Female patients in their forties often ask me about treatments for menopausal symptoms. When I mention hormone replacement therapy (HRT), some of them get nervous.
Because of outdated and since-debunked research, HRT has developed a stigma. Today, I’m debunking the most common misconceptions about HRT and perimenopause, including when to start HRT for perimenopause (as soon as you experience symptoms) and whether HRT is safe and effective (for many women, it is).
Understanding Perimenopause: A Process, Not an Event
While the average age for menopause in the United States is 51 (defined as going 12 months without a period), the journey to get there — known as perimenopause — can begin up to a decade earlier.
(Interestingly, there’s often a strong correlation between when a woman experiences menopause and when her mother did, suggesting the timing has a genetic component.)
Perimenopause isn’t a single event. It’s a gradual process that lasts several years. During this time, different symptoms may emerge, with sleep disruption often being the first noticeable sign. This is followed by what we call vasomotor symptoms: hot flashes, night sweats, and heart palpitations.
Many women also experience mood changes, including increased irritability and sometimes depressed mood.
Physical changes can include vaginal dryness and more frequent urinary tract infections. Some women also report cognitive changes, often described as “brain fog.”
Benefits of Starting HRT During Perimenopause
HRT has emerged as one of the most effective treatments for perimenopausal symptoms, particularly for managing vasomotor symptoms. Because of outdated research, most women don’t know this.
In 2002, a series of clinical trials called the Women’s Health Initiative (WHI) suggested that HRT use is associated with high risks of stroke and breast cancer. Instead of asking when to start HRT for perimenopause, women asked when to end HRT for perimenopause. Many women discontinued treatment.
However, subsequent research has largely debunked these findings, and we now have a stronger understanding of HRT’s safety profile and benefits.
When started during perimenopause, HRT offers several benefits. It can reduce the risk of depression, even in women who aren’t experiencing mood changes, and may decrease the risk of coronary artery disease when started close to menopause.
HRT has also shown promise in preventing cognitive decline and protecting the bones, reducing the risk of osteoporosis. Additionally, it helps manage genitourinary symptoms (vaginal dryness and more frequent UTIs) that can occur before menopause.
Is HRT Right for You?
Before asking your healthcare provider when to start HRT for perimenopause, consider your personal and family health history.
If you have a history of stroke, breast cancer, endometrial cancer, or ovarian cancer, avoid HRT. The same applies to those with blood clots, clotting disorders, or poorly controlled blood pressure. If blood clots are your only concern, transdermal estrogen might be an option, as it carries a lower clotting risk than oral estrogen.
Some relative contraindications include advanced liver disease and heavy or irregular bleeding during perimenopause. It’s also important to note that HRT isn’t a reliable birth control option, so if you still need contraception, consider other options.
Treatment Options
HRT isn’t one-size-fits-all. The treatment comes in different forms, including oral medications, transdermal patches, topical creams, and combinations through compounding pharmacies.
For women with an intact uterus, HRT typically includes both estrogen and progesterone, while those who’ve had a hysterectomy usually only need estrogen. Women with a progesterone IUD may not need additional progesterone in their HRT.
Testosterone therapy can be particularly helpful for specific perimenopausal symptoms, especially decreased libido and cognitive issues (brain fog, difficulty remembering names, etc.).
