The Benefits of Resistance Training for Women: A Woman’s Guide to Lifelong Strength
“I don’t want to bulk up.”
We hear female patients express this concern nearly every week. Despite mounting evidence about the benefits of resistance training for women, this misconception persists.
Women don’t have the same testosterone levels as men, which means they can’t build as much muscle mass as men do. The fear of accidentally becoming a bodybuilder from lifting weights twice a week is physiologically unfounded.
Resistance training actually delivers stronger bones, balanced hormones, and metabolic health that protects against diabetes and cardiovascular disease. These benefits of resistance training for women become even more important as they navigate their 30s, 40s, and beyond.
Why Women Can’t Build Massive Muscles
Women have lower testosterone levels compared to men: the primary anabolic hormone responsible for muscle growth.
Testosterone increases skeletal muscle fiber size and drives protein synthesis. Without high levels of this hormone, building substantial muscle mass becomes extremely difficult, even with intense training.
Your hormonal fluctuations actually hinder muscle building in certain ways. During your menstrual cycle’s luteal phase, progesterone’s catabolic effects blunt muscle protein synthesis. These natural variations, particularly pronounced during perimenopause, influence protein metabolism in ways that make “accidental” muscle gain nearly impossible.
When we recommend resistance training using weights, resistance bands, or bodyweight to enhance muscle mass, we’re not suggesting you’ll become a bodybuilder. We’re offering you a path to better health.
The conversation has shifted over the past decade. Where women once avoided the weight room, they now seek guidance on getting started. They want weight loss, muscle definition, and strength, recognizing that resistance training delivers all three without unwanted bulk.
 The Benefits of Resistance Training for Women
The Benefits of Resistance Training for Women
While toned arms and a stronger core are welcome benefits, the real value of resistance training for women lies beneath the surface.
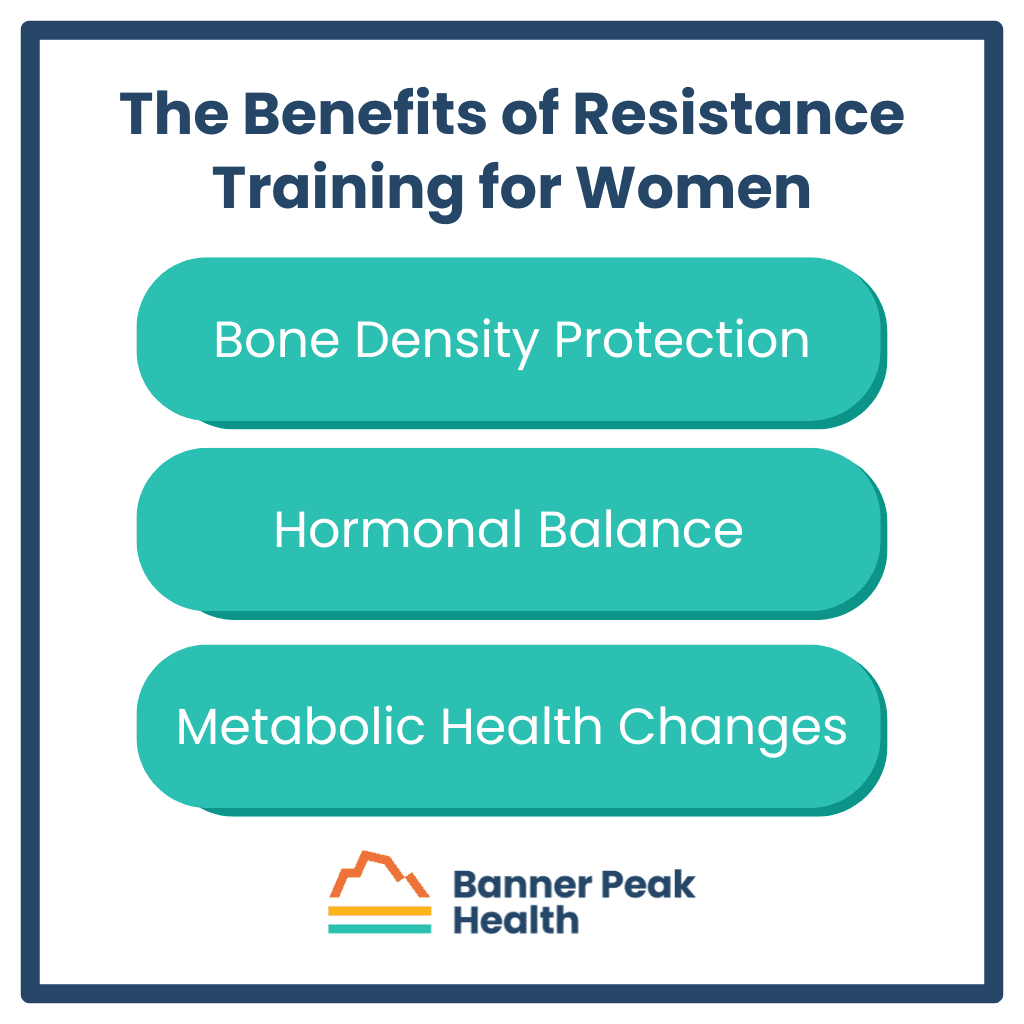
Bone Density Protection
Women face a higher osteoporosis risk than men, particularly after menopause. Progressive resistance training leads to improvements in bone density at important sites: the femoral neck, lumbar spine, and total hip. We measure these exact areas during bone density tests.
