NSAIDs: How Much Anti-Inflammatory Medication Is Too Much?
The medical community may be at an inflection point in how we think about nonsteroidal anti-inflammatory drugs. I’ve always been skeptical of their risk/benefit ratio, and I’m excited to see a growing body of medical literature supporting my position.
You’ve likely heard the acronym NSAID: nonsteroidal anti-inflammatory drug. NSAIDs work by blocking an important biochemical pathway, which reduces inflammation in the body.
NSAIDs are known by both brand and generic names: Motrin and Advil (ibuprofen), Aleve (naproxen), and Voltaren (diclofenac) are among the most common. We use them to reduce inflammation — more plainly, to reduce the pain associated with inflammation.
I believe any discussion about NSAIDs as pain treatment has to begin with the fundamentals of pain. From a medical perspective, we’ve gotten into the habit of thinking pain is universally bad; something that must be pharmacologically stamped out.
But pain serves a very real purpose. As humans, we’ve evolved to have an exquisitely nuanced and sensitive pain system.
From a simple but effective signal that the pan on the stove is hot and you need to let go of it immediately, to shin pain as you jog that warns you to alter your stride to avoid further injury, pain is useful. It’s an unmistakable communication that our connection to the environment needs to be modified. Our approach to pain relief needs to take this useful communication into account.
Yes, pain can be terribly destructive, but as we discuss NSAIDs, we need to keep an open mind about pain and why it exists in the first place.
Why Are NSAIDs So Popular?
Why are NSAIDs so popular? I’d say it’s because they occupy a sweet spot on the spectrum of pain-relieving drugs.
Tylenol (acetaminophen), when taken at recommended dosages, has very few side effects, though taking too much can be very toxic to the liver. However, Tylenol is not a very effective pain relief modality. On the other hand, medications such as glucocorticoids, which reduce inflammation, or narcotics, which blunt the body’s pain response, are much more powerful but have a much more formidable side effect profile.
In the middle of the spectrum are NSAIDs. With their moderate risk-to-benefit ratio, they’re a compromise and obvious first choice for many.
But in spite of their popularity, I believe NSAIDs shouldn’t be so hurriedly grabbed off the shelf.
My Unpopular Take on NSAIDs
We’re beginning to build a body of information that demonstrates that the acute use of NSAIDs for pain, in fact, may worsen the risk of acute pain becoming chronic pain.
There are some preliminary observational studies looking at temporomandibular joint pain and lower back pain, demonstrating that individuals who had taken NSAIDs early on for pain control were at greater risk for these syndromes developing into chronic pain.
The theory is that early inflammation is an adaptive response we’ve evolved to help our bodies heal in a way to prevent chronic pain from developing. By using NSAIDs to block that route of inflammation, we’re increasing our risk of developing chronic pain.
Certain studies conducted on mice look at neutrophils, a prominent component of the inflammatory response. These studies demonstrate that when an early rise in neutrophils is blunted by NSAID administration, mice are at greater risk of developing a chronic pain response.
While these studies are new and haven’t yet undergone large, full-scale, controlled trials, they do point to a truism that evolution exists for a reason. The fact that we’ve evolved pain mechanisms that do this and we’re still here on Earth suggests it’s an adaptive response that we shouldn’t readily block with drug therapy.
It indicates that, indeed, pain has a purpose.
In addition to the conceptual problem of NSAIDs for acute pain interfering with the healing process, nonsteroidal anti-inflammatory drugs also come with a long list of potential side effects which pose a very real risk.
The Side Effects of NSAIDs
Outside of stunting our body’s adaptive responses, nonsteroidal anti-inflammatory drugs are associated with a very long list of significant side effects: upset stomach, bleeding, ulcers, rising blood pressure, swollen legs, kidney impairment, even increased risk of heart attack.
Next time you take a trip to your local pharmacy, read the list of potential side effects printed on your preferred NSAID. You may be quite shocked!
