Would it surprise you to learn that many chronic illnesses — especially ones without a direct physical cause — are linked to childhood trauma?
Childhood trauma causes the nervous system to develop differently. While we’re still learning about this process, it’s clear there are legitimate, debilitating physical effects of childhood trauma in adulthood.
Defining Childhood Trauma
We define childhood trauma using the same criteria the CDC-Kaiser ACE Study put forth. ACE is an acronym for adverse childhood experiences. These equate to traumatic experiences and include three categories: abuse, household dysfunction, and neglect.
- Abuse can be emotional, physical, or sexual.
- Household dysfunction includes substance use disorders, mental illness in the home, parental separation or divorce, and incarceration of a household member.
- Neglect be emotional or physical.
Aside from bearing the effects of childhood trauma in adulthood, adults can experience new trauma, too. For example, the COVID pandemic was a source of trauma for many adults worldwide.
The Mind-Body Connection and How We Process Pain
The brain’s complex design dedicates parts of itself to rational thought and other parts to primitive survival instincts. We sometimes refer to these parts as our “thinking brain” and “feeling brain,” respectively.
Our feeling brain is where our brain perceives threats in our environment and makes instinctual decisions that keep us alive. This is the fight-or-flight center of the brain.
When we talk about repressed memories, this is the part of the brain we’re referring to. Because those memories connect to experiences too overwhelming for the thinking brain, we store them in the feeling brain.
Triggers are a way to access them.
For example, say you had a terrible experience sometime in the past, and during that experience, a certain type of food was cooking.
Later, you smell that food and suddenly feel terrible but don’t know why. That’s your feeling brain accessing your repressed memory as a result of that trigger — the same smell.
The olfaction is an association your brain formed during the trauma. That association is a trigger that unlocks the memory, but you’re not conscious of it because it exists in your feeling brain rather than your thinking brain.
It’s a form of classical conditioning similar to Pavlov’s dog.
This phenomenon can happen with physical pain, too. Sometimes, if a child suffers an injury as a result of abuse, they may not experience all the associated physical pain because it would just be too overwhelming.
Their brain locks it away to keep the child safe and alive, but that pain gets triggered later in life because the nervous system remembers it from before. This is one of the many effects of childhood trauma in adulthood.
Effects of Childhood Trauma in Adulthood
When the brain and body know it’s safe, they try to process the physical and emotional pain inflicted years before, but the rational mind doesn’t understand where the pain suddenly comes from. This is why adult victims of childhood trauma often tell their doctor, “I have all these things wrong with me, and I don’t know why.”
Physical effects of childhood trauma in adulthood often include GI symptoms like irritable bowel syndrome (IBS). They can also include overactive bladder, fibromyalgia, and inflammation and muscle pain (muscle knots).
When you better understand the effects of childhood trauma in adulthood, you can begin to process them and begin your journey to recovery.
If you have a history of childhood trauma (as defined above by the CDC-Kaiser study) and experience the symptoms we’ve described, now might be the right time to deal with it.
Those things that were once protective no longer serve you. They kept you alive in environments that weren’t nurturing, but now that you’re safe, they’ve come to the surface for a reason. It’s a sign to address them appropriately.
