I recently had COVID-19 for the second time. Fortunately, it was mild with minimal cold symptoms: only a stuffy nose and dry cough.
However, I was really tired and “not myself.” Others describe similar sensations and describe it as “COVID brain” or “brain fog.”
Unfortunately, COVID can involve the brain, but I don’t think that was why I felt so fatigued.
Most nights, I wear a SleepImage ring and track my sleep. I suffer from mild obstructive sleep apnea that I treat with nasal dilators and nasal glucocorticoid spray.
Usually, I keep my apnea-hypopnea index (AHI) in the mild range. With COVID, I noticed my AHI rose sharply by 33%.
What happened? I experienced the deleterious effects of nasal obstruction on sleep quality.
Our sleep and overall health depend on how freely we breathe through our noses during sleep. Restorative sleep relies on nasal breathing, which offers numerous advantages over mouth breathing, including improved sleep.
That said, is it dangerous to sleep with a blocked nose?
Health Benefits of Nasal Breathing
Your nose acts as an air filter, catching dust and allergens before they go deeper into your body. It also helps condition and humidify the air before it reaches your lungs.
Breathing through your nose also oxygenates your blood more effectively. The air passing through your nasal passages produces nitric oxide, a vasodilator that improves oxygen circulation.
Another positive response is that the parasympathetic nervous system responds to nasal breathing by lowering blood pressure and heart rate.
Unfortunately, your body misses these benefits when your nose is blocked.
Challenges Associated With a Blocked Nose
Upper respiratory infections can cause nasal congestion, such as colds, COVID, and chronic conditions like allergic rhinitis (hay fever).
Breathing through your mouth long-term can lead to serious complications. For example, your saliva contains antibodies. If your mouth dries out as you breathe, you’re at risk for dental caries and infections.
Bacterial sinus infections and anatomical blockages, like a deviated septum and nasal polyps, can also cause nasal blockages.
Whatever the cause, these blockages cause common symptoms, including:
- Snoring
- Hypopnea
- Apnea
When these symptoms happen simultaneously and your upper airway collapses, it results in obstructive sleep-disordered breathing.
Poor Sleep Quality
When we’re sick, we often feel fatigued. Our first instinct is to attribute the tiredness to the illness’s direct effects.
However, much of that fatigue may be from sleep disruption. The inability to breathe through our noses and rest effectively causes disrupted sleep.
How to Reduce Fatigue and Sleep Better With a Blocked Nose
If you take a sick day, use the opportunity to nap. Napping has many benefits, especially when you’re not well. Increasing your sleep helps boost your immune system so you can recover faster.
Another way to reduce fatigue is to open nasal passages.
Using the diagram below, let’s consider the anatomy susceptible to swelling and blockage.
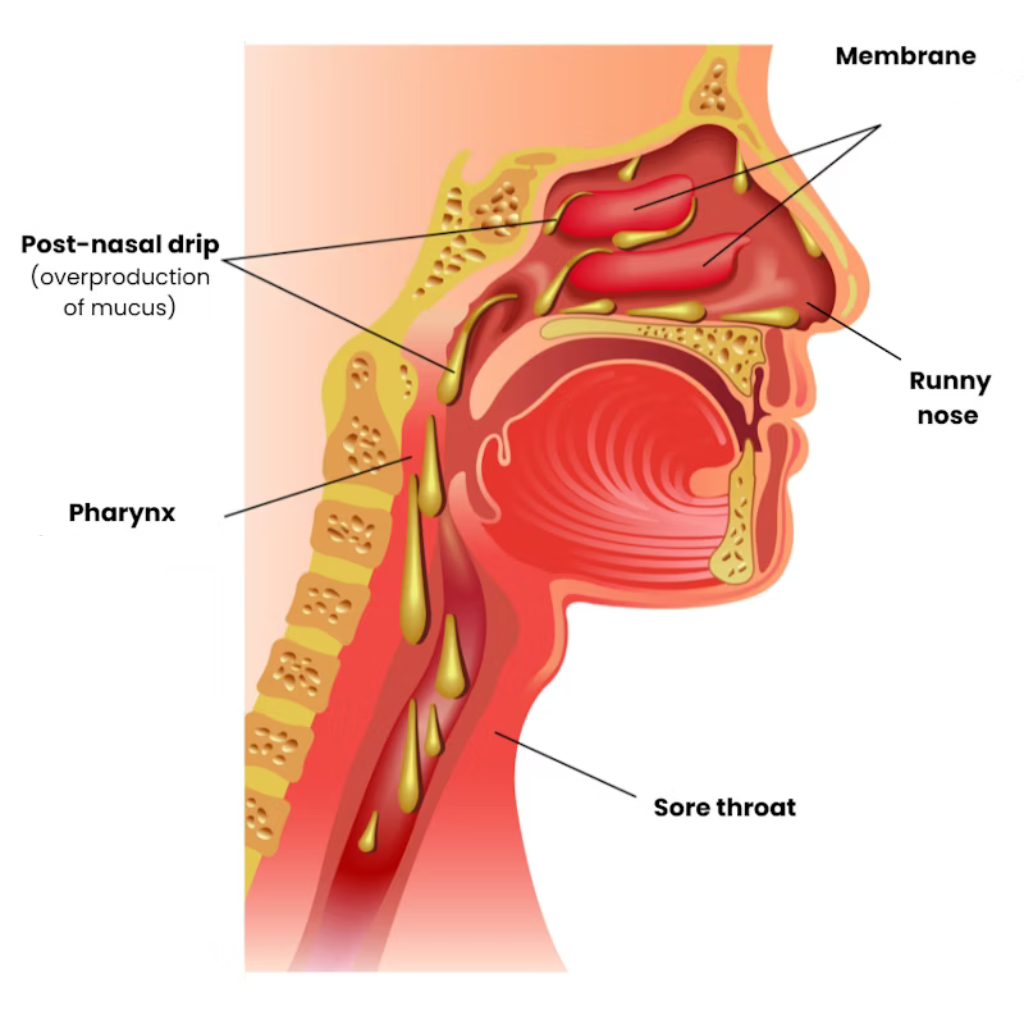