Today’s Takeaways
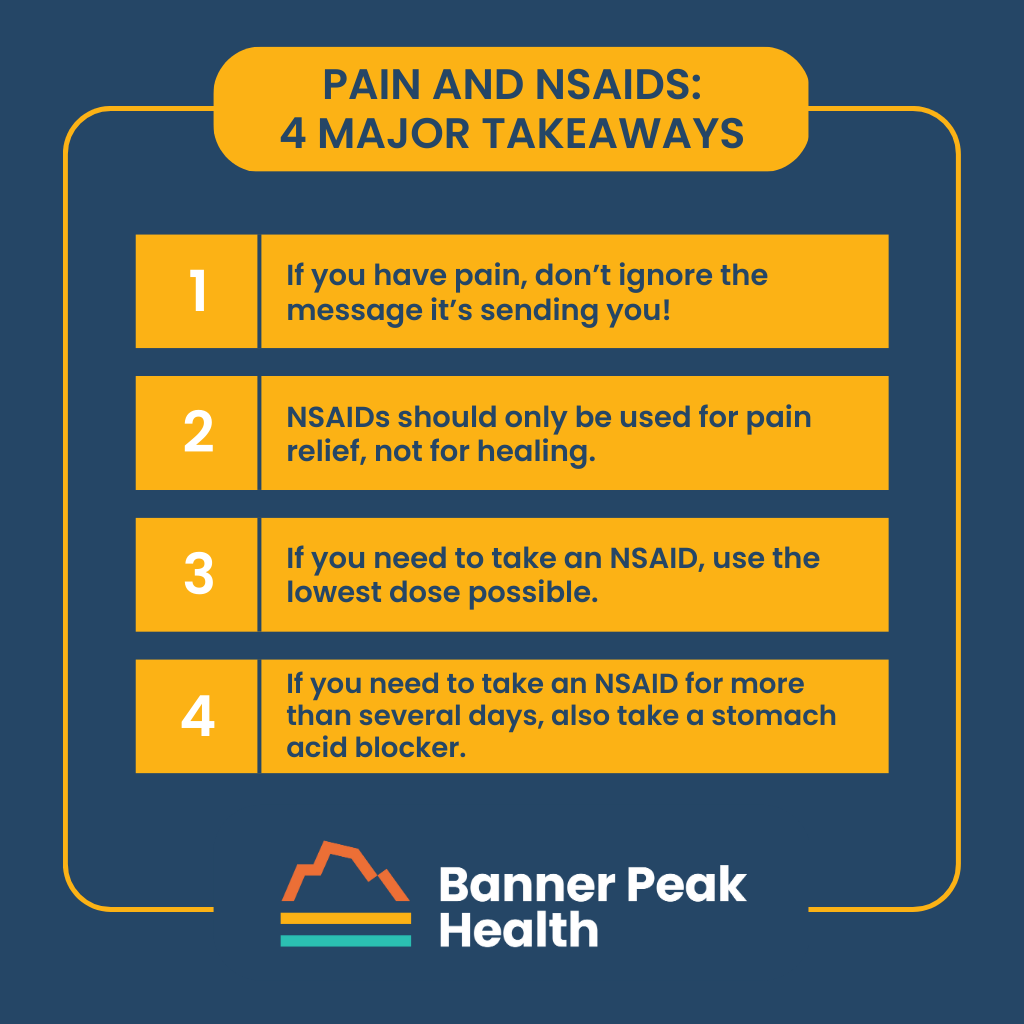
- If you have pain, don’t ignore the message it’s sending you! Pause and reflect. Ask yourself why you have pain in the first place, and see if you can modify the source.
- NSAIDs should only be used for pain relief, not for healing. We now know they actually interfere with overall healing.
- If you need to take an NSAID, use the lowest dose possible for the shortest period of time needed to experience pain relief.
- If you need to take an NSAID for more than several days, also take a stomach acid blocker such as Pepcid (famotidine) to reduce the risk of upset stomach and ulcers.
BONUS TIP: Diclofenac (brand name Voltaren) is available over the counter (without a prescription) in a topical formulation that works well for joint pain near the skin — such as in the hands and feet — with minimal risk of side effects.
The GRAIL Galleri Test: Catching Cancer Before It Catches You
Your DNA is your personal blueprint, the map of you. If that blueprint is disrupted — if your cells become dysregulated — the result may be cancer.
Cancer is a progressive set of errors that occur in the DNA, gradually creating a harmful disorder within certain cells. A simple analogy: the brakes in your car. Maybe the brake pads get a little thin, then the brake line wears out, the brake fluid gets low… and, after enough mechanical disruption, the car crashes.
We want to identify, as soon as possible, when cells are going bad, and avert the “car crash” of cancer.
For decades, medical science has searched for a way to identify these rogue cells at an early stage — for a way to detect cancer early. The benefits of this are obvious: the faster cancerous cells are discovered, the greater the chance the patient will experience a successful treatment and thrive.
But until now, medical technology has been limited in its ability to detect the body’s warning signals of cancer. Diagnoses have been based mostly on specific testing that spots deformed cells, or on scans that reveal an abnormal growth. This means many cancers are not found until they’ve already reached an advanced stage.
How to Detect Cancer Early: GRAIL Galleri® for Early Multi-Cancer Detection
Enter GRAIL Galleri®, a revolutionary multi-cancer early detection test that’s able to detect cancer signals and predict where within the body a signal is coming from.
I’m excited about Galleri testing because it enables us to expose disrupted cells at the DNA level. And we can do it at an earlier stage, often before cancer takes hold.
In cancer detection, it’s critical that our technologies are sensitive and specific. By sensitive, I mean that if cancer is present, there’s a distinct chance of finding it. By specific, I mean that if cancer is not there, we can avoid false positives.
GRAIL Galleri technology is both sensitive and specific, which gives it a powerful edge over other methods of cancer detection. In clinical studies of over 20,000 patients, Galleri showed that it could detect a cancer signal across over 50 types of cancer, far outpacing current methods that screen only for a short list of very specific types.