These improvements occur in both pre- and postmenopausal women. Combining resistance training for women with weight-bearing, high-impact aerobic exercises produces the best results for bone health.
Hormonal Balance
Resistance training for women influences hormones in ways that address menopausal symptoms. Regular training reduces LH and FSH levels, potentially reducing vasomotor symptoms like hot flashes.
It increases beneficial hormones that typically diminish with age:
- Estradiol
- Growth hormone
- IGF-1
- DHEAS
These hormonal improvements translate to increased lean body mass and sometimes lower blood pressure. These changes improve quality of life during menopause and beyond.
Metabolic Health Changes
Resistance training for women improves insulin sensitivity and cholesterol profiles while decreasing fat mass and increasing lean body mass.
For women with diabetes or prediabetes, these benefits matter. Diabetes is associated with low muscle strength and accelerated functional decline. Resistance training counters these risks.
What Happens During and After Resistance Training for Women
Understanding what occurs in your body during resistance training helps explain its powerful effects.
Resistance training for women improves metabolic rate by increasing lean body mass: your most metabolically active tissue. This fat-free mass elevates your resting metabolic rate, meaning you burn more calories even at rest.
This metabolic boost may decrease weight gain over time. Some studies suggest resistance training enhances metabolic rate through increased post-exercise oxygen consumption and improved mitochondrial function. Your cells literally produce energy more efficiently.
Resistance Training Through Your 30s, 40s, and Beyond
As women move through their 30s and 40s into perimenopause, resistance training becomes even more important, but the approach needs modification.
The biggest consideration as we age is minimizing injury risk. For those just starting out or returning after years away, beginning with lower intensities and higher repetitions prevents injury.
Adequate protein intake becomes important for older women. You need these building blocks of muscle to augment strength gains. Without sufficient protein, your body can’t effectively respond to training stimuli.
Mental and Emotional Changes
The mental health benefits of resistance training for women often surprise our patients.
The act of training itself triggers neurobiological changes that enhance mental well-being. For older women, especially those with pre-existing mental health conditions, improvements in depression and anxiety can be substantial.
People observe these effects regardless of whether they achieve strength gains.
Getting Started Safely
Most women want to start resistance training, but don’t know how to proceed safely.
We recommend working with a personal trainer or in a class setting, at least initially. Poor form leads to injury, derailing progress before it begins.
At Banner Peak Health, we maintain a list of personal trainers with whom we work closely. These professionals work one-on-one with patients to develop programs that fit individual schedules and fitness levels.
You don’t need extensive equipment. Our recommended trainers build effective programs using minimal tools:
- Resistance bands for travel
- TRX systems that hang over any door
- Bodyweight exercises requiring no equipment
The key is making it work with your busy schedule. Even using resistance bands for twenty to thirty minutes at home is beneficial. When traveling, throw the bands in your suitcase.
Today’s Takeaways
Resistance training for women builds a foundation for lifelong health, from protecting bone density to balancing hormones to improving metabolic function.
You don’t need a gym membership or expensive equipment to start. You just need commitment, proper guidance, and patience.
At Banner Peak Health, we connect you with personal trainers who understand your health history, work with physical therapists when needed, and monitor your progress through regular check-ins. Schedule an appointment to discuss a personalized strength training plan that fits your life, goals, and fitness level.
Vaginal Estrogen: A Doctor’s Guide to Benefits, Risks, and the Black Box Warning
Many women avoid vaginal estrogen therapy because of concerns about hormone treatments. These concerns stem from frightening media coverage and FDA black box warnings.
However, vaginal estrogen remains our most effective treatment for common and disruptive menopausal symptoms.
Understanding Vaginal Estrogen
Despite common misconceptions, vaginal estrogen is absorbed minimally — almost entirely within vaginal tissues, with little to none entering your bloodstream.
Vaginal estrogen acts locally rather than systemically. Unlike estrogen patches or pills that affect your entire body, vaginal estrogen works only where applied.
This local action means vaginal estrogen has few to no contraindications. It’s even safe for many women with a history of breast cancer.
Why Consider Vaginal Estrogen Therapy?
