We all want normal blood pressure. But what is the normal blood pressure for you? It’s a more complicated question than it seems.
Blood pressure is crucial to overall health, but how do we learn what our normal is, and how do we monitor it once we do?
What Is the “Normal” Blood Pressure?
The chart below reflects the American Heart Association’s parameters for “normal blood pressure.” However, those parameters are more complicated than they appear.
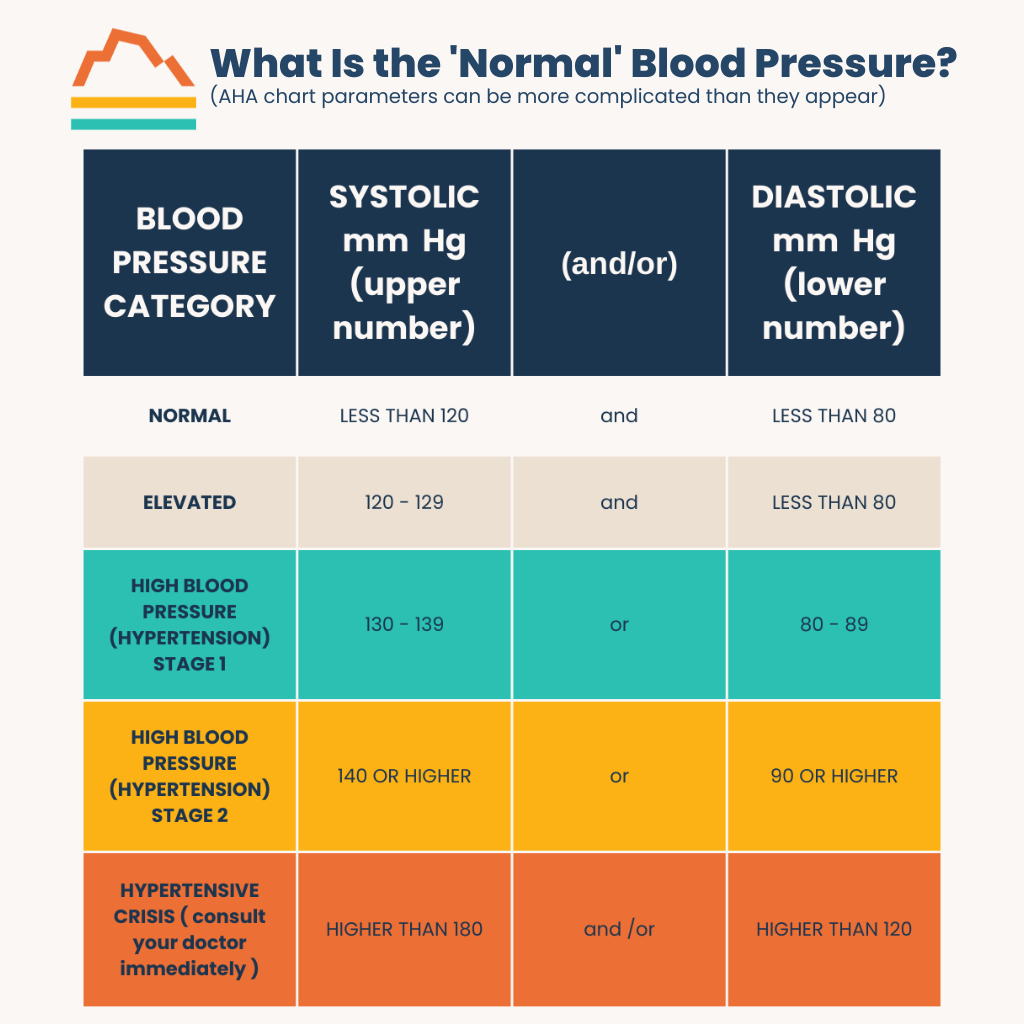
The numbers corresponding to “normal” in the chart are the blood pressure goals for healthy adults, not the results for the average American adult. The average blood pressure isn’t desirable from a health perspective because nearly half of American adults are hypertensive.
The “normal blood pressure” target has also changed significantly in the nearly four decades I’ve been in medicine. “Normal” blood pressure was defined as under 160 systolic in the 1980s, according to the SHEP study. The American Heart Association and the American College of Cardiology updated those guidelines to 140 systolic in 2014.
