Are you eligible for a COVID booster in California? The short answer is probably yes. If you’re over the age of five and at least two months removed from your last dose, you’re likely eligible for a COVID booster — but do you need one?
Unfortunately, this topic has become extremely complicated. Finding informed, unbiased, and explicit information about COVID boosters can be challenging.
To understand whether you need a booster, you’ll first need some context.
Are We Out of the Weeds With COVID?
Here’s the simple truth: the COVID pandemic isn’t over. No matter what you may hear from a politician — or, frankly, what you want to believe — COVID is still very much with us, at the current rate killing over 150,000 Americans per year, or three times the rate of influenza’s worst mortality year in the past decade.
Hypothetically, if a new disease emerged with the same current mortality rate as COVID, I think we’d respond much more seriously. The mental, emotional, and political baggage associated with COVID has led many to grow weary of responding to it.
Thankfully, vaccine technology has already saved millions of lives. COVID vaccines are safe and effective at reducing the risk of hospitalization and death, which is particularly important for those advanced in age or otherwise at elevated risk. Of course, that doesn’t mean there haven’t been challenges in understanding this evolving technology.
In the early days of the vaccine, we hoped herd immunity would disrupt the spread of COVID, which has since proven not to be the case. COVID vaccines have been more effective at saving lives than providing complete protection from becoming infected.
This unmet expectation has colored the vaccine debate with cynicism and futility. We must learn to appreciate vaccine technology for what it is, what it can do, and how it actually works. Learning is the first step to making informed decisions about your health.
What Is a COVID Booster and How Does It Work?
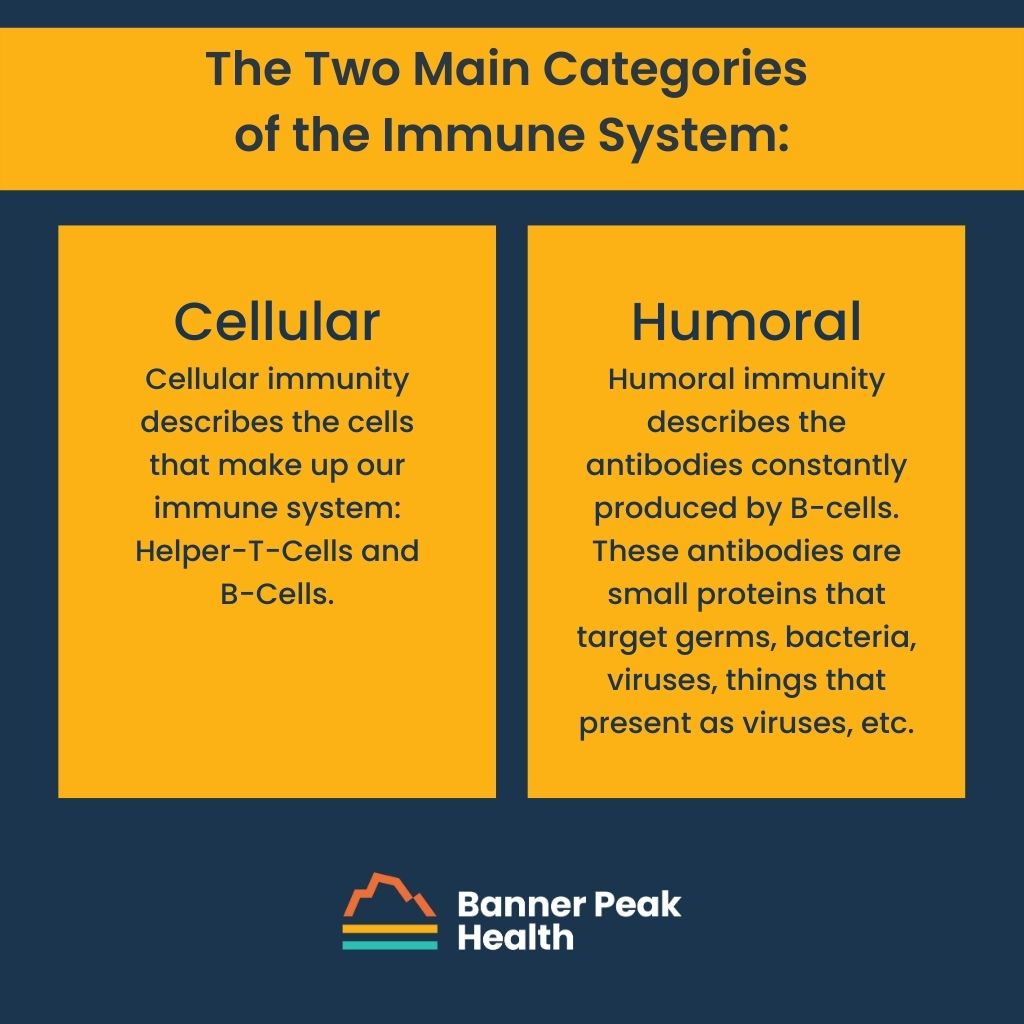
Your immune system can be divided into two broad categories: cellular immunity and humoral immunity.