Vaginal estrogen treats several common symptoms that fall under Genitourinary Syndrome of Menopause (GSM):
- Vaginal dryness
- Recurrent urinary tract infections
- Pain during intercourse (dyspareunia)
For these conditions, vaginal estrogen is the most effective treatment available. Relief is typically excellent, with many women reporting improvement in their symptoms.
When treating recurrent UTIs, vaginal estrogen provides additional benefits. It helps avoid repeated antibiotic use, reducing risks of antibiotic resistance and side effects from those medications.
Demystifying the Black Box Warning for Vaginal Estrogen
The FDA places a black box warning on all estrogen products. This warning states that unopposed estrogen (without progesterone) increases the risk of:
- Endometrial cancer in women with a uterus
- Stroke and blood clots
- Dementia in women over 65
- Pulmonary embolism and heart attack
- Breast cancer when combined with progestin
Modern research has debunked most concerns in this warning, even for systemic estrogen therapy. The book “Estrogen Matters” provides an excellent review of this evidence.
More importantly, this warning doesn’t apply to vaginal estrogen. Since vaginal estrogen isn’t absorbed systemically, it doesn’t create the risks associated with whole-body exposure.
A movement exists to remove this warning from vaginal estrogen products. Dr. Rachel Rubin, recently featured on Dr. Peter Attia’s podcast, leads physician groups like “Unboxing Menopause” and “Let’s Talk Menopause” that meet with the FDA to advocate for this change. These groups argue that the warning prevents women from accessing effective treatment for their symptoms by scaring them with information that doesn’t apply.
In July 2025, these advocacy efforts gained significant momentum when FDA Commissioner Dr. Marty Makary convened a panel of experts who overwhelmingly urged the agency to remove the black box warnings from vaginal estrogen products.
While no formal action has been taken yet, Makary promised the FDA would “take a hard look at” removing the warning and indicated they’re trying to move faster than typical government processes.
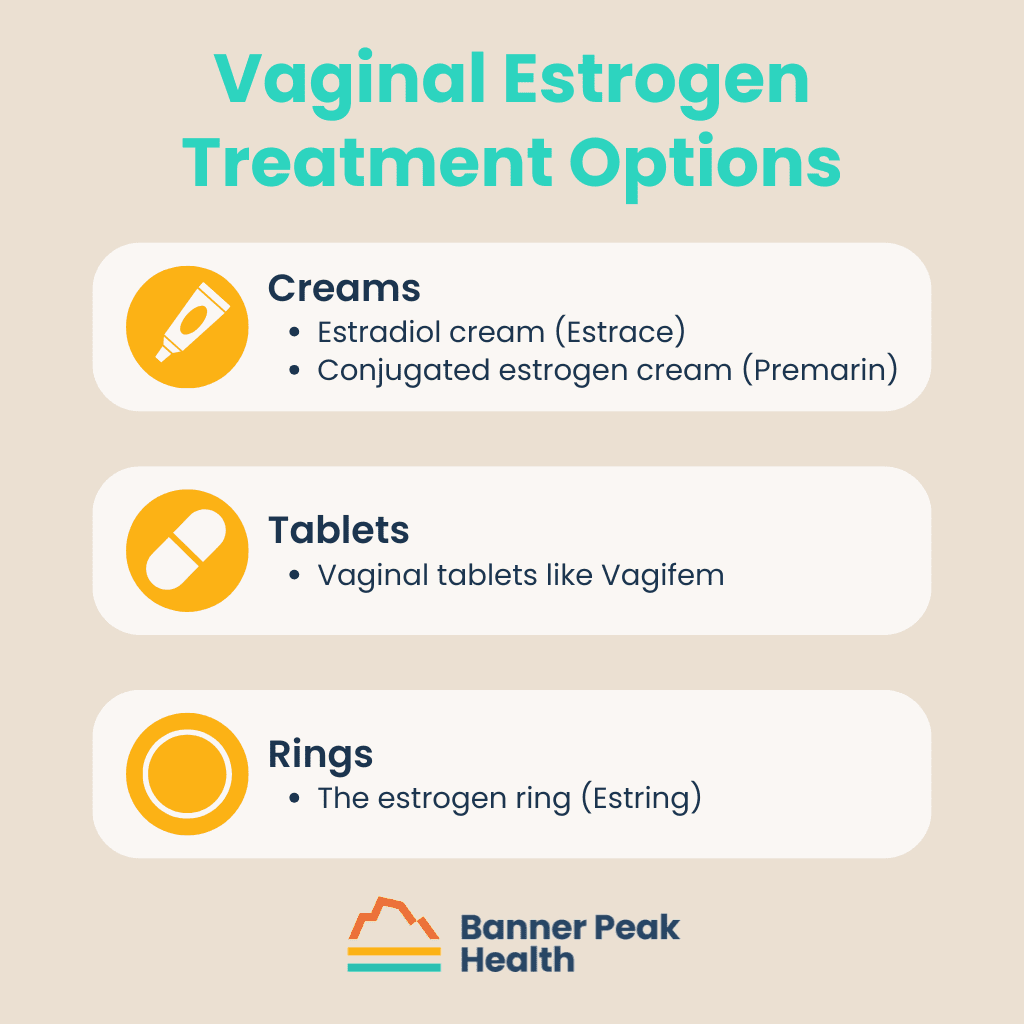
Vaginal Estrogen Treatment Options
If you decide vaginal estrogen is right for you, several options exist.
