Many women avoid vaginal estrogen therapy because of concerns about hormone treatments. These concerns stem from frightening media coverage and FDA black box warnings.
However, vaginal estrogen remains our most effective treatment for common and disruptive menopausal symptoms.
Understanding Vaginal Estrogen
Despite common misconceptions, vaginal estrogen is absorbed minimally — almost entirely within vaginal tissues, with little to none entering your bloodstream.
Vaginal estrogen acts locally rather than systemically. Unlike estrogen patches or pills that affect your entire body, vaginal estrogen works only where applied.
This local action means vaginal estrogen has few to no contraindications. It’s even safe for many women with a history of breast cancer.
Why Consider Vaginal Estrogen Therapy?
Vaginal estrogen treats several common symptoms that fall under Genitourinary Syndrome of Menopause (GSM):
- Vaginal dryness
- Recurrent urinary tract infections
- Pain during intercourse (dyspareunia)
For these conditions, vaginal estrogen is the most effective treatment available. Relief is typically excellent, with many women reporting improvement in their symptoms.
When treating recurrent UTIs, vaginal estrogen provides additional benefits. It helps avoid repeated antibiotic use, reducing risks of antibiotic resistance and side effects from those medications.
Demystifying the Black Box Warning for Vaginal Estrogen
The FDA places a black box warning on all estrogen products. This warning states that unopposed estrogen (without progesterone) increases the risk of:
- Endometrial cancer in women with a uterus
- Stroke and blood clots
- Dementia in women over 65
- Pulmonary embolism and heart attack
- Breast cancer when combined with progestin
Modern research has debunked most concerns in this warning, even for systemic estrogen therapy. The book “Estrogen Matters” provides an excellent review of this evidence.
More importantly, this warning doesn’t apply to vaginal estrogen. Since vaginal estrogen isn’t absorbed systemically, it doesn’t create the risks associated with whole-body exposure.
A movement exists to remove this warning from vaginal estrogen products. Dr. Rachel Rubin, recently featured on Dr. Peter Attia’s podcast, leads physician groups like “Unboxing Menopause” and “Let’s Talk Menopause” that meet with the FDA to advocate for this change. These groups argue that the warning prevents women from accessing effective treatment for their symptoms by scaring them with information that doesn’t apply.
In July 2025, these advocacy efforts gained significant momentum when FDA Commissioner Dr. Marty Makary convened a panel of experts who overwhelmingly urged the agency to remove the black box warnings from vaginal estrogen products.
While no formal action has been taken yet, Makary promised the FDA would “take a hard look at” removing the warning and indicated they’re trying to move faster than typical government processes.
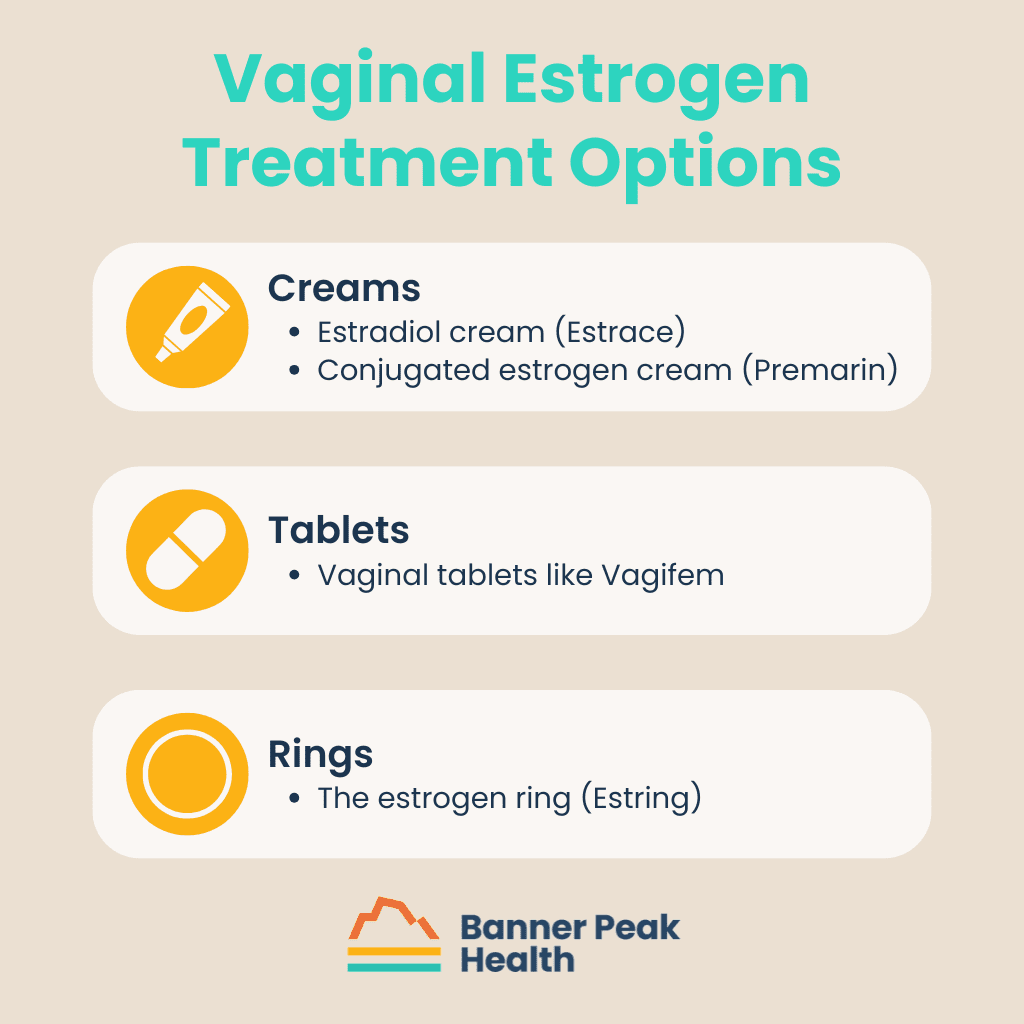
Vaginal Estrogen Treatment Options
If you decide vaginal estrogen is right for you, several options exist.
Creams
Two main types of vaginal estrogen cream are available:
Tablets
Vaginal tablets like Vagifem are a less messy alternative to creams.
Rings
The estrogen ring (Estring) is an alternative option.
I typically recommend vaginal tablets for most patients because they’re less messy and easier to use. However, some women prefer a cream, especially if they need only a small amount.
Most vaginal estrogen treatments require application just twice weekly, making them convenient for busy schedules.
When Vaginal Estrogen Isn’t Right for You
While vaginal estrogen is safe for most women, it’s not appropriate for everyone.
Contraindications include:
- Women using aromatase inhibitors for certain types of breast cancer
- Undiagnosed vaginal bleeding
- Pregnancy and breastfeeding
Today’s Takeaways
Vaginal estrogen therapy is safe and highly effective for treating common perimenopausal and menopausal symptoms. The black box warning causes unnecessary fear and prevents many women from receiving this beneficial treatment.
If you experience vaginal dryness, recurrent UTIs, or painful intercourse, consider vaginal estrogen as a treatment option. Ask your Banner Peak Health physician whether this therapy is suitable for you.


Lindsay Klein, MD
After years of feeling constrained by traditional medicine's time pressures and administrative demands, Dr. Klein joined Banner Peak Health to return to her original calling: building meaningful relationships with patients and providing truly individualized care.