots and similar devices flush out irritants with saline solution.
Important Safety Note: Always use distilled or properly boiled water and clean your device thoroughly to prevent introducing harmful pathogens.
2. Saline Sprays
These sprays moisturize the nasal passages and wash away allergens and irritants that cause inflammation. They’re safe for long-term use.
3. Antihistamine Sprays
Products like Astepro target H1 histamine receptors, blocking the histamine that immune cells release in response to allergens.
How they work: These sprays prevent histamine from binding to receptors, decreasing blood vessel dilation and reducing stimulation of sensory nerves that cause itching and sneezing.
Results appear within 15–30 minutes.
4. Nasal Steroid Sprays
Common options include Flonase (fluticasone), Nasacort (triamcinolone), and Nasonex (mometasone).
How they work: These sprays reduce inflammation by decreasing immune cell activity. When immune cells like eosinophils, neutrophils, and macrophages become less active, they produce fewer inflammatory mediators like histamine and cytokines.
Unlike antihistamines, steroid sprays take time to work — usually one to two weeks of consistent use.
5. Combination Antihistamine-Steroid Sprays
Prescription-only options like Dymista combine fluticasone (steroid) and azelastine (antihistamine) for dual action.
6. Anticholinergic Sprays
Products like ipratropium (Atrovent) target muscarinic receptors.
How they work: These sprays decrease glandular secretions, reducing mucus production and rhinorrhea (runny nose).
They’re particularly effective for patients with chronic runny nose without systemic allergy symptoms.
7. Decongestant Sprays
The most immediately effective (and potentially problematic) option. Brands include Afrin, Vicks Sinex, Sudafed OM, and Xlear, all containing oxymetazoline.
How they work: These target alpha-adrenergic receptors, causing vasoconstriction that reduces blood flow to the nasal mucosa. This decreases edema and mucus production and improves airway patency.
Critical warning: Never use for more than three days. Longer use causes rebound congestion (rhinitis medicamentosa), meaning your symptoms worsen with continued use.
8. Cromolyn (Mast Cell Stabilizer)
Products like NasalCrom stabilize mast cells, reducing their release of inflammatory mediators.
These products are most effective when used preventatively before allergy season begins.
9. Homeopathic Sprays
Products like Zicam claim to work through various mechanisms, but limited research supports their effectiveness.
Potential Side Effects of the Best Nasal Spray for Congestion
Even the best nasal sprays for congestion come with potential side effects:
All Nasal Sprays
Any nasal spray can cause irritation regardless of type.
Nasal Steroids
- Excessive dryness leading to nosebleeds (epistaxis)
- Impaired healing of nasal ulcerations
- Rarely, oral candidiasis (yeast infection)
- Possible association with glaucoma (low risk)
Anticholinergics
- Nasal and throat dryness
- Potential nasal bleeding
Decongestants
- Rebound congestion after three to five days of use
- Increasing dependence with continued use
My Recommendations
For most nasal congestion issues, I recommend a two-step approach:
- Mechanical removal of irritants. Start with saline irrigation or sprays to physically remove allergens and irritants. This reduces the burden of triggers causing your symptoms.
- Anti-inflammatory treatment. Follow with a nasal steroid spray to reduce inflammation. These can be used long-term if necessary.
For seasonal allergies, begin using nasal steroids two to three weeks before your typical allergy season starts.
For severe symptoms, you might temporarily add a decongestant spray (for no more than three days) while waiting for nasal steroids to reach full effectiveness.
For patients primarily experiencing a runny nose without other allergy symptoms, anticholinergic sprays often provide excellent relief.
For pregnant women or women trying to conceive who prefer to avoid steroids, cromolyn may be a good alternative.
Today’s Takeaways
The best nasal spray for congestion depends on your symptoms, their cause, and how long you’ve been experiencing them.
At Banner Peak Health, we don’t practice population medicine. We take time to understand each patient’s unique situation and recommend the right combination of treatments for their specific needs.
If nasal congestion is disrupting your life, let’s work together to find the right solution. We’ve got the time to research these options thoroughly and create a personalized approach for you.
The Ultimate Gut Health Diet: How to Optimize Your Microbiome
To achieve optimal health, we must pay attention to the entire ecosystem inside our bodies: not just our own cells, but the trillions of microorganisms that call our gut home.
Most people know what fiber is and recognize that it exists in food, but they don’t appreciate its role in health. While many Americans obsess over protein content, they overlook fiber as a crucial component of a diet for gut health.
The Foundation of a Gut Health Diet: Understanding Fiber
When discussing an effective gut health diet, we must start with fiber, the cornerstone of digestive wellness. Fiber falls into two categories: soluble and insoluble.