Creams
Two main types of vaginal estrogen cream are available:
Tablets
Vaginal tablets like Vagifem are a less messy alternative to creams.
Rings
The estrogen ring (Estring) is an alternative option.
I typically recommend vaginal tablets for most patients because they’re less messy and easier to use. However, some women prefer a cream, especially if they need only a small amount.
Most vaginal estrogen treatments require application just twice weekly, making them convenient for busy schedules.
When Vaginal Estrogen Isn’t Right for You
While vaginal estrogen is safe for most women, it’s not appropriate for everyone.
Contraindications include:
- Women using aromatase inhibitors for certain types of breast cancer
- Undiagnosed vaginal bleeding
- Pregnancy and breastfeeding
Today’s Takeaways
Vaginal estrogen therapy is safe and highly effective for treating common perimenopausal and menopausal symptoms. The black box warning causes unnecessary fear and prevents many women from receiving this beneficial treatment.
If you experience vaginal dryness, recurrent UTIs, or painful intercourse, consider vaginal estrogen as a treatment option. Ask your Banner Peak Health physician whether this therapy is suitable for you.

Why I Broke Free From the Healthcare Machine
As a child, I dreamed of becoming a physician.
I envisioned building relationships with patients, understanding their unique needs, and providing thoughtful, individualized care. As I pursued the long journey through medical training, I discovered that connecting with my patients provided the greatest meaning and satisfaction.
When I began practicing primary care, I hoped to maintain those connections. Instead, I found myself trapped in a system that prioritized efficiency over relationships.
The Reality of Traditional Medicine
Every patient encounter felt rushed. I tried to take my time with each person, but with 15–20 patients scheduled daily, I had just 20 minutes — often less — for each appointment. After getting patients settled in rooms, the actual conversation lasted mere minutes.
Patients would say, “One more thing,” and I’d have to respond, “We don’t have time for that today. You’ll need to make another appointment.” That response made me feel terrible.
I wasn’t providing the care patients deserved, and I wasn’t satisfied with my work.
The Moment Everything Changed
Over time, the administrators at my practice chipped away at each doctor’s autonomy. Then came a pivotal moment — a new policy about working in urgent care — when I realized I had become just a cog in a machine.
There was no recognition of the importance of continuity between doctor and patient. Everything was reduced to a numbers game, focused on efficiency and shifting patients to urgent care where they saw providers who didn’t know them.
That day, I called a colleague who had left the practice and asked, “What am I doing here?”
Her advice was simple: “Hang up and call Barry Rotman.”
A Luxury We All Deserve
Many people perceive concierge medicine as a luxury, and I agree. It is a luxury — one we all deserve.
Concierge care makes the doctor-patient relationship special again, transforming healthcare from transactional to relational.
Some patients tell me they already have a great relationship with their doctor in a traditional practice. That’s wonderful, but it’s the exception, not the rule. That doctor is likely bending the rules or pushing against the system to provide that level of care. Even then, what patients think is great care could be better in a concierge model.
This belief is so strong that I use concierge care myself. I’ve seen both sides of medicine, and I know which type of care I want for my health.
How Concierge Medicine Benefits Patients
The most obvious benefit is time — not just time spent face-to-face with patients, but time spent behind the scenes.
I can call specialists about my patients, coordinate with radiologists about imaging studies, and dig deep into the minutia of all facets of their health.