How Your Blood Pressure Measurement Changes
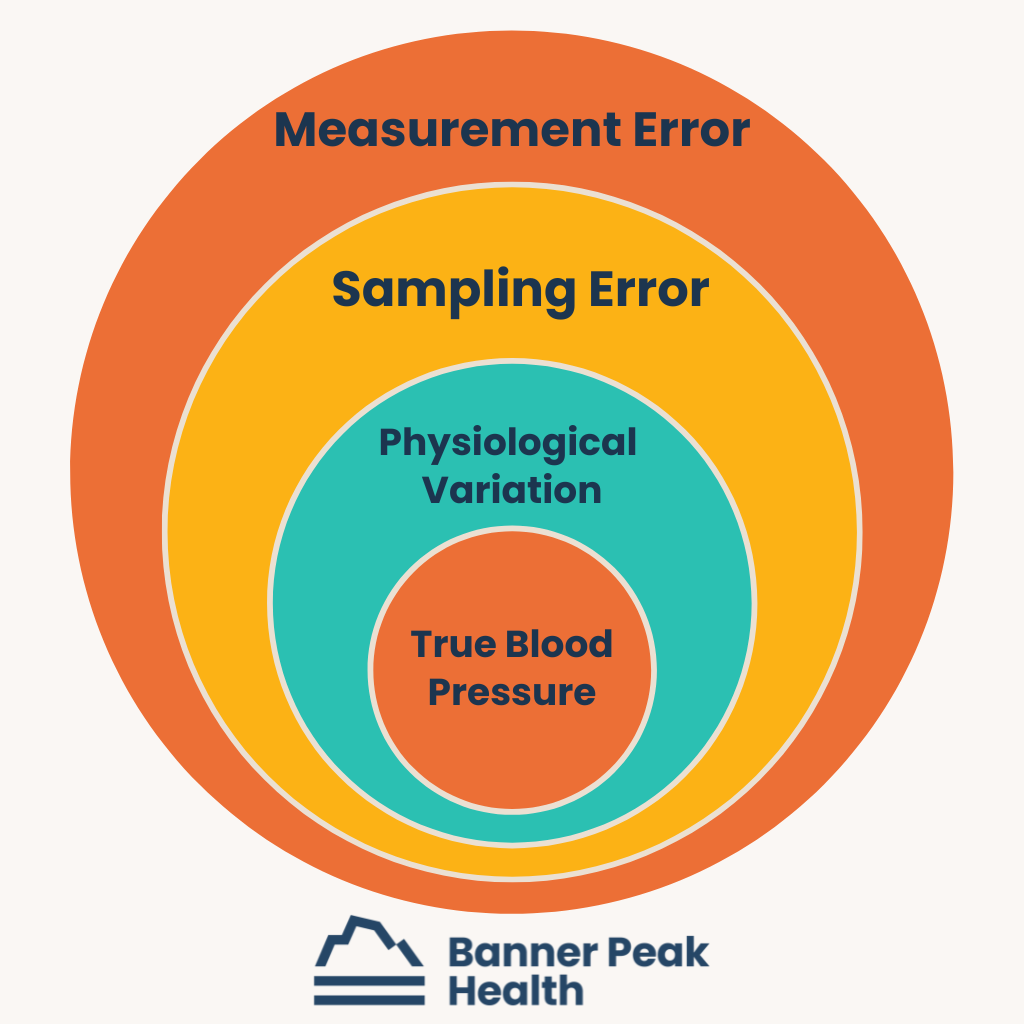
Medical guidelines recommend that adult blood pressure be lower than 120 or over 70, based on the SPRINT study. But even this recommendation isn’t straightforward. Many factors influence your measured blood pressure from minute to minute, and they compound like Russian nesting dolls.
For example, the study that determined the latest “normal blood pressure” did so by averaging the blood pressures of healthy adults taken every five minutes as the participants were calm and at rest without a doctor’s presence. Compare those conditions with the conditions under which you typically have your blood pressure taken — immediately after sitting down in an anxiety-inducing doctor’s office — and you can see why your blood pressure may not measure up to the standard.
Physiological Variations
Blood pressure changes constantly, like the weather, because of physiological variations, including body position, exercise, stress level, etc. Measuring it accurately requires a standard of conditions seldom met in daily life.
Sampling Errors
Blood pressure measurements also vary because of sampling errors. For instance, taking your blood pressure immediately after rushing into your doctor’s office after facing frustrating traffic is a bad idea. The measurement will probably be high and inaccurate.
Equipment and Technique Errors
Finally, errors stem from misused equipment and misapplied technique.
Common mistakes include using wrist cuffs. These measure blood pressure at the radial artery, which differs significantly from the brachial artery (the artery in your upper arm). Comparing the numbers from a wrist cuff to those in a chart meant for an arm cuff yields inaccurate results.
Another common mistake is positioning the arm lower than the heart. This position creates additional pressure in the artery and throws the measurement off. Having the wrong-sized cuff also leads to inaccurate measurements.
Getting an Accurate Blood Pressure Reading
How can you get an accurate blood pressure measurement? Be an educated consumer.
The SPRINT study taught us that the most accurate blood pressure measurement is taken at home, not at the doctor’s office. We need to be calm and comfortable.
That said, the simple task of determining blood pressure is not a simple task.
Understanding your blood pressure as an average or trend rather than a single measurement or number is important. Be familiar with your body and have conversations with your doctor about what is the normal blood pressure for you. Staying informed and engaged is the best way to stay healthy.

Barry Rotman, MD
For over 30 years in medicine, Dr. Rotman has dedicated himself to excellence. With patients’ health as his top priority, he opened his own concierge medical practice in 2007 to practice medicine in a way that lets him truly serve their best interests.