Perhaps most exciting of all, this new prevention tool can diagnose some of the deadliest forms of cancer at an earlier stage. The more lethal the cancer — lung, esophageal, liver, pancreatic — the faster its cells replicate and shed bits of DNA into the blood. Once that DNA reaches the bloodstream, GRAIL Galleri testing can detect the cancer before physical symptoms appear.
The Galleri test’s sensitivity rate exceeds 75% in the cancers that cause the most U.S. cancer deaths. It’s also highly accurate at localizing the cancer signal, so treatment at the right spot can begin quickly.
And the test’s false positive rate? Only about 0.5% — incredibly accurate compared to a false positive rate as high as 40% for some cancer screening tests.
How Does Galleri Testing Work?
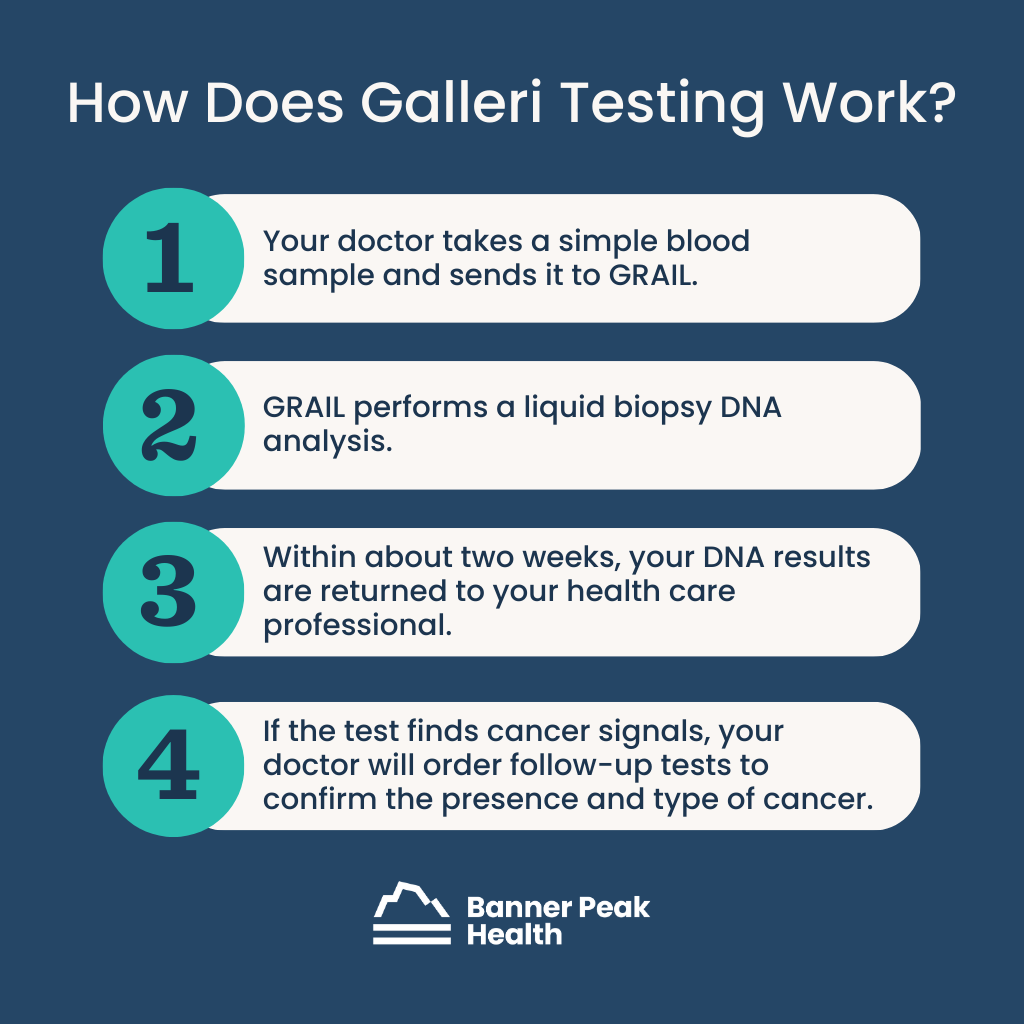
As they multiply, grow, and die, all cells (whether cancer or non-cancer) shed DNA into the bloodstream. As such, GRAIL Galleri testing begins with a simple blood sample.
Your physician requests a Galleri test kit, draws a sample of your blood, and submits it to GRAIL for a liquid biopsy DNA analysis. Within about two weeks, your DNA results are returned to your health care professional.
If the Galleri test has detected a cancer signal, it’s about 90% accurate at pinpointing the organ system where the cancer is located. This prompts the need for more specific follow-up testing, or other diagnostic tests that your doctor may call for, to confirm the presence of cancer in that organ.
