For over three years, we’ve waited for the COVID pandemic to be over. An analogy to intensive care medicine seems appropriate.
I was taught that “a patient enters an intensive care unit with dramatic catastrophes and leaves with incremental, slow, methodical improvements.” That is, the beginning is more obvious than the end.
We’ve made tremendous strides in reducing the number of infections, hospitalizations, and deaths attributed to COVID. With these gains, our societal focus has shifted elsewhere. Emergent government policies to address the economic and health effects of the pandemic are being scaled back. But is the pandemic over?
On one hand, the data in Contra Costa County and at the national level demonstrate markedly reduced levels of COVID viral particles in the sewer systems, fewer people in the hospital due to COVID, and fewer people dying.
On the other hand, based on the national data from April, we’re still losing 1,300 people per week to COVID. This yields an annual death rate of 68,000 more people than the number lost to influenza in any year for the last decade. Unfortunately, the risk of COVID is still with us.
Fight On
Vaccination has been our best weapon against COVID. After three years, most of us have had multiple vaccinations and, often, a COVID infection or two. We’re beating back the pandemic because of the level of immunity generated by this process. The obvious question becomes: What is the incremental benefit of yet another vaccination?
The answer depends on your level of risk for a bad outcome from COVID.
Almost everyone currently hospitalized with COVID falls into four broad and potentially overlapping categories:
- Over 50
- Multiple comorbidities (such as obesity, diabetes, heart disease)
- Immunocompromised
- Unvaccinated or under-vaccinated
In fact, 90% of those currently hospitalized have not received the most current bivalent COVID vaccine. This version contains two strains, one against the original Wuhan variant and another against a new omicron variant. Since this vaccine’s release in fall 2022, numerous studies have demonstrated its greater efficacy than the original single-variant vaccine, which will be phased out.
Most of you have already received a bivalent COVID vaccine booster. If you haven’t, please consider getting your first dose of the bivalent COVID vaccine now.
Who Needs a Booster?
What if you’ve already received the bivalent COVID vaccine? On April 19, 2023, the CDC updated its recommendations for booster vaccinations this spring. They identified risk groups who should receive an additional bivalent COVID vaccine, and they’ve included timing recommendations:
- If you’re over 65 years old, you should wait four months from your last vaccination or COVID infection to receive this booster.
- If you’re immunocompromised, you should wait at least two months from your last vaccination or COVID infection to receive this booster.
I sense a growing frustration with being asked to get a COVID vaccination again and again. We remember getting childhood vaccinations that lasted decades, and we can tolerate getting a tetanus booster every 10 years or so. However, the biology of the COVID virus and the vast numbers of infected individuals have allowed rapid evolution to occur, which continues to select for variants that can partially evade our vaccines.
We’ve been able to develop vaccines that work against these newer variants, such as the current bivalent COVID vaccine. Researchers are working to develop vaccines that target parts of the virus that don’t mutate as rapidly as the spike protein, the target of current vaccines.
Also, to compensate for the decline in efficacy over time, we increase the frequency of vaccination to get a recurring boost in our antibody levels, which are at their peak for one to six months after vaccination. Thus, recommendation for frequent vaccination allows us to extract maximum performance from our current vaccination technology, which is needed to maximally protect those at the highest risk.
Who Doesn’t Need a Booster?
It also makes sense to discuss who does NOT currently need a booster vaccination.
The incremental benefit of each additional vaccination has become ever smaller. Thus, for populations whose overall risk of a bad outcome is already very low, such as children and younger adults, a further tiny reduction isn’t worth the discomfort and rare (but not zero) risk of a serious vaccine complication.