The area labeled “runny nose” is the nares (i.e., nostrils). Beyond is a labyrinth of tissue called turbinates (the two pink folds between “runny nose” and “post-nasal drip”), which swell and secrete mucus when infected or inflamed, causing obstruction and nasal congestion.
Solutions for a Blocked Nose
Here are some common medication and non-medication solutions for a congested nose.
Decongestant Sprays and Pills
Decongestants (e.g., Afrin, Sudafed PE, etc.) help constrict blood vessels in the mucosa, reducing its thickness and opening up blocked nasal passages.
However, these also have a stimulant effect. To reduce fatigue caused by sleep deprivation, use this class of medications cautiously. For some people, they cause insomnia.
Nasal Steroids
Use nasal steroids (e.g., Flonase Sensimist and Nasacort) for viral upper respiratory infections, COVID-19, and allergic rhinitis. They’re available over-the-counter without a prescription.
Nasal steroids are glucocorticoids, which, when absorbed into your body in higher doses, can have significant side effects. However, the spray is a fine mist that the body doesn’t absorb appreciably; it remains almost entirely in the nose.
There, it shrinks the mucosa and reduces nasal secretions. The best time to use a nasal steroid is immediately after a shower when the steam has opened your nasal passages.
Nasal Strips
Nasal strips (e.g., Breathe Right) physically dilate the frontal nasal passages. However, nasal obstruction occurs deeper in the turbinates, which are beyond the reach of nasal strips.
So, while the nasal strips may offer some relief, it’ll be minimal.
Non-Medicated Sprays
Non-medicated sprays (e.g., nasal saline and Neti Pots) are effective for allergic rhinitis because they flush the total amount of antigen that adheres to the nose’s lining.
Reducing the amount of antigens reduces the signal to your body, which inflames the nasal passages and creates mucus. Improving air filtration in your home reduces the number of airborne allergens that reach your nose.
These solutions don’t help with viral infections (e.g., colds and COVID) because the viruses infect the cells that line your nasal passage and can’t be rinsed away.
Today’s Takeaways
So, is it dangerous to sleep with a blocked nose? Well, it’s best to avoid it if possible. We all get upper respiratory infections occasionally, and despite our best efforts, we suffer from temporary nasal obstruction and become mouth breathers.
However, sleeping with an obstructed nasal passage long-term can lead to significant health and quality of life issues.
If you suffer from nasal obstruction often, address the underlying causes to improve symptoms like fatigue. If you need help diagnosing and treating breathing issues, contact Banner Peak Health.

Barry Rotman, MD
For over 30 years in medicine, Dr. Rotman has dedicated himself to excellence. With patients’ health as his top priority, he opened his own concierge medical practice in 2007 to practice medicine in a way that lets him truly serve their best interests.