Soluble Fiber
Soluble fiber dissolves in water, creating a viscous, gel-like substance. When consumed, it expands in your stomach and:
- Increases fullness
- Slows gastric emptying
- Helps maintain weight
- Decreases glucose absorption, reducing blood sugar spikes
Popular weight loss medications tout these same effects. Thanks to fiber, you can achieve similar benefits through dietary changes, no prescription needed.
Soluble fiber plays a key role in lowering cholesterol and is an important component of any cholesterol management plan. It binds bile acids in the gut, which reduces the reabsorption of cholesterol. This effect is dose-dependent. The more soluble fiber consumed, the greater the reduction in LDL cholesterol.
Find soluble fiber in the soft, fleshy parts of fruits and vegetables, beans, barley, and oat bran.
Insoluble Fiber
Insoluble fiber doesn’t dissolve in water. It passes through your digestive system largely intact, increasing stool bulk and promoting movement through your digestive tract.
Most plant foods contain both types of fiber. Consider an apple: the flesh contains soluble fiber, while the skin provides insoluble fiber.
The Gut Health Diet Triad: Pre, Pro, and Post
A diet for gut health contains three components:
- Prebiotics (primarily fiber): Fuel for your gut bacteria
- Probiotics: Beneficial living bacteria introduced through food or supplements
- Postbiotics: Your gut bacteria produce these beneficial compounds, including short-chain fatty acids
Think of this like a bee colony: The quality and variety of pollen (prebiotics) determine how many and what kind of bees (probiotics) thrive, which impacts the quality and quantity of honey (postbiotics) produced.
How Much Fiber Do We Need?
The standard American diet includes only 10–15 grams of fiber daily, a fraction of what our bodies need.
For optimal gut health, aim for 30–40 grams daily. Some experts recommend up to 50 grams.
The Power of Plants in a Diet for Gut Health
The foundation of a gut health diet is simple: eat more plants.

I’m not advocating for veganism, as animal proteins are integral to a healthy diet. Just incorporate more plant-based foods from these categories:
- Vegetables: All varieties
- Legumes: Beans, lentils, chickpeas, soybeans
- Fruits: Fresh, seasonal options
- Nuts and seeds: Unsalted, unprocessed varieties
- Whole grains: Brown rice, quinoa, oats, sprouted breads
Practical Tips for a Gut Health Diet
1. Start Low, Go Slow
Don’t change your diet too quickly. Your gut microbiome needs time to adapt.
If you’ve tried beans before and felt sick, consider how you introduced them. Starting with a spoonful and gradually increasing allows your gut bacteria time to adjust. Over time, the populations capable of digesting these foods grow, strengthening your digestive capacity.
2. Diversify Your Plate
At Restaurants
Don’t hesitate to request additions to your meal. Ask for extra vegetables on your salad or sandwich. Most restaurants accommodate health-conscious requests.
At Home
Make each meal an opportunity to support your gut health. For example, switch up a basic salad by:
- Using multiple leafy green varieties
- Adding legumes like lentils or chickpeas
- Incorporating seeds for extra fiber
For sandwiches, upgrade your approach:
- Choose sprouted bread (like Ezekiel) with three grams of fiber and five grams of protein per slice
- Use bean spreads or hummus instead of processed condiments
- Add multiple vegetables for color and variety
3. Start With Breakfast
Breakfast is an opportunity to start your day with a fiber-rich meal. Follow this approach:
- Begin with plain, unsweetened Greek yogurt or kefir
- Add chia seeds, flax seeds, and hemp hearts
- Include crushed walnuts for healthy fats
- Top with fresh berries
This single meal is full of fiber, protein, healthy fats, and probiotics.
Apply the same principle to oatmeal or smoothies, adding multiple plant-based ingredients to maximize nutritional value.
4. Consider Supplements When Needed
Food works best as your primary fiber source, but supplements can help, especially for constipation management.
Psyllium husk is particularly effective. Unlike Metamucil, which contains artificial dyes and sweeteners, choose pure psyllium husk powder. Yerba Prima makes an excellent version.
Here are some tips for using psyllium husk:
- Stir the powder vigorously and quickly to prevent clumping
- Mix it with water and a splash of orange juice for a better taste
- Start with a small amount and gradually increase your intake
- Choose the powder form over capsules for greater effectiveness
Beyond Fiber: The Gut-Body Connection
A gut health diet improves more than just digestion. The short-chain fatty acids your gut bacteria produce support whole-body wellness.
Short-chain fatty acids create healthy enterocytes (the cells that line your gut) that enhance gut barrier integrity. This reduces the movement of harmful compounds from your gut into your bloodstream, decreasing inflammation.