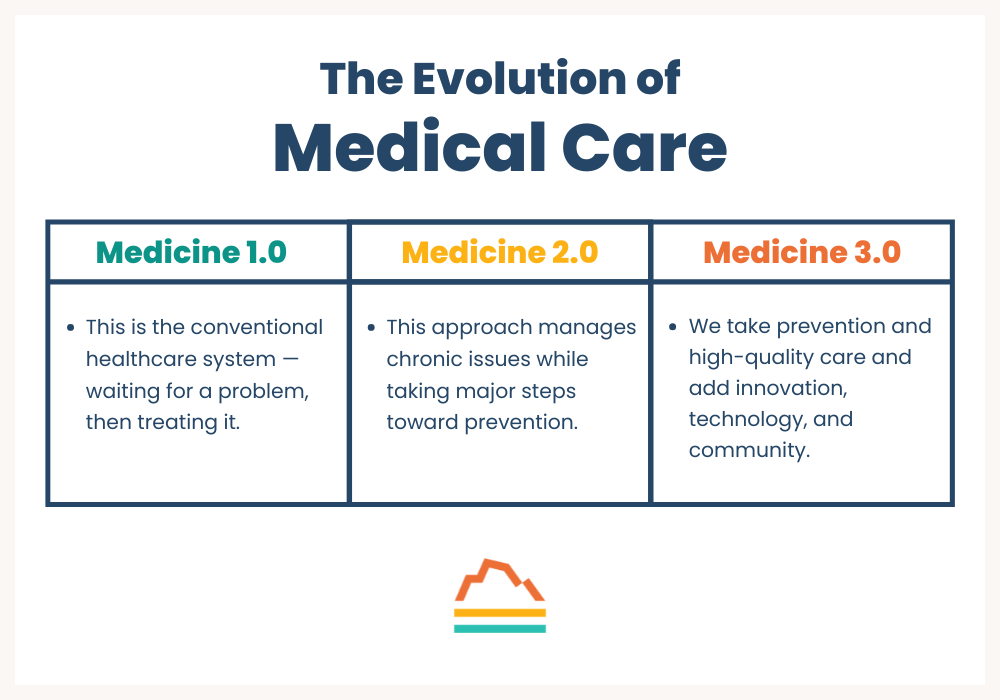
Time also allows me to practice what I call medicine 2.0 and 3.0, with more flexible appointment types. I can schedule quick phone calls, video visits, or Zoom meetings.
This flexibility helps meet people where they are and work on their specific goals.
The Evolution of Medical Care
Medicine 1.0
This is the conventional healthcare system — waiting for a problem, then treating it. It’s reactive medicine that leads to poor health outcomes with little emphasis on prevention.
Medicine 2.0
This approach manages chronic issues while taking major steps toward prevention.
We work to prevent cancer, neurodegenerative disease, and cardiovascular disease — still the number one killer in the United States. We examine family history and personal factors to create individualized prevention plans.
Medicine 3.0
We take prevention and high-quality care and add innovation, technology, and community. We build on a good model to make it great.
Addressing What Matters Most
In traditional care, doctors lack the time to address issues like stress management, even though stress impacts everything from sleep to exercise to heart rate variability.
In the concierge model, we have time for these conversations. We can develop tailored strategies for stress management that fit into each patient’s busy life.
Traditional medicine stays surface-level. There’s no opportunity to uncover that stress might be the root cause of multiple symptoms. In concierge care, we can dig deeper.
What Motivates Me Every Day
The most rewarding aspect of practicing concierge medicine is the bond I form with each patient. This connection gets me up in the morning and keeps me going.
It’s hard to help patients if you don’t know them well. Now I have the privilege of truly knowing my patients and providing care that addresses their unique needs.
Today’s Takeaways
Having a doctor who knows you personally, coordinates your care, serves as your cheerleader, and helps with both small issues and nebulous health challenges isn’t just life-changing — it can be lifesaving.
By joining Banner Peak Health, I’ve met my original goals as a doctor: to be present for my patients and to practice quality medicine joyfully. I now have the time to care for the whole person and honor each patient’s individuality.
I’m thrilled to have begun this new phase of my career.
Pneumococcal Vaccine Schedule for Adults: Which Is Best for You?
The medical community used to believe vaccinating infants and young children was more important than vaccinating adults.
While early vaccination prevents infectious diseases from spreading among large populations, we now know that our ability to fight off certain diseases can decline as we age, especially in those with chronic illnesses and weakened immune systems.
One of those diseases is pneumonia, a lung infection that usually presents with fever and cough, often due to bacteria entering the lower respiratory tract and replicating.
Older and/or sicker people have a higher risk of severe pneumonia-related complications, though younger, healthier folks aren’t immune. The best pneumococcal vaccine schedule for you depends on your age, vaccination history, and underlying risk factors.
The CDC’s Updated Recommendations for Pneumococcal Vaccines for Adults
In June 2024, the CDC approved PCV21, a new pneumococcal vaccine for adults, and updated its guidelines that October.
Former guidelines recommended individuals aged 65 and over start pneumonia vaccination. Now, due to emerging data demonstrating an increase in pneumonia cases among 50+ year-olds, the CDC suggests everyone over 50 be vaccinated against pneumonia.
A Brief History of Pneumonia Vaccination
Many types of pneumonia exist. PCV21 prevents a specific type of bacterial pneumonia caused most commonly by streptococcus pneumonia. It doesn’t prevent atypical pneumonia, also known as walking pneumonia.