If results confirm a form of cancer, GRAIL’s oncology team supports Banner Peak Health to develop a quick, effective treatment plan for the affected area.
Who Should Try the Galleri Test?
The GRAIL Galleri test is recommended for adults with an elevated risk for cancer, which includes people ages 50 and above, as well as those with significant risk factors and/or a family history of cancer. Consult with your doctor to determine the right testing for you.
When it comes to GRAIL’s Galleri test, I’m excited to use a simple blood test that can help detect cancer. The greatest benefit? We can begin early treatment, before that cancer has a chance to grow and spread.
Want to learn more about GRAIL’s Galleri test? Start here.
Are You Eligible for a COVID Booster in California?
Are you eligible for a COVID booster in California? The short answer is probably yes. If you’re over the age of five and at least two months removed from your last dose, you’re likely eligible for a COVID booster — but do you need one?
Unfortunately, this topic has become extremely complicated. Finding informed, unbiased, and explicit information about COVID boosters can be challenging.
To understand whether you need a booster, you’ll first need some context.
Are We Out of the Weeds With COVID?
Here’s the simple truth: the COVID pandemic isn’t over. No matter what you may hear from a politician — or, frankly, what you want to believe — COVID is still very much with us, at the current rate killing over 150,000 Americans per year, or three times the rate of influenza’s worst mortality year in the past decade.
Hypothetically, if a new disease emerged with the same current mortality rate as COVID, I think we’d respond much more seriously. The mental, emotional, and political baggage associated with COVID has led many to grow weary of responding to it.
Thankfully, vaccine technology has already saved millions of lives. COVID vaccines are safe and effective at reducing the risk of hospitalization and death, which is particularly important for those advanced in age or otherwise at elevated risk. Of course, that doesn’t mean there haven’t been challenges in understanding this evolving technology.
In the early days of the vaccine, we hoped herd immunity would disrupt the spread of COVID, which has since proven not to be the case. COVID vaccines have been more effective at saving lives than providing complete protection from becoming infected.
This unmet expectation has colored the vaccine debate with cynicism and futility. We must learn to appreciate vaccine technology for what it is, what it can do, and how it actually works. Learning is the first step to making informed decisions about your health.
What Is a COVID Booster and How Does It Work?
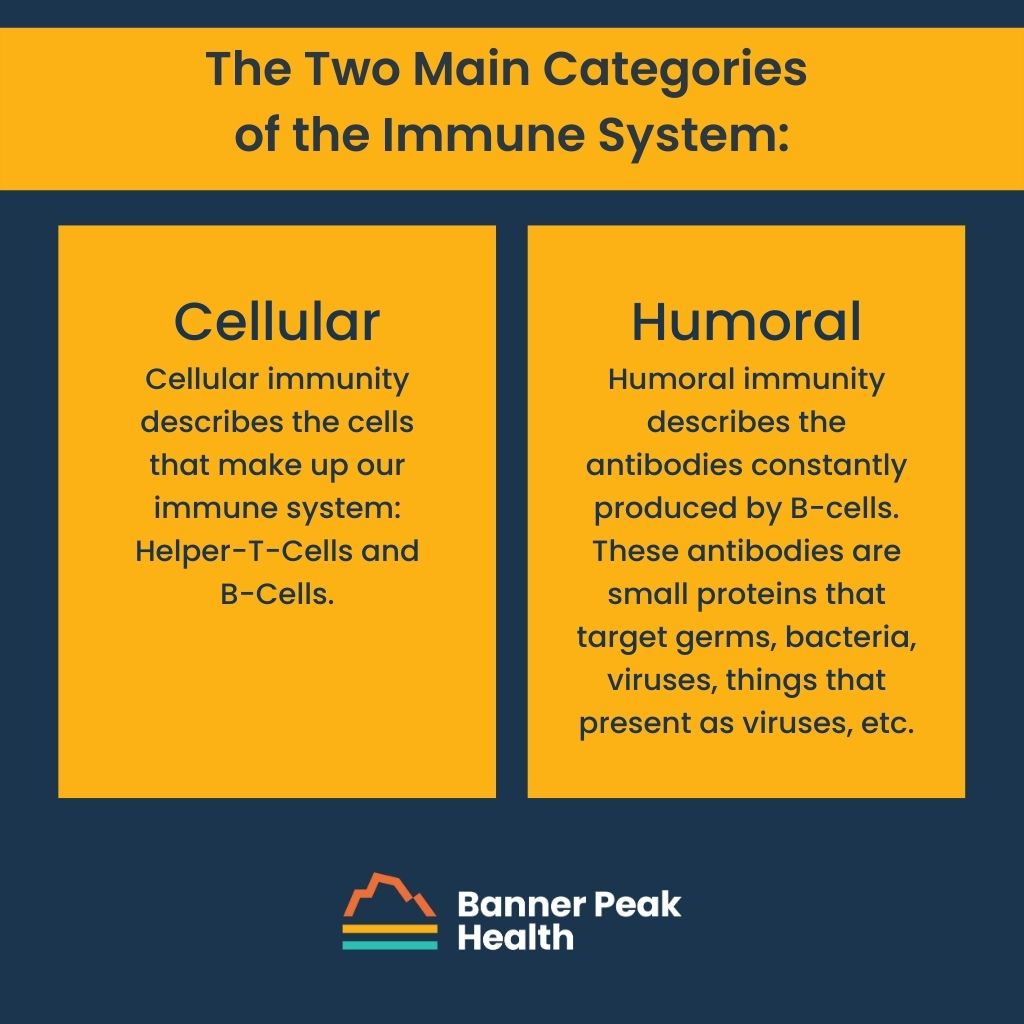
Your immune system can be divided into two broad categories: cellular immunity and humoral immunity.
