I’m a huge fan of physician Peter Attia, author of the book Outlive. He’s used his popularity to reshape the vocabulary of preventative medicine.
Attia defines “healthspan” as the number of years we can live with a high level of function, as opposed to “lifespan,” which is the number of years we’re alive regardless of health status.
He’s also coined the terms “Medicine 2.0” and “Medicine 3.0.” The former, a reactive, disease-based approach, treats existing illnesses. The latter prevents illness from developing by using a far-sighted approach.
Attia has become one of the best-known proponents of the “Longevity Medicine” movement, focusing on how to help people lead longer and more fulfilling lives. Prevention has always been a core aspect of primary care medicine, but Peter Attia has refocused its goals and created a growing demand for a more sophisticated level of prevention than has been available in traditional medicine.
Inspired by Peter Attia, I want to bring state-of-the-art preventative healthcare to Banner Peak Health, practice Medicine 3.0, and maximize patients’ healthspan.
Introducing the Metric-Driven Empowerment Cycle
I studied political economy as an undergraduate, focusing on how political and economic forces shape our society. I’ve retained this vantage point throughout my medical career.
In my last blog post, I described the term “diagnostic desert,” analogous to the term “food desert,” which is the scarcity of grocery stores in lower socio-economic neighborhoods. With no lucrative drug, surgery, or diagnostic procedure, vast areas of our healthcare system are underserved.
Most preventative healthcare falls into this category. Tragically, our current system incentivizes doctors to prescribe patients medication rather than work with those patients to help them live healthier lives.
Pharmacology plays a vital role in prevention, particularly in reducing the risk of hypertension and elevated cholesterol. However, our most potent tools for overall risk reduction stem from how we eat, sleep, exercise, and handle stress.
Practicing medicine at this level appears old-fashioned and low-tech. However, recent technological advances have enabled convenient, real-time, continuous monitoring of biomarkers in these areas. A small ring can measure the physiology of your sleep. A patch on your arm can record how your blood sugar varies throughout the day. By recording actionable data, these technologies provide the tools to fine tune and enhance the wearer’s health.
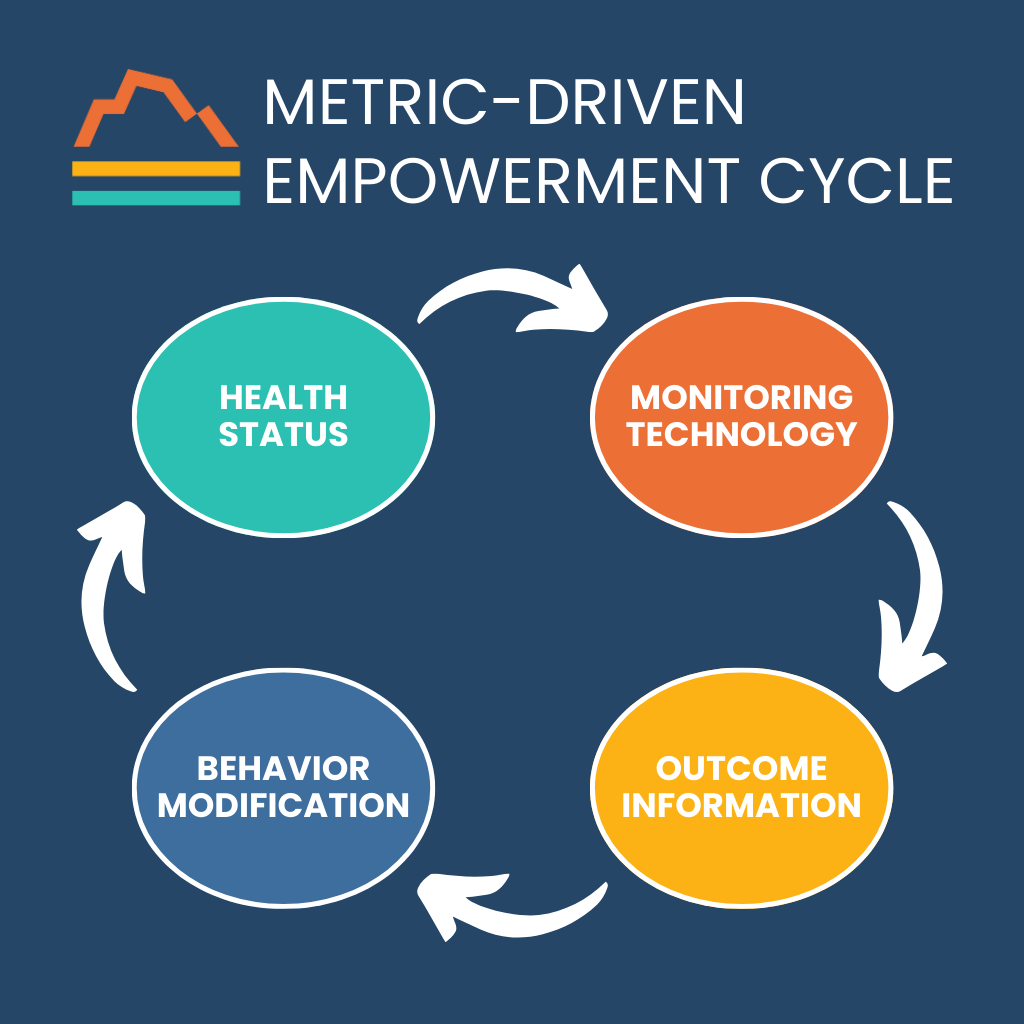
Harnessing these technological tools, we can follow a reiterative process to increase healthspan:
- Identify the health status to be improved
- Optimally measure the health status
- Use the diagnostic information to modify behavior
- Watch the new behavior improve health status
- Rinse and repeat
This cycle represents the foundation of preventative care at Banner Peak Health. We call it the Metric-Driven Empowerment Cycle (MDEC).