The first pneumonia vaccines, introduced in the early 2000s, targeted the serotypes most common among children and certain adults. Eventually, many of those serotypes disappeared because of herd immunity and the vaccination of higher-risk adults.
It’s a cycle: New strains appear, we create and administer vaccines to fight those strains, those strains are eradicated, new strains appear, etc. That’s why we’ve seen frequent updates to the pneumococcal vaccine schedule for adults and a quick succession of new pneumococcal vaccines for adults in the last decade.
The new vaccine (PCV21) contains no eradicated serotypes; only the serotypes that cause 77–85% of invasive pneumococcal infections in adults.
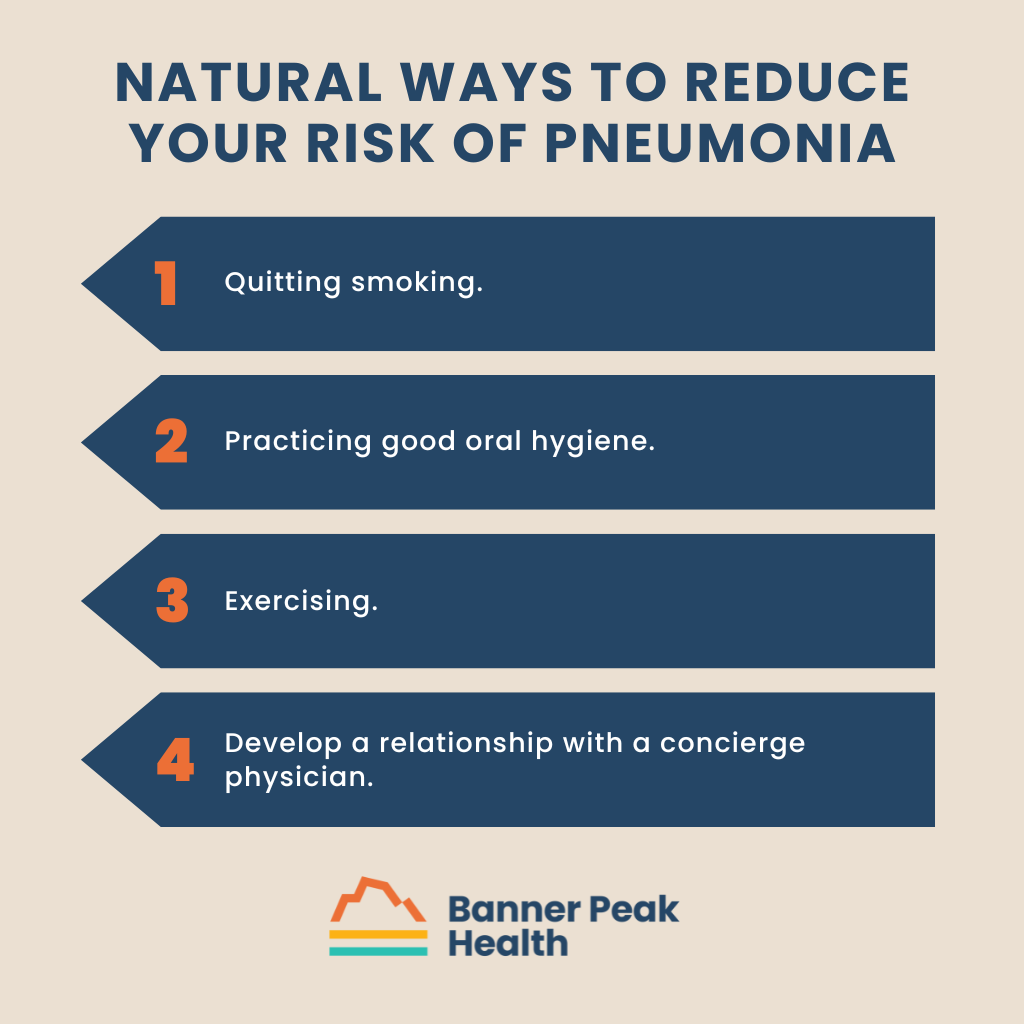
Natural Ways to Reduce Your Risk of Pneumonia
Aside from following a pneumococcal vaccine schedule for adults, you can reduce your risk of pneumonia by:
- Quitting smoking. If you don’t smoke, don’t start. In addition to increasing your risk of pneumonia, smoking damages the lungs, increases the risk of lung diseases like chronic obstructive pulmonary disease (COPD), and exacerbates existing chronic diseases like diabetes and heart disease.
- Practicing good oral hygiene. Regularly brushing your teeth limits the colonization of certain bacteria in your mouth. Left unchecked, these bacteria could spread to your lungs and lower respiratory tract.
- Exercising. Regular physical activity keeps your lungs in good shape. Exercise is especially helpful for patients with chronic conditions, including diabetes, heart disease, and chronic kidney disease.