Cellular immunity describes the cells that make up our immune system. There are several kinds of cells, but let’s cover the basics.
- T-cells sense infection and recruit other immune cells to fight. When you get a vaccine or booster, T-cells lay out the game plan for the rest of your adaptive immune system. Once they encounter a particular virus or bacteria, T-cells will remember that virus or bacteria forever. If they run into it again, they can flip back in the playbook to remember which cells to notify.
- B-cells produce antibodies that fight bacteria and viruses. These antibodies, found in the bloodstream, are temporary.
Humoral immunity describes the antibodies constantly produced by B-cells. These antibodies are small proteins that target germs — bacteria, viruses, things that present as viruses, etc.
Cellular and humoral immunity are the basic mechanisms of vaccine technology.
Most COVID vaccines are mRNA vaccines. Messenger RNA, or mRNA, is genetic material that acts as an instruction manual for protein synthesis. An mRNA vaccine tells your immune system to create proteins that look like part of SARS-CoV-2: the virus that causes COVID. Your T-cells sense this “virus,” alert your B-cells to produce antibodies, and store that information for the future.
Again, your immune cells will remember this virus forever, but the quantity of these specific antibodies will not stay elevated forever. This process is a mock battle against COVID, creating temporary antibodies that will work against the real thing.
Why only temporary? Well, by the end of our lives, we’ll have been exposed to thousands, if not millions of unique germs. If we permanently made the maximum amount of antibodies for every germ we encountered, there wouldn’t be any room in our bloodstream for, well, blood.
Because of this, there is relatively high turnover of antibodies within the bloodstream. Antibodies associated with COVID — from what we can tell — remain at peak levels in our circulation for only a matter of months. These antibodies are part of our humoral immunity.
Think of the COVID virus as an army seeking to invade your homeland. Your immune system provides several layers of defense. Think of your antibodies as your standing military with many troops stationed at the border ready to prevent any viruses from even crossing. Your cellular immunity can be thought of as your reserves, ready to be called up but requiring several days to get to the front lines with the possibility of a bigger battle until they arrive.
Periodic booster vaccinations can keep the number of troops at the border at a high enough level to reduce the possibility of experiencing any symptoms or serious health outcomes in the event of a COVID invasion.
Who Should Get a COVID Booster Shot?
To continue the battle analogy, those whose military isn’t quite as robust will get more benefit from the added strength provided by more frequent vaccinations.
Those with weakened immune systems due to advanced age or pre-existing medical conditions should get COVID boosters more regularly. This list also includes pregnant women.
But what about healthy individuals, kids, and young adults?
The appeal of the booster, and the vaccine in general, is a greatly reduced risk of hospitalization and death. In kids and young adults, this risk is already incredibly low. The reward (protection against hospitalization and death) doesn’t outweigh the extremely low risk associated with vaccines (rare autoimmune reactions such as mild cases of myocarditis).
In short, boosters aren’t necessary for low-risk individuals. However, they are still very worthwhile for those at high risk.
Medicine is all about weighing individualized risk with individualized benefits. Your risk should be considered against the potential benefits of medical intervention, including a vaccine. Unfortunately (and perplexingly), COVID vaccines have become a controversial topic. This puts physicians in a strange position when giving medical advice.
Luckily, concierge medicine ensures an intimate, individualized experience. This model is conducive to the aforementioned concept: weighing individualized risk with individualized benefits. Your specific needs are our priority.
As always, if you have any questions or concerns, don’t hesitate to reach out.

Barry Rotman, MD
For over 30 years in medicine, Dr. Rotman has dedicated himself to excellence. With patients’ health as his top priority, he opened his own concierge medical practice in 2007 to practice medicine in a way that lets him truly serve their best interests.