Cellular immunity describes the cells that make up our immune system. There are several kinds of cells, but let’s cover the basics.
- T-cells sense infection and recruit other immune cells to fight. When you get a vaccine or booster, T-cells lay out the game plan for the rest of your adaptive immune system. Once they encounter a particular virus or bacteria, T-cells will remember that virus or bacteria forever. If they run into it again, they can flip back in the playbook to remember which cells to notify.
- B-cells produce antibodies that fight bacteria and viruses. These antibodies, found in the bloodstream, are temporary.
Humoral immunity describes the antibodies constantly produced by B-cells. These antibodies are small proteins that target germs — bacteria, viruses, things that present as viruses, etc.
Cellular and humoral immunity are the basic mechanisms of vaccine technology.
Most COVID vaccines are mRNA vaccines. Messenger RNA, or mRNA, is genetic material that acts as an instruction manual for protein synthesis. An mRNA vaccine tells your immune system to create proteins that look like part of SARS-CoV-2: the virus that causes COVID. Your T-cells sense this “virus,” alert your B-cells to produce antibodies, and store that information for the future.
Again, your immune cells will remember this virus forever, but the quantity of these specific antibodies will not stay elevated forever. This process is a mock battle against COVID, creating temporary antibodies that will work against the real thing.
Why only temporary? Well, by the end of our lives, we’ll have been exposed to thousands, if not millions of unique germs. If we permanently made the maximum amount of antibodies for every germ we encountered, there wouldn’t be any room in our bloodstream for, well, blood.
Because of this, there is relatively high turnover of antibodies within the bloodstream. Antibodies associated with COVID — from what we can tell — remain at peak levels in our circulation for only a matter of months. These antibodies are part of our humoral immunity.
Think of the COVID virus as an army seeking to invade your homeland. Your immune system provides several layers of defense. Think of your antibodies as your standing military with many troops stationed at the border ready to prevent any viruses from even crossing. Your cellular immunity can be thought of as your reserves, ready to be called up but requiring several days to get to the front lines with the possibility of a bigger battle until they arrive.
Periodic booster vaccinations can keep the number of troops at the border at a high enough level to reduce the possibility of experiencing any symptoms or serious health outcomes in the event of a COVID invasion.
Who Should Get a COVID Booster Shot?
To continue the battle analogy, those whose military isn’t quite as robust will get more benefit from the added strength provided by more frequent vaccinations.
Those with weakened immune systems due to advanced age or pre-existing medical conditions should get COVID boosters more regularly. This list also includes pregnant women.
But what about healthy individuals, kids, and young adults?
The appeal of the booster, and the vaccine in general, is a greatly reduced risk of hospitalization and death. In kids and young adults, this risk is already incredibly low. The reward (protection against hospitalization and death) doesn’t outweigh the extremely low risk associated with vaccines (rare autoimmune reactions such as mild cases of myocarditis).
In short, boosters aren’t necessary for low-risk individuals. However, they are still very worthwhile for those at high risk.
Medicine is all about weighing individualized risk with individualized benefits. Your risk should be considered against the potential benefits of medical intervention, including a vaccine. Unfortunately (and perplexingly), COVID vaccines have become a controversial topic. This puts physicians in a strange position when giving medical advice.
Luckily, concierge medicine ensures an intimate, individualized experience. This model is conducive to the aforementioned concept: weighing individualized risk with individualized benefits. Your specific needs are our priority.
As always, if you have any questions or concerns, don’t hesitate to reach out.
We Need More Empathy in Healthcare
I’m always trying to learn what patients value in their relationship with their primary care doctor.
Whenever I ask people what they appreciate about their physician, I usually hear the same responses: “My doctor is thoughtful, thorough, energetic, a good listener, etc.” No one ever says, “I like that my doctor is fast.”
In fact, the converse is true. Always, without fail, people remark to me that their interactions with their physicians are too hurried. This lack of time has markedly denigrated their relationship with their doctor.
Unfortunately, electronic health records have only amplified those time-pressured frustrations. People often complain that their physicians don’t make eye contact, but instead stare down at their keyboard, frantically typing.