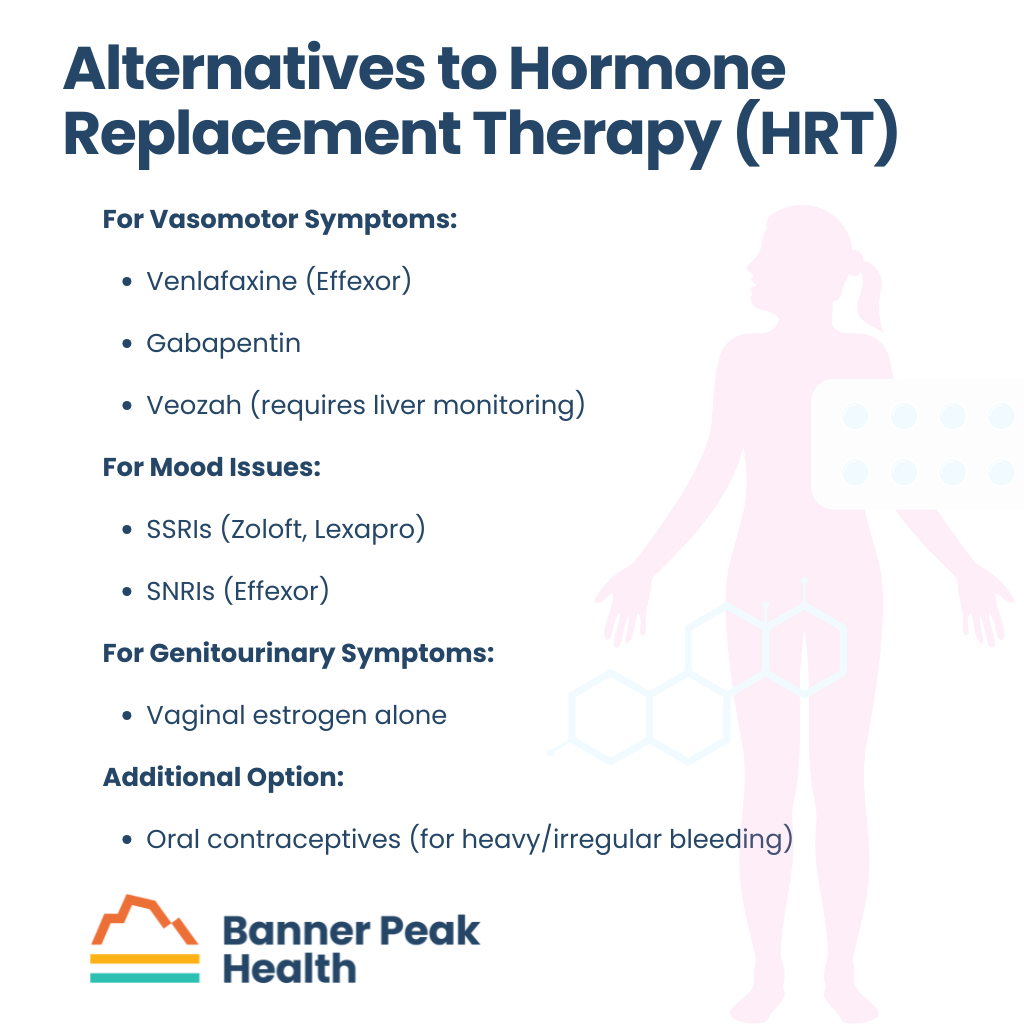 Alternatives to HRT
Alternatives to HRT
For women who can’t or choose not to use HRT, several alternatives exist.
You might manage vasomotor symptoms with medications like venlafaxine (Effexor) or gabapentin. A newer option, Veozah, is available but requires careful liver function monitoring.
You may address mood issues with SSRIs like Zoloft or Lexapro, or SNRIs like Effexor. For genitourinary symptoms, vaginal estrogen alone may be sufficient.
Some doctors might recommend oral contraceptives instead of HRT, particularly for women who experience heavy, irregular bleeding or who need contraception. While these contain higher doses of estrogen than typical HRT, they can manage certain symptoms.
Insurance and Access
Insurance coverage for HRT varies.
Insurance often covers common forms like estrogen sprays, oral progesterone, estrogen patches, and vaginal estrogen formulations, though out-of-pocket costs can still be significant. Coverage for compounded formulations is less common, but may be possible with proper documentation of medical necessity.
When to Start HRT for Perimenopause
Decide when to start HRT for perimenopause based on your symptoms and medical history.
Don’t wait until symptoms become severe or hurt your quality of life. If you think you might be experiencing perimenopausal symptoms, schedule a conversation with your healthcare provider to discuss whether HRT might be right for you.
Here at Banner Peak Health in Walnut Creek, I customize HRT treatment to each woman’s needs and preferences, whether that means choosing pills, patches, or creams. What works best for one woman may not be ideal for another, and finding the right combination often involves some trial and error.
If you’d like to explore your HRT treatment options or discuss when to start HRT for perimenopause, reach out today to schedule an appointment at our Walnut Creek office. I’m happy to chat.

Lindsay Klein, MD
After years of feeling constrained by traditional medicine's time pressures and administrative demands, Dr. Klein joined Banner Peak Health to return to her original calling: building meaningful relationships with patients and providing truly individualized care.