Today’s Takeaways
Your gut microbiome is an essential organ system that requires proper nourishment. When considering your diet, remember that your food nourishes both your body and the trillions of beneficial bacteria supporting your health.
By gradually increasing fiber intake, diversifying your plant consumption, and making strategic dietary choices, you can improve your gut health and reduce inflammation throughout your body.
At Banner Peak Health, we believe in a preventative, nutrition-focused approach to wellness. We know that a proper gut health diet doesn’t require extreme measures; just thoughtful, consistent choices that nourish both you and your microbial partners.
Why I Left Hospital Medicine for Concierge Care
After completing my medical training, I had a clear vision: to connect with patients on a personal level and develop lasting relationships based on trust. I wanted to practice medicine the way I was trained to.
Looking at the healthcare landscape as a newly minted internal medicine doctor, I faced a choice: I could work at a hospital, or I could enter traditional primary care.
The latter system contradicted my values. The model pushed doctors to see as many patients as possible in 15-minute visits — complex health issues squeezed into inadequate time slots.
This approach felt like a disservice to both my patients and myself.
Building Clinical Expertise
I went with the first option. I spent five years as a hospitalist at Northwestern, caring for 15–20 patients a day with complex and often critical conditions.
Those years proved invaluable. I honed my clinical skills, gained extensive experience, and worked alongside specialists in a multidisciplinary environment. I valued the collaborative approach and the immediate impact of caring for critically ill patients.
I noticed that many hospitalized patients could have avoided their situation with proper preventative care. If I had met them five or ten years earlier, perhaps they wouldn’t be in the hospital at all.
During this time, I cared for several patients who belonged to concierge practices. Through them, I met physicians practicing concierge medicine, which aligned with my training and beliefs.
These connections became the bridge to my current practice.
The Move to Banner Peak Health
Both personal and professional factors drove my transition to Banner Peak Health.
On the personal side, after my third son was born, my wife and I reassessed our priorities. We wanted to be closer to our extended families, and we wanted to move to an area where we could more easily participate in activities we love — hiking, biking, and camping — and share those activities with our boys.
Professionally, I was struck by Banner Peak Health’s embodiment of what Dr. Rotman and I call “concierge medicine 2.0.” Traditional concierge medicine (version 1.0) offers excellent medical care, strong community connections, and superior service.
Banner Peak delivers all that, plus the integration of cutting-edge innovations and technologies. It’s a collaborative environment where physicians eagerly learn from each other. We evaluate new technologies, test them ourselves, and help patients implement beneficial solutions.
Another distinction: patient panel size. At my previous practice, I had as many as 440 patients. At Banner Peak, my maximum will be 250. This smaller panel allows me to dive deeper with each patient, discussing nutrition, microbiome, exercise optimization, and more.
The Four Pillars in Real Life
I emphasize four pillars of wellness with my patients: nutrition, exercise, sleep, and stress management. I don’t claim to be perfect in any of these areas, especially after moving across the country with three young children!
Sleep, for instance, is a variable equation with a nine-month-old. Nutrition remains more consistent because I can control what I eat regardless of time constraints.
And when it comes to exercise, I recommend “exercise snacks” for busy patients with young families — short bursts of activity throughout the day. This might mean doing lunges while carrying your toddler, sets of pushups or pullups before a shower, or fitting in wall sits during phone calls. I also try to ride my bike to work most days of the week.
The goal isn’t perfection but consistent effort toward improvement.
Technology as a Health Partner
I’m particularly excited about continuous glucose monitors (CGMs) like Stelo. These devices — once available only by prescription for diabetics — now provide valuable feedback to anyone interested in optimizing their metabolism.
CGMs create powerful input-output feedback loops. Patients see what four slices of pizza do to their blood sugar in real time. Next time, they might choose two slices instead, or they might take a walk after eating to mitigate the spike.
This immediate feedback helps patients understand how their bodies respond to different inputs and outputs, creating accountability that drives positive change.
The Future of Concierge Medicine 2.0
Dedicated time with a physician can fundamentally change a patient’s day-to-day experience. I find profound professional satisfaction in that. Knowing I’ve helped someone make lasting changes that’ll improve their health for years or decades is one of medicine’s greatest rewards.
Beyond individual care, I envision creating a community of like-minded people engaged in health-promoting behaviors. Banner Peak Health builds health partnerships that change lives through personalized preventative care and community support.
When it comes to Banner Peak Health’s future, I envision more than individual doctor-patient relationships. I see a community where like-minded people support each other’s health journeys. This community approach amplifies the benefits of personalized care, as patients connect, share experiences, and motivate each other toward better health outcomes.
I’m excited to be a part of it.