“If my doctor ever develops a bald spot, I’ll be the first to know,” patients joke.
At the end of the day, patients want an empathetic healthcare experience. But what does that look like in practice?
An Empathetic Healthcare Experience vs. The Reality of Conventional Care
Envision the ideal relationship with your doctor. What do you imagine? Maybe you want more one-on-one time, or more eye contact. Perhaps you’d feel more comfortable bringing up a health concern if your doctor didn’t seem so distracted!
In some ways, people want a time machine that will take them back to a perhaps mythical era — when doctors weren’t distracted by technology, they weren’t constantly on a time-crunch, and they certainly weren’t assigned to different patients every year due to insurance transitions.
How an Alternative Payment Model Can Benefit Both Physicians and Patients
Concierge medicine is an alternative payment model for funding the highest-quality healthcare. By using this model, we can recapture, reinvent, and preserve that old-school physician-patient relationship that enables patients to be heard.
Of course, this approach to medicine doesn’t just benefit patients. Physicians also suffer when they’re trapped in a time-pressured environment. They’re unable to give their intellectual and emotional all to their patients — they can’t research cases, discuss treatment options with other doctors, or even process their own thoughts.
Concierge medicine provides a bridge between the patient and the physician — everyone wins. This alternative payment model allows us (pun incoming) to go back to the future.
Why Is Empathy So Important in Healthcare?
Most of us have heard of the Golden Rule: “Do unto others as you would have them do unto you.” This applies to many areas of life, but especially healthcare.
We understand that the fundamental truth of the Golden Rule is empathy. Empathy can manifest in a healthcare setting from the moment you pick up the phone to schedule your first appointment. You want to be acknowledged as a person with unique emotions, concerns, and goals. Wouldn’t it be nice to interact with a person (not a machine) who treats you as a fellow human being, kindly, patiently, and respectfully?
Unfortunately, we as patients have experienced that following the Golden Rule is impossible in the traditional healthcare system because of time and insurance constraints. That’s why we founded Banner Peak Health in the first place. We’ve created a clinic where we’re free to abide by the Golden Rule and provide the care we want and expect our own friends and family to receive.
What to Look for in a Healthcare Practitioner
On the hunt for an empathetic physician? Here are a few questions to ask along the way:
How do they listen to you? How do they treat or evaluate you? The answer should be: patiently and attentively. Who wants to feel like their doctor is just going through the motions? Your physician should be thorough and should advocate for your comfort.
How do they communicate with you and educate you? Feeling understood is paramount, and a physician who talks down to you can be intimidating and insulting — and definitely not conducive to a strong patient-physician relationship.
Being truly seen and heard by your doctor helps you feel like your well-being is their first and foremost priority — because it should be.
Why Preventative Care Is the Ultimate Health Investment
I’ve heard people proudly declare that they haven’t seen a doctor in two years, five years, even seven years. Implicit in this is the notion that the less time you spend with a doctor, the healthier you are.
I vehemently disagree with this philosophy.
In fact, when I meet people who boast this, my retort is, “Do you ever change the oil in your car?”
If you go too long without an oil change, it can lead to a complete engine shutdown that destroys your car engine. Clearly, the human body is infinitely more complex than an automobile, and just like getting an oil change, we need to be proactive in building and maintaining our health.
Silently Saving Lives: Why Preventative Care Is Important
I feel prevention and the role it plays in our current healthcare system is similar to a forgotten hero.
Everyone identifies the surgeon as a life-saving hero when he removes an inflamed appendix — but the primary care physician who spends years caring for a large panel of patients, working diligently to help them stop smoking, lose weight, and treat diabetes, may not get the recognition he deserves.
That physician’s careful, diligent work saves lives, too, probably dozens, by minimizing the risks of cardiovascular disease. But he and his patients will never know which individual lives were saved.
In order of magnitude, the health benefit of this form of care may be much greater than that of a surgeon who saves one life at a time. That isn’t to belittle the surgeon’s contribution, but to emphasize the value and importance of preventative healthcare, even though it may be hidden.
Our current fee-for-service healthcare model encourages a triage-based system where doctors are stuck having to push prevention to the bottom of the priority list. Many people can’t fully benefit from preventative healthcare in this type of system.
What Is Preventative Care?
I believe preventative care goes fundamentally much deeper than people realize. Most people are familiar with what I refer to as traditional preventative care: mammograms, pap smears, colonoscopies, chest CT scans, and prostate cancer screening. These are the visible, medicalized forms of preventative care.
These, I believe, make up only the small tip of the pyramid.
At its most essential, preventative care simply refers to the efforts we make to prevent disease and illness. Prevention isn’t just what you do in a medical environment once a year. It’s how you live your life every single day.
The Peak of Prevention
When I think of preventative care, I think of a pyramid. I call this pyramid the Peak of Prevention, and it has three levels of preventative care: Traditional, Cardiovascular, and Lifestyle. Each level relates to a progressively deeper, more time-consuming commitment to your health and to disease prevention.