- Develop a relationship with a concierge physician. It’s not enough to find any board-certified physician. Many physicians are swamped with patient panels thousands strong. They don’t have time to research all the new pneumonia vaccines introduced in the last 15 years, and they often make generic, population-based recommendations that disregard individual risk factors.A physician practicing in a concierge setting enjoys a small patient panel. He or she has time to learn about your medical history and research the best pneumococcal vaccine schedule for you.
Today’s Takeaways
While PSAs about seasonal vaccines (e.g., flu shots and COVID boosters) are common this time of year, it’s important to choose vaccines and boosters based on your individual risk — not just population-based recommendations.
For most patients who have never received pneumococcal vaccines for adults and are now eligible, PCV21 is the best choice. Meanwhile, many patients who have already received a recent pneumococcal vaccine may not need PCV21 now or in the near future.
The best way to stay healthy is to find a physician who has time to get to know your personal history and research the most appropriate vaccines for you. The doctors at Banner Peak Health make every recommendation on a case-by-case basis and are happy to answer your questions. Schedule an appointment today.
When to Start HRT for Perimenopause: A Physician’s Guide
Female patients in their forties often ask me about treatments for menopausal symptoms. When I mention hormone replacement therapy (HRT), some of them get nervous.
Because of outdated and since-debunked research, HRT has developed a stigma. Today, I’m debunking the most common misconceptions about HRT and perimenopause, including when to start HRT for perimenopause (as soon as you experience symptoms) and whether HRT is safe and effective (for many women, it is).
Understanding Perimenopause: A Process, Not an Event
While the average age for menopause in the United States is 51 (defined as going 12 months without a period), the journey to get there — known as perimenopause — can begin up to a decade earlier.
(Interestingly, there’s often a strong correlation between when a woman experiences menopause and when her mother did, suggesting the timing has a genetic component.)
Perimenopause isn’t a single event. It’s a gradual process that lasts several years. During this time, different symptoms may emerge, with sleep disruption often being the first noticeable sign. This is followed by what we call vasomotor symptoms: hot flashes, night sweats, and heart palpitations.
Many women also experience mood changes, including increased irritability and sometimes depressed mood.
Physical changes can include vaginal dryness and more frequent urinary tract infections. Some women also report cognitive changes, often described as “brain fog.”
Benefits of Starting HRT During Perimenopause
HRT has emerged as one of the most effective treatments for perimenopausal symptoms, particularly for managing vasomotor symptoms. Because of outdated research, most women don’t know this.
In 2002, a series of clinical trials called the Women’s Health Initiative (WHI) suggested that HRT use is associated with high risks of stroke and breast cancer. Instead of asking when to start HRT for perimenopause, women asked when to end HRT for perimenopause. Many women discontinued treatment.
However, subsequent research has largely debunked these findings, and we now have a stronger understanding of HRT’s safety profile and benefits.
When started during perimenopause, HRT offers several benefits. It can reduce the risk of depression, even in women who aren’t experiencing mood changes, and may decrease the risk of coronary artery disease when started close to menopause.
HRT has also shown promise in preventing cognitive decline and protecting the bones, reducing the risk of osteoporosis. Additionally, it helps manage genitourinary symptoms (vaginal dryness and more frequent UTIs) that can occur before menopause.
Is HRT Right for You?
Before asking your healthcare provider when to start HRT for perimenopause, consider your personal and family health history.
If you have a history of stroke, breast cancer, endometrial cancer, or ovarian cancer, avoid HRT. The same applies to those with blood clots, clotting disorders, or poorly controlled blood pressure. If blood clots are your only concern, transdermal estrogen might be an option, as it carries a lower clotting risk than oral estrogen.
Some relative contraindications include advanced liver disease and heavy or irregular bleeding during perimenopause. It’s also important to note that HRT isn’t a reliable birth control option, so if you still need contraception, consider other options.
Treatment Options
HRT isn’t one-size-fits-all. The treatment comes in different forms, including oral medications, transdermal patches, topical creams, and combinations through compounding pharmacies.
For women with an intact uterus, HRT typically includes both estrogen and progesterone, while those who’ve had a hysterectomy usually only need estrogen. Women with a progesterone IUD may not need additional progesterone in their HRT.
Testosterone therapy can be particularly helpful for specific perimenopausal symptoms, especially decreased libido and cognitive issues (brain fog, difficulty remembering names, etc.).