Today’s Takeaway
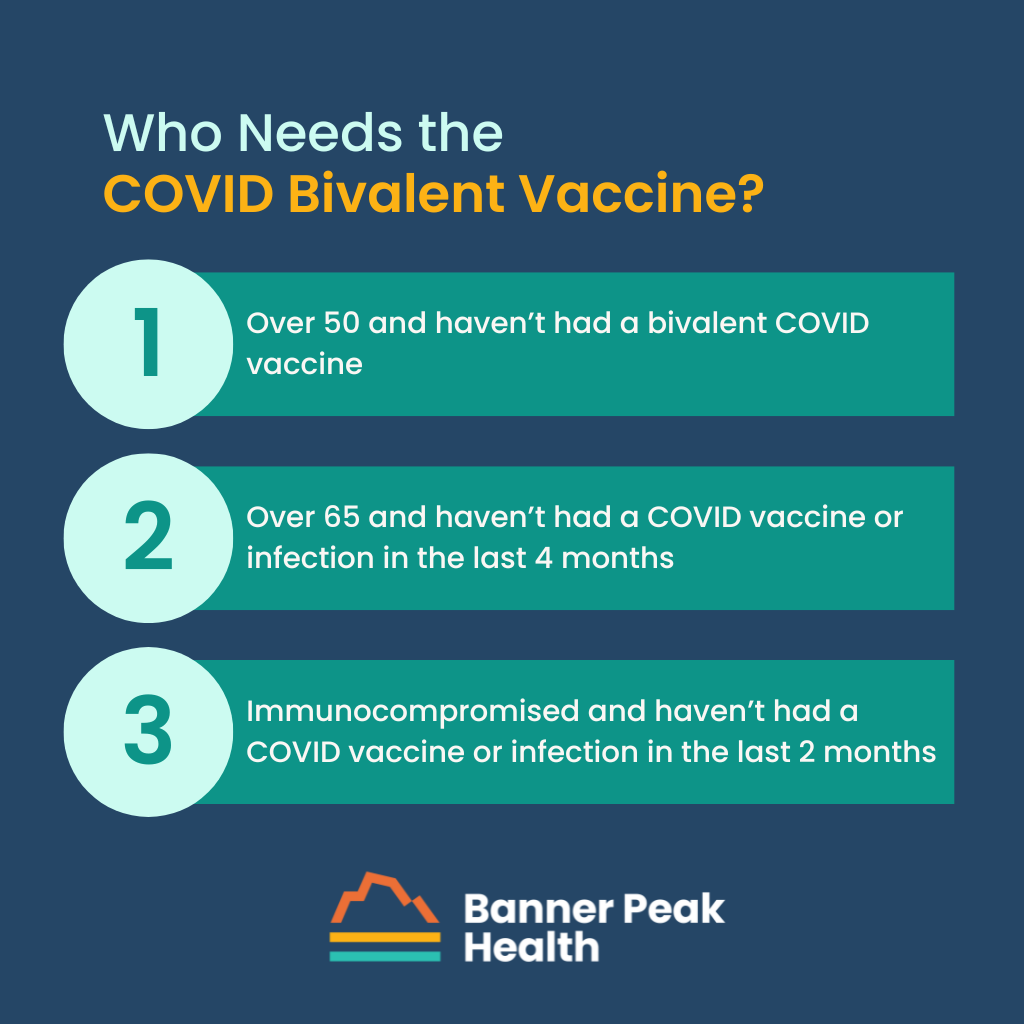
Please get a COVID bivalent vaccine now if you fall into any of these categories:
- If you’re over 50 and haven’t yet had a bivalent COVID vaccine
- If you’re over 65 and haven’t had a COVID vaccine or infection in the last 4 months (or wait until 4 months have elapsed)
- If you’re immunocompromised and haven’t had a COVID vaccine or infection in the last 2 months (or wait until 2 months have elapsed)
Please reach out if you have any questions or concerns.

Barry Rotman, MD
For over 30 years in medicine, Dr. Rotman has dedicated himself to excellence. With patients’ health as his top priority, he opened his own concierge medical practice in 2007 to practice medicine in a way that lets him truly serve their best interests.