The first level of the pyramid is the Traditional level.
Most people have access to and are familiar with this level of preventative care. As I mentioned before, it includes mammograms, prostate cancer screenings, pap smears, and colonoscopies.
The second level is the Cardiovascular level.
You may have heard about some of the preventative care performed at this level, like something to do with cholesterol or blood pressure. But testing isn’t routine, and prevention requires more commitment. If we want to, we can drill down and look at specific risk factors, order detailed lipid testing, and explore different heritable traits.
At the Cardiovascular level, we can go deeper than you’ve probably ever gone in the care of previous doctors. This is where I’ll tell you, “You’re here to let me help you prevent bad things, and that’s the work we’ll do together.”
I may also warn you, as I do with all new patients, that I may very well make you work harder than your other doctors have. I do this because prevention is an investment in time — but it’s an investment you’re making to reduce problems down the line.
Finally, the foundation of the pyramid — the Lifestyle level — is the bedrock on which everything rests.
It’s an area you may not have explored in great detail with any prior doctors, and a lot of it has to do with how we live our lives day to day.
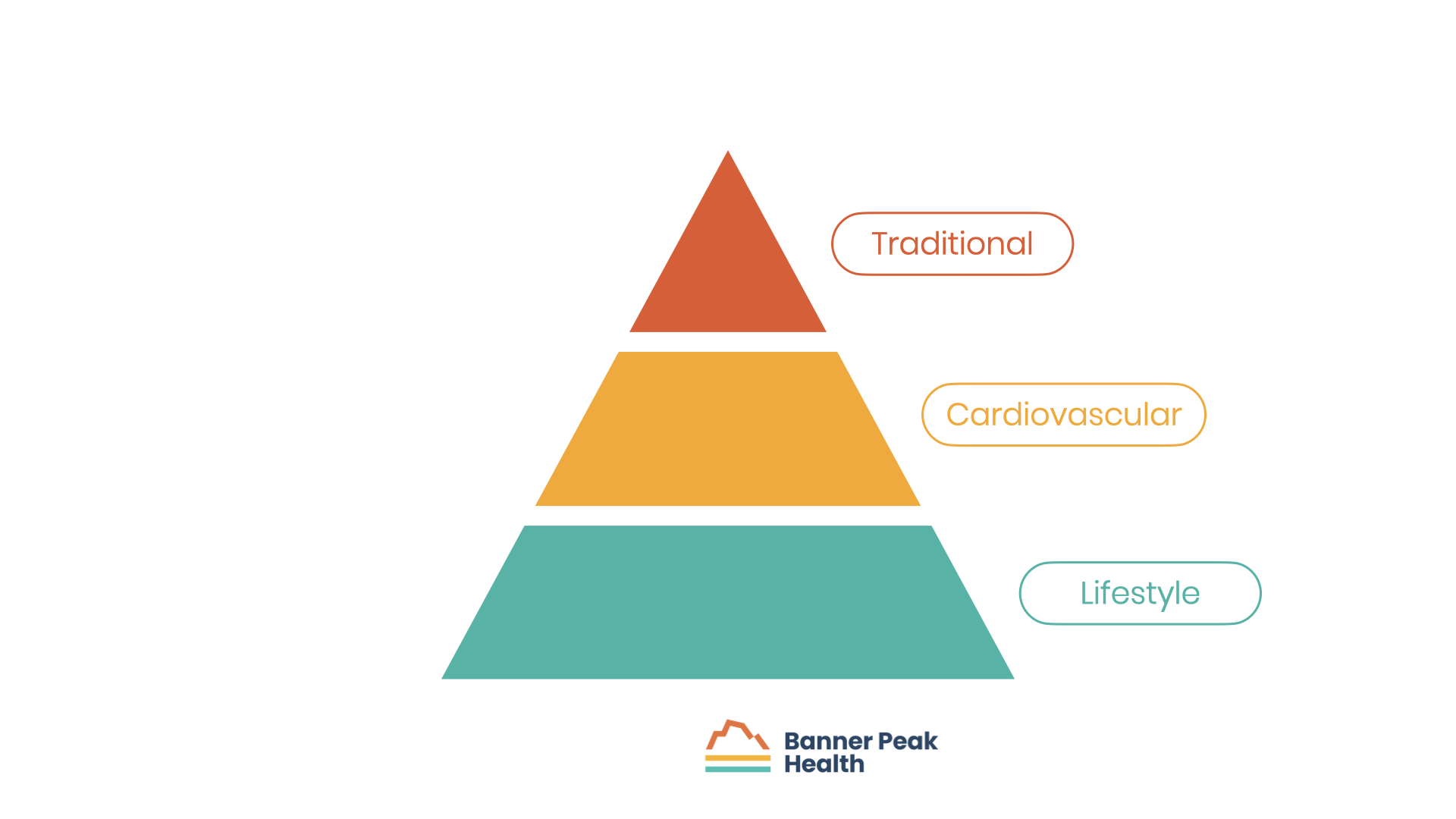
A very important part of the foundation is the quality and quantity of our sleep. I often joke that in my business: all roads lead to Rome, and Rome is sleep.