For example, we have a general sense of the quantity of sleep we get. When was bedtime? When did the alarm go off? Any awakenings during the night? However, our quality of sleep is unknown. By definition, we are unconscious when we sleep. Sleep is made up of restorative phases, such as REM and deep sleep, which conditions such as obstructive sleep apnea can disrupt.
Now, consumer wearables and medical devices allow the ongoing assessment of sleep quantity and quality. This technology allows us to diagnose potential problems and monitor and adjust treatment strategies.
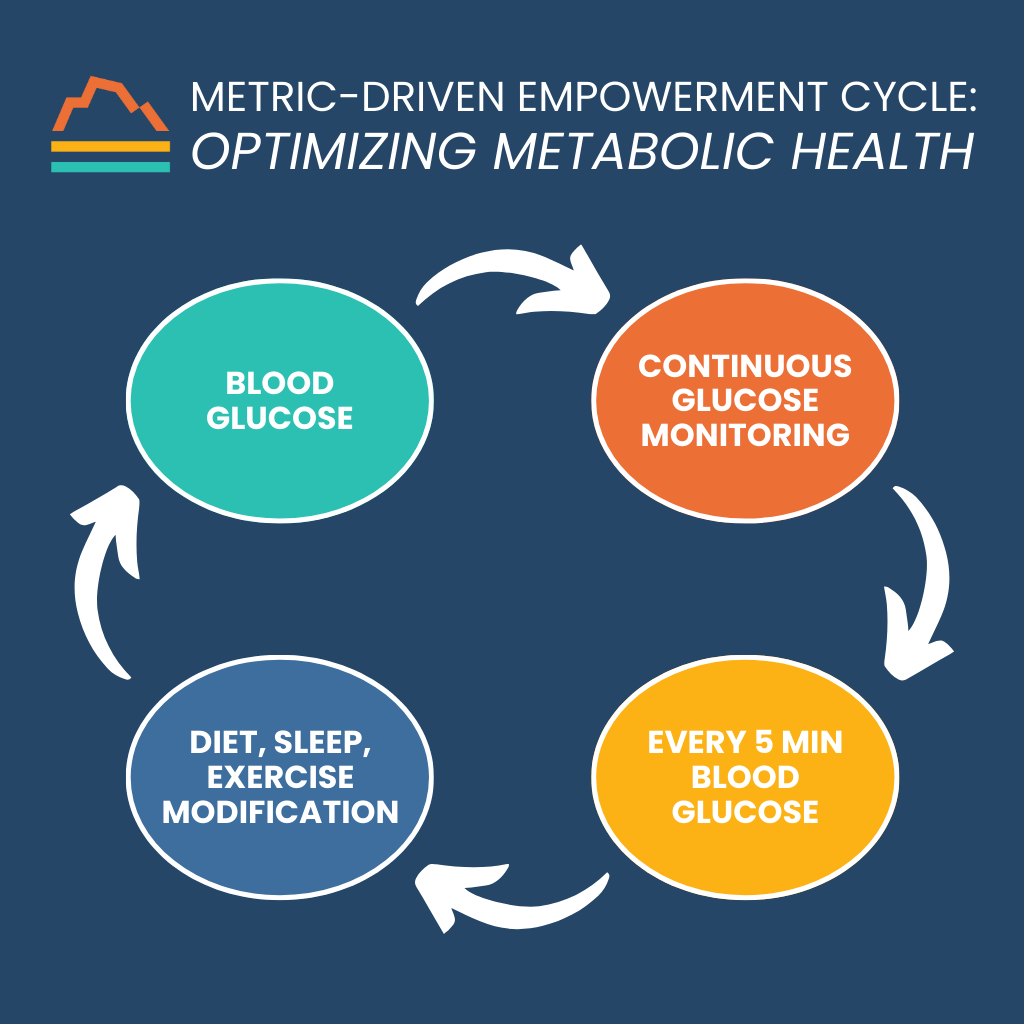
Optimizing metabolic health offers another important area for monitoring technology. We know that elevated glucose (sugar) levels are associated with diabetes mellitus, which is a risk factor for many bad outcomes, including heart disease and strokes. However, pre-diabetes, a condition of insulin resistance but not full-fledged diabetes, can confer a significant risk of these bad outcomes as well. An estimated one in three adults in the United States is pre-diabetic.
New wearable technology can diagnose and manage this extremely common, “hidden” risk factor. A continuous glucose monitor remains on the skin for 10–14 days, noting glucose levels every five minutes. The monitor sends that data to a smartphone, which allows highly personalized diagnosis and treatment.
It’s yet another example of the MDEC:
Final Thoughts
The Metric-Driven Empowerment Cycle provides a new paradigm of care at Banner Peak Health. Now, we can offer the highest quality of care for our patients: medical care that prioritizes prevention and empowers patients by blending the latest medical technology with an old-fashioned determination to work hard.
We want patients to live longer and better!

Barry Rotman, MD
For over 30 years in medicine, Dr. Rotman has dedicated himself to excellence. With patients’ health as his top priority, he opened his own concierge medical practice in 2007 to practice medicine in a way that lets him truly serve their best interests.