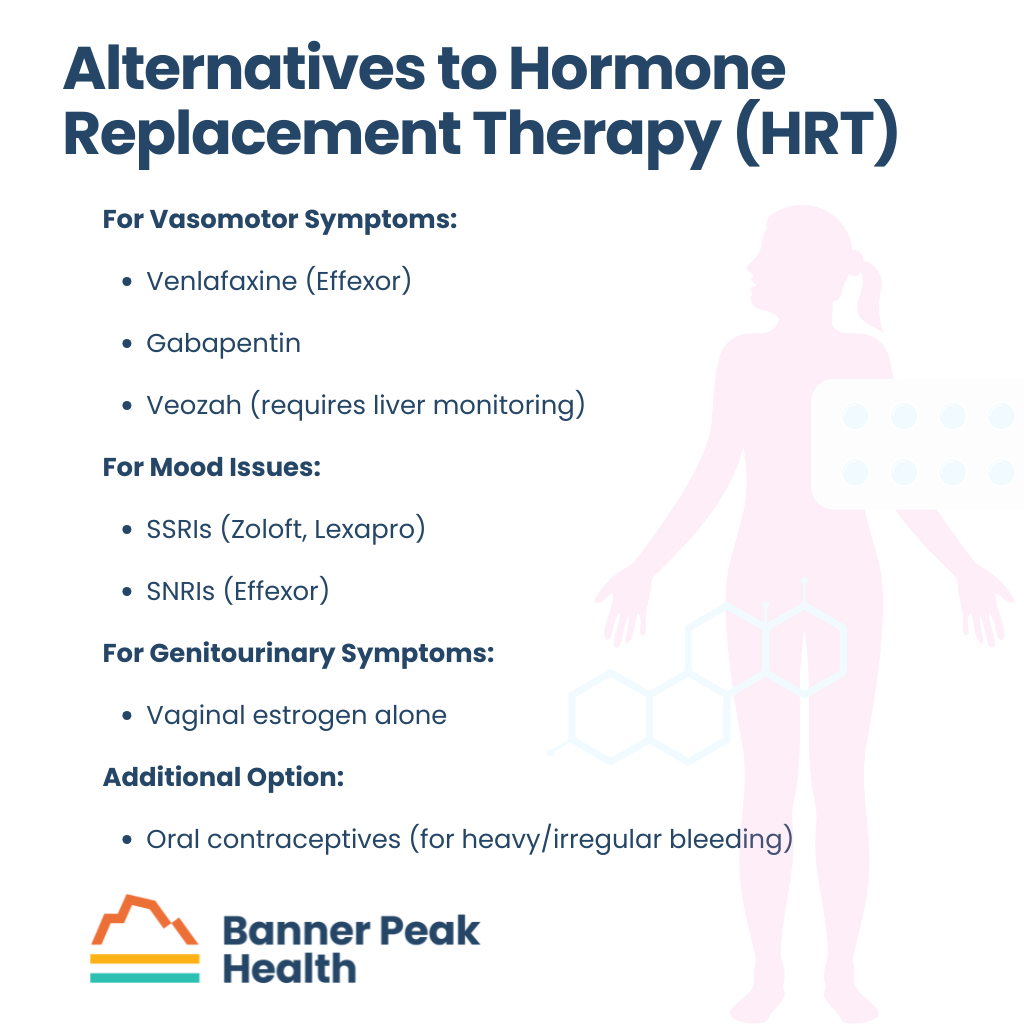 Alternatives to HRT
Alternatives to HRT
For women who can’t or choose not to use HRT, several alternatives exist.
You might manage vasomotor symptoms with medications like venlafaxine (Effexor) or gabapentin. A newer option, Veozah, is available but requires careful liver function monitoring.
You may address mood issues with SSRIs like Zoloft or Lexapro, or SNRIs like Effexor. For genitourinary symptoms, vaginal estrogen alone may be sufficient.
Some doctors might recommend oral contraceptives instead of HRT, particularly for women who experience heavy, irregular bleeding or who need contraception. While these contain higher doses of estrogen than typical HRT, they can manage certain symptoms.
Insurance and Access
Insurance coverage for HRT varies.
Insurance often covers common forms like estrogen sprays, oral progesterone, estrogen patches, and vaginal estrogen formulations, though out-of-pocket costs can still be significant. Coverage for compounded formulations is less common, but may be possible with proper documentation of medical necessity.
When to Start HRT for Perimenopause
Decide when to start HRT for perimenopause based on your symptoms and medical history.
Don’t wait until symptoms become severe or hurt your quality of life. If you think you might be experiencing perimenopausal symptoms, schedule a conversation with your healthcare provider to discuss whether HRT might be right for you.
Here at Banner Peak Health in Walnut Creek, I customize HRT treatment to each woman’s needs and preferences, whether that means choosing pills, patches, or creams. What works best for one woman may not be ideal for another, and finding the right combination often involves some trial and error.
If you’d like to explore your HRT treatment options or discuss when to start HRT for perimenopause, reach out today to schedule an appointment at our Walnut Creek office. I’m happy to chat.