Another part is eating: how we eat, what we eat, etc. Eating expands into the topic of exercise, aerobic capacity, strength training, and preserving muscle mass as we age.
Finally, we’ll discuss stress and how we can cope with it. We’re all aware of our metaphorical stress inbox, but are we aware of and making proper use of our stress outbox?
Understanding and building a healthy relationship with the Peak of Prevention is crucial to long-term health and wellness. It’s the core of the work I do with all my patients.
Recognize the Importance of Preventative Care and Invest in Yourself
The real foundation of preventative care is a conceptual shift that responsibility for that care belongs to the individual rather than the healthcare system. It requires self-education, ownership, and commitment.
For anything to have value, you need to own it and invest in it. You have to invest in yourself.
The key to successful prevention is understanding that it’s a mindset. If you want to receive from your body, you have to give to your body. This becomes truer with each passing year.
Prevention, like life, is a marathon, not a sprint. It’s not an event — it’s a way of life.
COVID: The New Annual Holiday Tradition?
We've now gone through three holiday seasons confronting COVID. Unbelievable, but I have double-checked my math.
Each year, the COVID pandemic has been at a unique phase in terms of treatment options and lethality. However, each holiday season illustrates how important human behavior is in determining the course of the pandemic. The basic human desire to gather and celebrate with our friends and families works against us by accelerating the rate of infections. Again, the year 2022 demonstrates this trend.
COVID home antigen tests are a game-changer, providing us with a tool to determine rapidly and conveniently who is infected. Yet, we have lost the ability to count how many people are infected. For tracking the pandemic, we now rely on other metrics including measuring the number of viral particles shed into the sewage system.
Based on this form of data, the Bay Area is now experiencing more COVID cases than during any other time in the pandemic. I fear that this astounding statistic is not being adequately communicated. Because we have a high rate of vaccination and access to medical treatments for COVID, the rates of hospitalizations and death are not record-setting but have been rising rapidly since Thanksgiving.
What should we do about the situation? That depends on your degree of risk for a bad outcome from COVID.
Those over 50 years old, pregnant, or with multiple or severe medical conditions should take action to reduce their risk. The most basic advice would be to wear a mask when indoors around large numbers of other people — not a stylish cloth mask or paper surgical mask but an effective mask with an N95 rating or similar.1
Simple masks help reduce the spread of germs from you to other people. However, at this stage in the pandemic with most people not wearing any masks, you need a high-quality mask to avoid inhaling their germs. I am purposely using the general term “germs” rather than "the COVID virus". As you have heard, we are in the midst of a triple pandemic with rising rates of influenza, respiratory syncytial virus (RSV) and COVID. Wearing a mask will reduce your risk of contracting any of these illnesses.
Eating indoors now represents a growing risk.
Observing the rapid acceleration of COVID infections, I have tried to avoid or minimize eating indoors at restaurants. When my family hosted a Thanksgiving dinner for 13 people, I asked everyone to perform a home COVID antigen test that day before gathering. I highly recommend this technique for others as well. First, this reduces the risk of spreading COVID. Secondly, this allows me to relax a bit and not worry about creating a super-spreader event.
A new Bivalent COVID booster was released this past Fall. This is the first booster to include a newer Omicron descendant variant in addition to the original Wuhan variant. Since then, laboratory and clinic data have shown that adding this booster can further reduce the risk of infection and serious health outcomes. In fact, for many people, being fully vaccinated and boosted against COVID has reduced its danger to that of influenza.
Unfortunately, the risk of mild cases persists but can be reduced by being up to date with COVID boosters.
Should everyone get the new Bivalent COVID booster? Not necessarily. I believe that for most low-risk people, younger than 50 years old, non-pregnant without serious illness, the marginal benefit does not exceed the very rare potential for a vaccine side effect. For this group of people, who have already had two, three, or four vaccines and possibly a case of COVID infection, you can take a pause from further vaccination for now.
On the other hand, everyone else should get the new Bivalent COVID booster. Please wait 2-3 months after a previous booster or COVID infection.
This was my third-year asking patients to reduce their COVID risk during the holiday season. This has become a holiday tradition! We can count our blessings that the risk of serious illness from COVID has been remarkably reduced during this time. As many of you know, I had COVID in September. Fortunately, it was a mild case. Nonetheless, I was in bed for a few days, had to be out of the office for a 10-day period, and still have a lingering, dry cough.
I believe getting another COVID booster, being a more diligent mask wearer, and testing before family gatherings represent a modest inconvenience that I can endure to reduce my chance of getting COVID again.
Everyone can — and should — weigh their own risks and benefits.