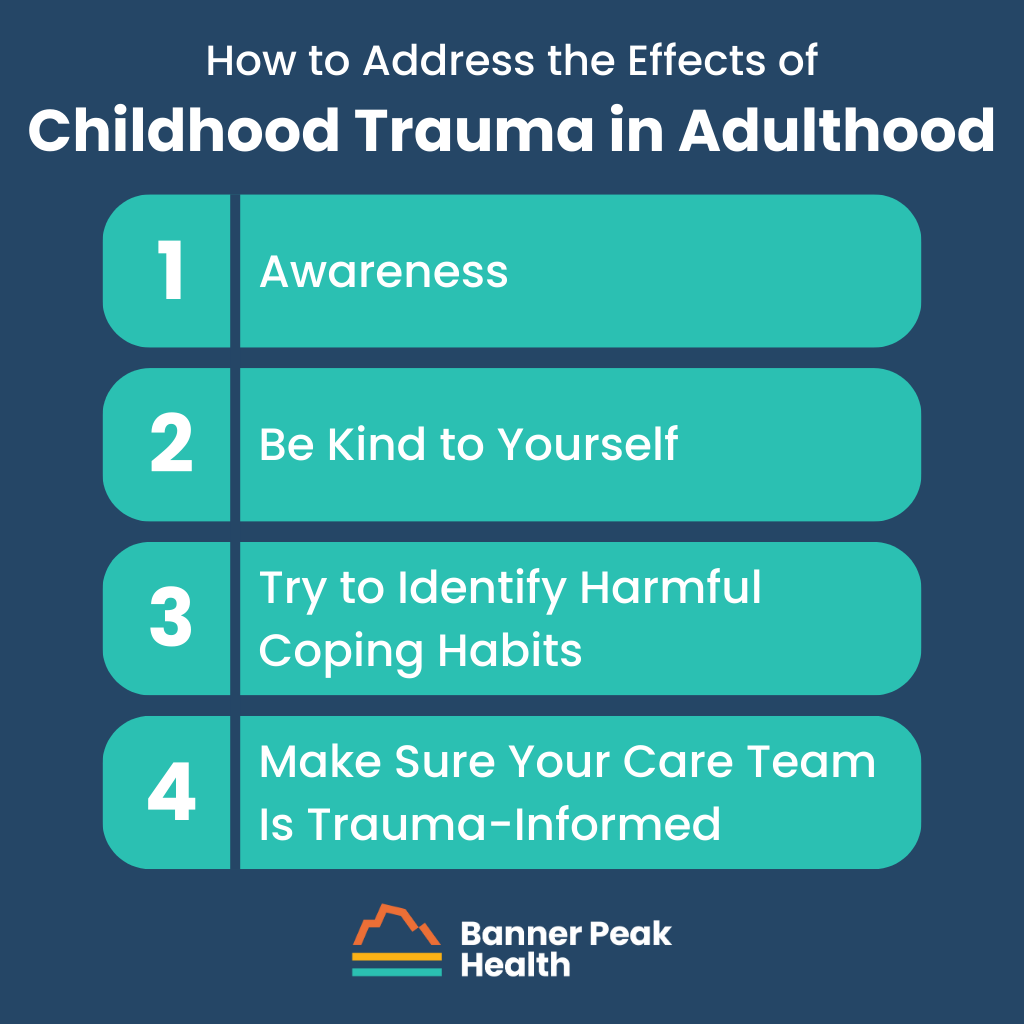
How to Address the Effects of Childhood Trauma in Adulthood
Ready to address the effects of childhood trauma in adulthood? Here are four steps we recommend to get started.
Step 1: Awareness
Many journeys of recovery begin with a step of admission or acceptance. This one is no different.
You must admit the possibility that what you’re experiencing is real. It’s not just “in your head.” It’s programmed into your nervous system.
Unfortunately, many doctors tell adult victims of childhood trauma that their symptoms are all in their heads or just a result of anxiety or depression. But anxiety is a symptom, not a disease, and it’s likely a reaction to pain that has been inflicted but hasn’t been appropriately processed.
Step 2: Be Kind to Yourself
Understand that your body was and is trying to help you survive — and you did. Your body isn’t against you. It protected you in extraordinary ways.
Trauma is not the event; trauma is the response to the event. Overcoming trauma is not about removing the event. You can’t undo the past.
Trauma is part of our survival response. It’s extraordinary the way the human body stores information with the understanding that it will be processed later, when it’s safe to do so. When we see it this way, we empower ourselves to change our perspective from weakness to strength.
Honor your authentic self. You survived.
Step 3: Try to Identify Harmful Coping Habits
Healing from trauma isn’t easy; sometimes, we reach for things that aren’t in our best interests. Identify unhealthy habits and either reduce, quit, or ask for help to quit.
It can be helpful to find an alternative (healthy) coping mechanism to turn to when you feel triggered or stressed.
Step 4: Make Sure Your Care Team Is Trauma-Informed
As doctors, our standard training does not make us trauma-informed. That leaves the onus on you to find medical professionals who are trauma-informed.
When you’ve experienced the effects of childhood trauma in adulthood or are processing those effects, you need a trauma-informed care team.
If you’d like help finding a trauma-informed care team or want to know more about becoming a member here at Banner Peak Health, reach out. We’d be happy to speak with you.

Waheeda Hiller, MD
For over 20 years in Internal Medicine, Dr. Hiller has dedicated herself to providing unparalleled care to patients. She joined Banner Peak Health in 2023 as a concierge physician to better serve patients with the depth of thought, knowledge, and compassionate care they need to live the healthiest lives possible.